Abstract
The present study aimed to elucidate the antinociceptive and anti-inflammatory properties of the methanol extract from the mycelium of the endophytic fungus Rhizoctonia sp. (MEMRh) in mice. The antinociceptive activity was assessed using the abdominal constriction, hot plate, and formalin tests. The anti-inflammatory activity was assessed using a murine model of paw edema. Intraperitoneal administration of MEMRh (0.1, 1, 10 and 100 mg/kg, i.p.) produced an inhibition of acetic acid-induced writhing in mice for at least 8 h. In addition, all doses tested of the methanol extract were able to prevent thermal nociception in the hot-plate test. Furthermore, treatment with MEMRh (10 mg/kg, i.p.) inhibited both the early and late phases of formalin-induced nociception. This antinociceptive effect exhibited by MEMRh in the formalin test was reversed by the systemic administration of naloxone. MEMRh produced inhibition in a carrageenan-induced edema model at a dose of 10 mg/kg. The same extract also displayed significant activity against a histamine- or PGE2-induced edema model. The experimental data demonstrated that MEMRh showed remarkable anti-inflammatory and antinociceptive activities. Further studies are warranted to define and isolate the active anti-inflammatory and antinociceptive components from this endophytic fungus, which may yield effective agents for the treatment of inflammatory disorders.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The presence of endophytes brings many advantages to the host plant, including the ability to produce antibiotics and other secondary metabolites of pharmacological interest and use as biological control agents [1]. The prospect that endophytes produce novel bioactive products stems from the idea that some endophytes may have coevolved with their respective higher plant, and as a result may produce certain metabolites characteristic of their hosts [2]. On the other hand, endophytes may produce useful compounds unique to them [3].
The discovery that an endophytic fungus (Taxomyces andreanae) also produced the anticancer drug paclitaxel (Taxol®) derived from Pacific yew (Taxus brevifolia) was unexpected [4]. Moreover, several studies indicate that endophytic fungi isolated from medicinal plants have the ability to produce secondary metabolites of interest against cancer, sepsis and malaria [5–7]. Thus, these observations stimulated the opening of a fascinating area of research in microbiology where there is only fragmented information on endophytes. Studies on endophytic fungi are therefore of great value to ecology and pharmacology. For instance, the mycelia of fungi of the genus Rhizoctonia are able to produce a large series of secondary metabolites with interesting biological activities, such as the three dioxopiperazines [8], and phenylacetic acid and derivatives are found in the culture filtrate of R. solani [9] and the two benzophenone derivatives active against Helicobacter pilori in Rhizoctonia sp. as an endophyte of Cynodon dactylon [10].
Schinus terebinthifolius Raddi, popularly called Brazilian pepper, is a tree species belonging to the family Anacardiaceae, which is used in popular medicine as a remedy for wounds and respiratory problems [11]. Moreover, extracts of the leaves, seeds or stem barks from Schinus terebinthifolius have biological effects of interest in animal models, including anti-allergic effects [12] and healing of surgical wounds in the bladder [13]. Interestingly, the presence of endophytic fungi in trees of the genus Schinus has been reported [14].
Thus, the current study was undertaken to assess the analgesic and anti-inflammatory action of the methanol extract from the mycelium of Rhizoctonia sp. fungus (MEMRh) isolated as an endophyte from Schinus terebinthifolius seeds.
Materials and methods
Fungus material and extract preparation
Rhizoctonia sp. was isolated as an endophytic fungus on healthy seeds of Schinus terebinthifolius Raddi collected from the Universidade Federal de Alagoas Arboretum and was identified by morphological and rDNA analyses, as described elsewhere [15].
Rhizoctonia sp. culture was maintained in PDA medium on petri dishes at 26 ± 2°C, under continuous light. Liquid cultures were obtained by cutting plugs of mycelium (7 mm diameter) from the edges of 5-day-old cultures and placing them in PDB medium (1 plug per 100 ml medium into 250 ml Erlenmeyer flasks) on orbital shakers at 200 rpm. The mycelium biomass that had grown for 15 days was filtered and dried and the crushed mycelium (50 g) was extracted with methanol (3 × 200 mL). After filtration, the methanol solution was evaporated in a rotary evaporator under reduced pressure, yielding 14.66 g. At the time of use, the extract was reconstituted in saline (NaCl 0.9%) at the required concentrations.
Animals
Male Swiss mice weighing 18–22 g were obtained from the Universidade Federal de Alagoas breeding unit. The animals were maintained with free access to food and water and kept at 22 ± 2°C with a controlled 12 h light–dark cycle at Instituto de Ciências Biológicas e da Saúde. Experiments were performed during the light phase of the cycle. The animals were allowed to adapt to the laboratory for at least 2 h before testing and used only once. All experiments were carried out in accordance with institutional guidelines and ethics (License no. 23065.12614/2006-89).
Abdominal writhing test
The writhing test was carried out according to the method previously described by Collier et al. [16]. Abdominal writhing in mice was caused by the intraperitoneal (i.p.) injection of 0.6% acetic acid, 0.1 ml/10 g body weight. Control animals received the same volume of saline (NaCl 0.9%). The animals were previously treated via the i.p. route with different doses of MEMRh (0.1, 1, 10 and 100 mg/kg body weight) 1 h before stimulation with acetic acid. Control animals received the same volume of vehicle (saline). Five minutes after the acetic acid injection, the number of times that each animal presented abdominal constriction was counted for 10 consecutive minutes. Indomethacin (10 mg/kg, p.o.) was used as the standard drug for comparison. Each experimental group contained at least six animals.
Hot-plate test
The hot-plate test was used to measure reaction times according to the method described by Eddy and Leimback [17]. Mice were placed individually on a hot-plate metallic surface (Insight®, Brazil; model EFF-361) maintained at 54 ± 1°C, and the time between placement of the animal on the hot-plate and the occurrence of either licking of the hind paws, shaking or jumping off the surface was recorded as reaction time (s). Reaction time was measured at 60 min following treatment with saline (i.p.), of MEMRh (1, 10 and 100 mg/kg, i.p.) or morphine (5 mg/kg, i.p.), with a cut-off time of 30 s. Each experimental group contained at least six animals.
Formalin test
Formalin-induced paw-licking was determined essentially as described by Murray et al. [18]. Mice were injected with formalin (2.5%, 20 μl) in the subplantar area of the right hind paw. The duration of paw licking, an index of nociception, was measured from 0 to 5 min (early phase) and from 15 to 30 min (late phase) after formalin administration. Animals were treated with MEMRh (10 mg/kg, i.p.) 1 h before intraplantar injection of the stimulus. Each experimental group contained at least six animals. In some experiments, naloxone (5 mg/kg, i.p.), was administered 30 min before MEMRh in order to investigate putative opioid-like activity of the extract.
Induction of acute inflammation in mice hind paws by phlogistic agents
Acute inflammation in the hind paws of mice was induced by subcutaneous injection of 0.05 ml of 1% freshly prepared solutions of carrageenan (300 μg/paw), histamine (100 μg/paw) or PGE2 (100 ng/paw) into right hind paws of mice. The left hind paws were injected with saline (NaCl 0.9%) and used as controls. The inflammation was quantified by measuring the volume displaced by the paw, using a plethysmometer (PanLab, Italy) at different times after stimulations. Mice paw edema was measured by plethysmography at 0, 1, 2, 3 and 4 h after carrageenan or 1 h after histamine and PGE2 intraplantar injection. Administration of MEMRh (10 mg/kg, i.p.), indomethacin (10 mg/kg, i.p.) or promethazine (5 mg/kg, i.p.) was conducted 1 h prior to the inflammatory stimulation. Results were expressed as the difference in volume between the carrageenan-injected and the saline-injected paws [Δ paw volume (μL)].
Statistical analysis
The data were expressed as mean ± standard error of mean (SEM). The statistical analysis involving two groups was carried out using Student’s t test. ANOVA followed by Student–Neuman–Keuls test was used to compare three or more groups. P values of 0.05 or less were considered significant.
Results
Antinociceptive activity
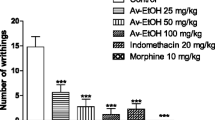
After intraperitoneal injection of acetic acid in mice, 30.6 ± 9.1 writhings were observed in a period of 10 min. Pre-treatment with increasing doses (0.1–100 mg/kg) of MEMRh showed that there is an inhibitory effect in all doses assayed. The dose–response curve did not show a difference between doses, suggesting that this fraction could be in its maximal effect (Fig. 1).
Effects of the MEMRh on acetic acid-induced writhing response in mice. The number of writhes in 10 min was measured after acetic acid injection. Indomethacin (10 mg/kg, i.p.) was used as a positive control. The values are expressed as the mean ± SEM (n = 6). **P < 0.01 and ***P < 0.001 indicate statistically significant differences from the saline-treated group
We also evaluated the duration of the analgesic effect of MEMRh in the acetic acid-induced abdominal constriction model. In this case, five different groups of mice were pre-treated with MEMRh (10 mg/kg, i.p.) at 30, 60, 120, 240 or 480 min before acetic acid injection. As shown in Fig. 2, treatment with MEMRh showed a maximum antinociceptive effect at 30 min which remained until at least 120 min after i.p. injection of MEMRh. At 8 h after pain stimulus, MEMRh was still able to display an antinociceptive effect.
Time response curve for the analgesic effect of MEMRh on acetic acid-induced writhing response in mice. Writhings were counted over 10 min following i.p. injection of acetic acid. MEMRh (10 mg/kg) was administered i.p. 30, 60, 120, 240 or 480 min before acid acetic injection (0.6%). Control animals received an i.p. injection of the vehicle. Each bar is the mean ± SEM (n = 6). **P < 0.01 and ***P < 0.001 indicate statistically significant differences from the saline-treated group
As shown in Table 1, MEMRh administered at doses of 1, 10 and 100 mg/kg exerted a significant increase in response latency against thermal stimulus-induced nociception compared to control.
Figure 3 shows the results obtained with the formalin test. Treatment of mice with MEMRh (10 mg/kg i.p.) resulted in a significant inhibition of formalin-induced licking in the first phase (neurogenic pain) and the second phase (inflammatory pain) of the formalin test. Pre-treatment with a non-selective opioid receptor antagonist (naloxone 5 mg/kg) significantly reversed the antinociceptive effect of MEMRh in both phases of the formalin test. The reference drug, morphine (5 mg/kg, i.p.), significantly reduced paw licking time in both phases when compared to the saline-treated animals and such action was completely reversed by naloxone.
Effect of treatment with MEMRh on nociception induced by formalin. The licking time was determined during the first 5 min (1st phase; a), and during 15–30 min (2nd phase; b) after 2.5% formalin injection in mice. 60 min before formalin, mice received i.p. saline or MEMRh (10 mg/kg). Another group of animals was pretreated with naloxone (5 mg/kg, i.p.) 15 min before morphine (5 mg/kg, i.p.) or MEMRh (10 mg/kg). Data are expressed as mean ± SEM (n = 6). ***P < 0.001 compared to respective saline-treated group
Anti-inflammatory activity
The inhibitory effects of MEMRh in the second phase of the formalin model (the inflammatory phase) led us to test it on mice paw edema induced by carrageenan, histamine or PGE2. As shown in Fig. 4, a single treatment of mice with MEMRh (10 mg/kg, i.p., 1 h) was capable of reducing the edema induced by carrageenan (300 μg/paw), an effect observed at 60, 120 and 240 min after the administration of this phlogistic agent. Likewise, indomethacin (10 mg/kg, i.p., 1 h) also significantly inhibited the edematogenic response evoked by carrageenan in mice, at the 2nd, 3rd and 4th time points (Fig. 4).
To evaluate whether the fraction was also able to inhibit the edema induced by mediators involved in inflammation, mice were pre-treated with the fraction and then received an intraplantar injection of histamine or PGE2. MEMRh (50 mg/kg, i.p.) significantly diminished the edema induced by histamine (100 μg/paw) or PGE2 (100 ng/paw) (Table 2). Indomethacin or promethazine were able to reduce, in a significant manner, the mouse paw edema induced by histamine and PGE2 in mice, respectively (Table 2).
Discussion
Endophytic microorganisms that reside in the tissues of living plants are relatively little studied and are potential sources of novel natural products for exploitation in medicine, agriculture, and industry. These organisms are of biotechnological importance as new pharmaceutical compounds, secondary metabolites, and agents of biological control, and other useful characteristics could be found by further exploration of endophytes. Therefore, the use of endophytic fungi opens up new areas of biotechnological exploitation, which leads to the necessity of isolating and cultivating these organisms. There have been some studies on detecting biological activities, including anti-inflammatory effects, of fungal endophytes from medicinal plants [19–21].
The present study proposed to evaluate the analgesic and anti-inflammatory action of MEMRh (methanol extract from the mycelium of Rhizoctonia sp. endophytic fungus of Schinus terebinthifolius seeds). This is the first time that a methanol extract of Rhizoctonia sp. has been described as an analgesic and anti-inflammatory.
Initially, we used the acetic acid-induced writhing test to assess antinociceptive activity of the methanol extract. This test is a typical model for inflammatory pain and has long been widely used as a model for the evaluation of analgesic and anti-inflammatory properties of new agents [16]. The intraperitoneal administration of the methanol extract produced a significant inhibition in the nociceptive response, in all doses tested, when assessed by the writhing test in mice. Several mechanisms of action may be suggested to explain the observed antinociceptive activity of MEMRh, particularly the activity assessed with the writhing test. The antinociceptive activity seen could be due in part to inhibition of the release of inflammatory mediators or blockade of peripheral cyclooxygenase activity [22]. Despite being claimed as a highly sensitive and useful model for analgesic drug development, this model of visceral pain is not a selective pain test [23]. In this model, the acetic acid acts indirectly by inducing the release of endogenous mediators, which stimulate the nociceptive neurons that are sensitive to non-steroidal anti-inflammatory drugs and narcotics [16]. Thus, several other methods were used to clarify the mechanism(s) involved in the present study, including the hot-plate test and formalin-induced paw licking test.
The hot-plate test is a selective model for studying the central but not peripheral analgesic properties of compounds, because heat stimulation sensitizes peripheral nerve endings and the impulses generated transmit by way of the spinal cord to the brain. This assay is widely used to screen potential substances or centrally acting opiate analgesic drugs that inhibit pain of central origin [23]. The present findings confirmed the central antinociceptive effect of the methanol extract as evidenced by the increase in reaction time of mice in the hot-plate test.
To better clarify the results obtained in this study, the antinociceptive effect of MEMRh was confirmed in the formalin test, a model of inflammatory pain which has two distinctive phases that may indicate different types of pain [24]. The early and late phases of the formalin test have obviously different properties, and therefore this test is useful not only for assessing the analgesic substance, but also for elucidating the mechanism of analgesia [25]. The early phase, named non-inflammatory or neurogenic pain, is a result of direct stimulation of nociceptors and reflects centrally mediated pain; the late phase, named inflammatory pain, is caused by local inflammation with a release of inflammatory and hyperalgesic mediators [24].
In the present study, MEMRh administration induced antinociceptive activity in both the early and late phases of the formalin test. Similarly, morphine produced marked inhibition of both the early and late phases in this test. It is also interesting to note that pretreatment with naloxone significantly reversed the antinociceptive effect of the methanol extract and morphine in both phases of the formalin test, compared to methanol extract and morphine alone. Based on the findings of both the hot-plate and the formalin tests, MEMRh seems to possess significant central and peripheral antinociceptive mechanisms that are partly mediated by the activation of opioid systems.
In order to evaluate the anti-inflammatory activity of MEMRh, we used the mice paw edema model. Carrageenan-induced paw edema as an in-vivo model of inflammation has been frequently used to assess the anti-edematous effect of natural products. It has been reported that various mediators are released by carrageenan in the mouse paw; thus, while the initial phase may be due to the release of histamine, the second phase is attributed to the release of prostaglandins and is sensitive to most clinically effective anti-inflammatory drugs [26].
Our results indicate that the inhibitory effect of MEMRh on carrageenan-induced edema is probably due to histamine reduction, since it was able to inhibit the edema induced by this mediator. We can also speculate that part of the anti-edematogenic effect of the methanol extract is due to prostaglandin liberation, since its effect on carrageenan-induced edema was more pronounced than that produced by histamine. It has been well characterized that carrageenan-induced paw edema is associated with the rapid production of several inflammatory mediators such as histamine and prostaglandins, among others [27, 28]. Therefore, we propose that the anti-edematogenic effects observed with the methanol extract are related to interference with one or more of these pathways. In fact, MEMRh has been found to markedly reduce the edema formation induced by both histamine and PGE2 in mice, suggesting that these compounds probably act through distinct mechanisms.
Based on our results, we propose that MEMRh exerts significant peripheral and central antinociceptive effects, probably mediated by activation of the opioidergic mechanism. Furthermore, the extract was able to suppress inflammation induced by phlogistic agents, confirming its analgesic and anti-inflammatory activities. The results indicate that bioactive metabolites from endophytes could be useful sources for research and development of bioactive leader compounds from nature, being sources of molecules for the management of pain and inflammatory disorders. Studies are currently underway to determine the active compounds present in MEMRh and also to characterize the possible mechanisms of action that cause the biological effects detected.
References
Basile A, Giordano S, Lopez-Saez JA, Cobianchi RC (1999) Antibacterial activity of pure flavonoids isolated from mosses. Phytochemistry 52:1479–1482
Strobel GA, Daisy B (2003) Bioprospecting for microbial endophytes and their natural products. Microbiol Mol Biol Rev 67:491–502
Tan R, Zou W (2001) Endophytes: a rich source of functional metabolites. Nat Prod Rep 18:448–459
Stierle A, Strobel G, Stierle D, Grothaus P, Bignami G (1995) The search for a taxol-producing microorganism among the endophytic fungi of the pacific yew, Taxus brevifolia. J Nat Prod 58:1315–1324
Wiyakrutta S, Sriubolmas N, Panphut W, Thongon N, Danwisetkanjana K, Ruangrungsi N, Vithaya M (2004) Endophytic fungi with anti-microbial, anti-cancer and anti-malarial activities isolated from Thai medicinal plants. World J Microbiol Biotechnol 20:265–272
Cota BB, Rosa LH, Caligiorne RB, Rabello AL, Almeida-Alves TM, Rosa CA, Zani CL (2008) Altenusin a biphenyl isolated from the endophytic fungus Alternaria sp., inhibits trypanothione reductase from Trypanosoma cruzi. FEMS Microbiol Lett 285:177–182
Wang FW, Ye YH, Chen JR, Wang XT, Zhu HL, Song YC, Tan RX (2006) Neoplaether, a newcytotoxic and antifungal endophyte metabolite from Neoplaconema napellum IFB-E016. FEMS Microbiol Lett 261:218–223
Pedras MS, Yu Y, Liu J, Tandron-Moya YA (2005) Metabolites produced by the phytopathogenic fungus Rhizoctonia solani: isolation, chemical structure determination, syntheses and bioactivity. Z Naturforsch C 60:717–722
Aoki H, Sassa T, Tamura T (1963) Phytotoxic metabolites of Rhizoctonia solani. Nature 200(490):575
Ma YM, Li Y, Liu JY, Song YC, Tan RX (2004) Anti-Helicobacter pylori metabolites from Rhizoctonia sp. Cy064, an endophytic fungus in Cynodon dactylon. Fitoterapia 75:451–456
Bendaoud H, Romdhane M, Souchard JP, Cazaux S, Bouajila J (2010) Chemical composition and anticancer and antioxidant activities of Schinus molle L. and Schinus terebinthifolius Raddi berries essential oils. J Food Sci 75:C466–C472
Cavalher-Machado SC, Rosas EC, Brito FA, Heringe AP, Oliveira RR, Kaplan MAC, Figueiredo MR, Henriques MGMO (2008) The anti-allergic activity of the acetate fraction of Schinus terebinthifolius leaves in IgE induced mice paw edema and pleurisy. Int Immunopharmacol 8:1552–1560
Lucena PLH, Ribas-Filho JM, Mazza M, Czeczko NG, Dietz UA, Correa Neto MA, Henriques GS, Santos OJ, Ceschin AP, Thiele ES (2006) Avaliação da ação da aroeira (Schinus terebinthifolius Raddi) na cicatrização de feridas cirúrgicas em bexiga de ratos. Acta Cir Bras 21:44–49
Aziz T, Sylvia DM, Doren RF (1995) Activity and species composition of arbuscular mycorrhizal fungi following soil removal. Ecol Appl 5:776–784
Albuquerque ED (2007) Rhizoctonia sp, endofítico de sementes de Schinus terebenthifolius Raddi: Análise química e bioatividade de seus extratos, pp 23–60. Mestrado em Produção Vegetal. Centro de Ciências Agrárias, Universidade Federal de Alagoas, Alagoas, Brasil
Collier HO, Dinneen LC, Johnson CA, Schneider C (1968) The abdominal constriction response and its suppression by analgesic drugs in the mouse. Br J Pharmacol Chemother 32:295–310
Eddy NB, Leimbach D (1953) Synthetic analgesics II. Dithienylbutenyl- and dithienylbutylamines. J Pharmacol Exp Ther 107:385–393
Murray CW, Porreca F, Cowan A (1988) Methodological refinements to the mouse paw formalin test. An animal model of tonic pain. J Pharmacol Methods 20:175–186
Weber D, Sterner O, Anke T, Gorzalczancy S, Martino V, Acevedo C (2004) Phomol a new anti-inflammatory metabolite from an endophyte of the medicinal plant Erythrina crista-galli. J Antibiot 57:559–563
Deshmukh SK, Mishra PD, Kulkarni-Almeida A, Verekar S, Sahoo MR, Periyasamy G, Goswami H, Khanna A, Balakrishnan A, Vishwakarma R (2009) Anti-Inflammatory and anticancer activity of ergoflavin isolated from an endophytic fungus. Chem Biodivers 6:784–789
Xu L, Zhou L, Zhao J, Li J, Li X, Wang J (2008) Fungal endophytes from Dioscorea zingiberensis rhizomes and their antibacterial activity. Lett Appl Microbiol 46:68–72
Zakaria ZA, Sulaiman MR, Morsid NA, Aris A, Zainal H, Pojan NH, Kumar GH (2009) Antinociceptive, anti-inflammatory and antipyretic effects of Solanum nigrum aqueous extract in animal models. Methods Find Exp Clin Pharmacol 31:81–88
Le Bars DL, Gozariu M, Cadden SW (2001) Animal models of nociception. Pharmacol Rev 53:597–652
Hunskaar S, Hole K (1987) The formalin test in mice: dissociation between inflammatory and non-inflammatory pain. Pain 30:103–114
Shibata M, Ohkubo T, Takahaski H, Inoki R (1989) Modified formalin test: characteristic biphasic pain response. Pain 38:347–352
Fernandes ES, Passos GF, Medeiros R, Cunha FM, Ferreira J, Campos MM, Pianowski LF, Calixto JB (2007) Anti-inflammatory effects of compounds alpha-humulene and (−)-trans-caryophyllene isolated from the essential oil of Cordia verbenacea. Eur J Pharmacol 569:228–236
Posadas I, Bucci M, Roviezzo F, Rossi A, Parente L, Sautebin L, Cirino G (2004) Carrageenan-induced mouse paw oedema is biphasic, age-weight dependent and displays differential nitric oxide cyclooxygenase-2 expression. Br J Pharmacol 142:331–338
Di Rosa M, Giroud JP, Willoughby DA (1971) Studies on the mediators of the acute inflammatory response induced in rats in different sites by carrageenan and turpentine. J Pathol 104:15–29
Acknowledgments
This work was supported by grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), the Programa de Cooperação Acadêmica/Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (PROCAD/CAPES) and the Fundação de Amparo à Pesquisa do Estado de Alagoas (FAPEAL) (Brazil).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Barros, B.S., da Silva, J.P., de Souza Ferro, J.N. et al. Methanol extract from mycelium of endophytic fungus Rhizoctonia sp. induces antinociceptive and anti-inflammatory activities in mice. J Nat Med 65, 526–531 (2011). https://doi.org/10.1007/s11418-011-0534-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-011-0534-x