Abstract
This paper analyzes the impact of mental health treatment on suicide attempts. While prior work demonstrates the effectiveness of mental health treatment at reducing suicide risk, few studies examine nationally representative populations or use broad measures of access to mental health services. A methodological problem can arise in studies of mental health treatment and suicidal behavior because a suicide attempt can result in the use of more mental health services. Using nationally representative survey data combined with national estimates of provider availability, this paper employs a methodological correction to address that potential problem of reverse causation. This paper uses measures of the density of health care providers in an area as statistical instruments for use of mental health treatment in an analysis of the impact of mental health treatment on suicide attempts. This study finds that mental health treatment significantly reduces suicide attempts.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Suicide poses a significant public health problem in the USA. In 2015, suicide was the tenth leading cause of preventable death with 44,193 individuals dying by suicide.1 Additionally, while preventable mortality from many other causes has been declining in recent years, deaths by suicide have been increasing.2 From 1999 to 2014, suicide rates increased 24%, from 10.5 per 100,000 people to 13 per 100,000 people.3 In addition to lives lost, suicide results in large economic costs, estimated at over $93 billion per year.4 As a result, reducing suicide has become a top priority for patients, providers, payers, policy makers, and advocates.5
Mental health treatment for those at risk of suicide is an important part of suicide prevention. Over 90% of suicide victims have at least one psychiatric disorder.6 Antidepressant prescriptions are correlated with lower suicide rates,7, 8 and other forms of therapy, such as cognitive therapy and interpersonal psychotherapy, have been shown to reduce suicidal behavior.9,10,11 Most suicide victims have some contact with medical providers within a month of death, and approximately one-third have contact with a mental health provider.12 However, there is opportunity for individuals at risk for suicide to receive more treatment.13
Research has shown that mental health treatment utilization among individuals with risk of suicidal behavior is very low and a significant proportion of these individuals report lack of treatment access as a primary reason for not obtaining care.14 This is a concern, given research has shown a reduction in risk of suicide following mental health treatment.15 The literature has also documented evidence of the challenges related to continued receipt of mental health services.16 However, this literature has been limited either to a select population, for example veterans17 or limited to a few treatment centers.16 Very few studies have investigated the impact of mental health treatment in reducing risk of suicide among a nationally representative sample of the population.14 Additional research examines the relationship between physician density and suicide rates among adolescents and young adults in European countries.18 This work, however, has several limitations. First, it examines general physician density, not behavioral health specialists. Next, it is unable to estimate the impact of physician density on probability of receiving treatment. Finally, it is unable to control for a wide variety of potential cofounders.
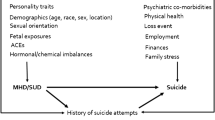
A number of factors complicate the accurate identification of the effect of mental health treatment on suicide attempts. Underlying mental health conditions can drive the decision to attempt suicide, as well as the decision to seek mental health treatment. Also, uncompleted suicide attempts can result in increases in mental health treatment. These relationships can pose an analytic problem of reverse causation, which in this context could be higher levels of suicidal behavior leading to greater use of treatment. This study addresses that potential problem by using geographic variation in the availability of mental health service providers as a statistical instrument in an analysis of the impact of mental health treatment on suicide attempts.
This study contributes to the literature in two important ways. First, it examines the impact of mental health treatment on suicide attempt among a nationally representative sample of the population using a statistical correction for reverse causation in treatment seeking behavior—something that has not been previously done in the literature. Second, the study examines the impact of mental health treatment on suicide attempt among various subgroups of the population, which have been recently identified in the literature as facing unique challenges, to determine whether the impact of mental health treatment might vary among different sub-populations.19 This is an important contribution to the literature as it quantifies the importance of mental health treatment in reducing suicide attempt on a nationally representative sample, while using an empirical strategy to overcome a methodological challenge common in this literature.
Methods
This study combines two data sources, the National Survey on Drug Use and Health (NSDUH) and the Area Health Resources File (AHRF), to estimate the effect of mental health treatment on suicide attempts. Individual’s suicide attempts and demographic characteristics are obtained from the 2008–2014 NSDUH. Conducted by the Substance Abuse and Mental Health Services Administration, the NSDUH is a nationally representative survey of the non-institutionalized population aged 12 and older and is the nation’s leading survey on mental health. As such, it is widely used to examine mental health issues. In this study, the sample is limited to those 18 and older to focus on the adult population.
The dependent variable is obtained from the question “In the past 12 months, did you try to kill yourself?” and is coded as a binary variable equal to one if the survey respondent answered “yes” and zero otherwise (i.e., whether the respondent answered “no” or was not asked the question as part of a legitimate skip pattern). The primary independent variable of interest is the receipt of mental health treatment and is defined here as whether in the past 12 months the survey respondent had received any inpatient mental health treatment (i.e., staying overnight in a hospital), any outpatient mental health treatment (i.e., treatment at an outpatient mental health clinic/center, or in the office of a private therapist, psychologist, psychiatrist, social worker, counselor, or in a doctor’s office, or in an outpatient medical clinic, or in a partial day hospital, or day treatment program), or was prescribed any psychotropic medication.
In addition to these variables, the NSDUH provides a number of control variables including gender, race, age, health insurance status, and income, which are factors that have been shown to be associated with suicidal ideation.20 The analysis also includes county level measures of the log of the population, the log of per capita income, the percent of the population with no high school education, and the unemployment rate. Using these variables, the primary specification is as follows:
where Sisy is the variable indicating whether individual i living in state s during survey year y attempted suicide, Xisy is the vector of individual and county control variables for the respondent, σ and τ are vectors of state and year fixed effects, respectively, and ϵ is the error term.
As outlined above, there is likely a relationship between suicide attempts and mental health treatment that can complicate efforts to estimate the impact of mental health treatment on suicide attempt accurately. Thus, an instrumental variable approach was utilized to identify the impact of Treatment on suicide attempts. The Health Resources & Services Administration’s (HRSA) AHRF provides an instrumental variable that plausibly does not suffer from the methodological concerns described above when conditioned on the control variables. The AHRF is a dataset that includes a wide range of information on health facilities and professionals at the county level. The AHRF provides the number of psychologists and psychiatrists for each county in the USA. The number of mental health professionals can affect the access and travel costs for mental health care21 and thus should be associated with patient propensity to receive mental health treatment. Though mental health providers may be driven to locate in areas by factors that are associated with suicide, namely, income levels, and urbanity, when conditioning on these other factors, an instrumental variable approach can still identify the effect of the mental health treatment. By controlling for the societal factors that are associated with suicide and the mental health provider’s location decision, a provider’s location decision becomes plausibly unrelated (in a statistical sense) to the respondent’s decision to attempt suicide.
To operationalize the instrument, the number of psychologists plus psychiatrists per capita for each county is calculated and then matched with the NSDUH data based on the survey respondent’s county of residence. A potential drawback to using the AHRF data is that contemporary data are matched to historic NSDUH data. While the AHRF only measures provider density for a single year, the number of psychiatrists and psychologists in a particular county remained relatively stable over the study period (for example, the correlation coefficient for the number of psychiatrists in a county in 2005 and 2013 is 0.996). To demonstrate the effect of instrumentation, the analysis was also undertaken without their use. Analysis was further conducted on the subset of survey respondents who indicated that they had an unmet need for mental health treatment.
It is possible that psychiatrists and psychologists will locate in areas with a relatively higher prevalence of behavioral health conditions. If this is the case, it could potentially bias the results of the first stage of the analysis. An alternative way to view the mechanism through which the instrument set operates is to consider probability of mental health treatment as a function of the number of physicians per capita without the limitation that they be specialty behavioral health providers. A denser concentration of providers per capita reduces the travel and access costs of obtaining health care and increases the probability of contact with medical professionals. This, in turn, would also increase the probability of receiving mental health treatment both directly as people actively seek treatment and indirectly as individuals get screened for mental health conditions during the course of general medical care. Given this mechanism, an alternative instrument set of general medical density that includes the number of primary care providers (PCP) per capita was considered along with the number of active medical doctors (MDs) per capita. The alternative instruments should be highly correlated with the number of psychiatrists and psychologists per capita, but primary care providers per capita should not be more likely to locate in areas with a relatively higher prevalence of behavioral health conditions. Thus, the alternative instrument set should not suffer from bias in the first stage that could arise with the primary instrument set.
Given the dichotomous nature of both the outcome variables, the study estimates a linear probability model (LPM) for the first stage and probit in the second stage.22 Estimates are weighted to make the results nationally representative, and standard errors are clustered at the state levels. Estimates are shown for the full population and for the subset of the population that needs mental health treatment; that is, individuals with mental health treatment and those who reported an unmet need for treatment. Additionally, the analysis is stratified along several demographic dimensions to examine potential differences in the impact of treatment.
Results
Summary statistics for the primary analysis can be found in Table 1. Approximately one-half percent of the sample attempted suicide over the study periods, while 14% received mental health treatment. Average provider densities were 33.22 per 100,000 people for psychologists; 13.22 per 100,000 for psychiatrists; 80.86 per 100,000 for PCPs; and 294.16 per 100,000 for active MDs. The sample is 48% male, 80% white, and 14% Hispanic with an average age of 46.6. Finally, 84% were covered by some sort of health insurance and incomes averaged 343% of the federal poverty level (FPL).
Table 2 presents the results of the primary instrumental variable analysis. The marginal effect of mental health treatment on the probability of suicide attempt indicates that mental health treatment is associated with a 17.7 percentage point decline in the probability of attempting suicide. This effect is robust across the instrument set, ranging from a 17.1 to a 20.4 percentage point decline in suicide attempt probabilities. First stage statistics from the linear probability model indicate the choices of instruments in the analysis are valid.
Sensitivity Analysis
Table 3 reports the results, stratified by the full population and those who need mental health treatment, for both ordinary least squares (OLS) and probit models that are non-instrumented and from the instrumental variable analysis. The non-instrumented results indicate that mental health treatment is positively correlated with suicide attempts at high levels of statistical significance for both the full population and those in need of mental health treatment. Given the discussion above about the possibility of this finding without the use of a methodological correction, this result is not surprising. As such, it provides no insight into the actual causal impact of mental health treatment on suicide attempts. However, the full population instrumental variable results show a consistent reduction in probability of suicide attempts. In addition to the results from the primary analysis using a probit second stage, results from a model using a LPM second stage showing a 4.4 percentage point decline in probability of suicide attempts with mental health treatment. For those who need mental health treatment, there is also reduction in the probability of suicide attempt.
Robustness Check and Sub-populations
Table 4 presents results from the alternative instrument set, general medical provider density. Depending on the instrument specification, these results indicate mental health treatment reduces suicide attempts by approximately 12.4 to 21.3 percentage points (marginal effects for PCPs per capita and active MDs per capita specifications, respectively). These results are in line with the main results; however, given the more intuitive relationship between probability of treatment and mental health infrastructure density, mental health professionals per capita remain the preferred instrument set.
Table 5 presents results for several sub-populations from the preferred specification. These results indicate that the effects shown in the primary analysis seem to be driven by females, individuals not aged 25–54, and non-blacks. Additionally, the effects seem to be concentrated in more metropolitan counties, likely due to the higher provider densities and better access to treatment available in urban areas.
Implications for Behavioral Health
Greater access to mental health treatment, as measured by mental health provider density, is associated with more mental health treatment, which, in turn, significantly reduces suicide attempts. The gains in suicide prevention are concentrated among individuals who are young, white, and female. These results affirm that mental health treatment is an important protective factor for suicide.
Higher densities of behavioral health providers imply a lower opportunity cost of seeking and receiving treatment for those at risk of suicide. While the rate of active MDs is closely associated with behavioral health provider density, it is not directly related to receipt of behavioral health treatment. The broader measures of provider density affect the suicide rate only to the extent they are related to higher behavioral health provider density or that greater mental health screening occurs during general care visits. Therefore, the density of behavioral health providers will have a greater effect on suicide rates than more general measures of the number of doctors per capita in the area. Also, more provider availability might attenuate the role of stigma as a barrier in accessing mental health care. That this is observed in the results suggests that these measures are capturing the effects of greater access to behavioral health services and are not a spurious correlation.
However, these results should be considered in light of some limitations of the study design. First, the underlying assumptions of the instrumental variable approach cannot be directly tested. Any violation of the assumption would result in biased estimates, and while controls are included for a number of potential paths by which provider density and suicide rates may be related, it is impossible to fully rule out a relationship between the two. Next, the mental health provider data is only a snapshot of an area’s providers, which are then paired with both contemporary and historical data. While it is a reasonable assumption that provider availability does not drastically change over time, this matching might introduce error into the results. To the extent that the mismatching is random (as provider entry and exits from the market are likely to be), this would have the effect of attenuating the precision of the results but does not bias them. Finally, the analysis considers a broad measure of mental health treatment and could not investigate which types of treatment or the type of provider (psychiatrist, psychologist, clinical social worker etc.) are most effective at reducing suicide risks.
A number of interventions focusing on limiting the immediate means by which people commit suicide have been shown to be effective in reducing suicide.23 The results of this analysis suggest a similar effect of availability of treatment. If the means by which mental health treatment are easily accessible or close at hand, then individuals may be more likely to avail themselves of treatment.
Higher concentrations of mental health providers not only improve the chances of an individual seeking treatment, but they also can lead to better treatment. Denser areas of mental health providers area associated with higher levels of follow-up care and lower rates of prescription only treatment.21 Consistent with the results of this study, timely and recurring visits with mental health providers can improve care coordination with other providers24 and is associated with other positive behavioral health outcomes.25, 26 However, it should be noted that insurance coverage, out-of-pocket costs, and limited mental health service provider participation in insurance plans can be important barriers to accessing mental health treatment,27 and thus, an increase in provider concentration might not necessarily translate into more utilization of treatment.
Policies designed to expand availability of and access to mental health treatment could be considered as part of the response to reduce suicides. Improving reimbursement rates to mental health providers to match traditional health providers may serve to increase their supply, particularly in low density areas, and encourage them to participate in more insurance networks.28,29,30 Better consumer education efforts could also improve access, as most individuals lack basic information on mental health treatment or how to obtain it, posing a significant barrier to adequate treatment.31
While broader availability of mental health treatment options does reduce suicide risk, it is still evident from the literature that access alone is not sufficient in and of itself. More work is needed, particularly among primary care providers, to whom a majority of individuals first turn for mental health treatment.31 If these providers have only limited experience with behavioral health issues, they may be unable to treat or refer their patients to specialists for appropriate care. Steps could be taken to develop improved screening procedures to identify suicide risk and improve the awareness of primary care providers of mental health issues.
References
Heron M. Deaths: Leading Causes for 2015. National Vital Statistics Reports. 2017;66(5):2-76.
Case A, Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences. 2015;112(49):15078-15083.
Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999-2014. NCHS Data Brief 241. Published April 2016.
Shepard DS, Gurewich D, Lwin AK, et al. Suicide and Suicidal Attempts in the United States: Costs and Policy Implications. Suicide and Life-Threatening Behavior. 2016;46(3):352-362.
Substance Abuse and Mental Health Services Administration. Leading Change 2.0: Advancing the Behavioral Health of the Nation 2015-2018. HHS Publication No. (PEP) 14-LEADCHANGE2. Published 2014.
Lonnqvist JK, Henriksson MM, Sisometsa ET, et al. Mental disorders and suicide prevention. Psychiatry and Clinical Neurosciences. 1995;49:S111-S116.
Gibbons RD, Hur K, Bhaumik DK, et al. The relationship between antidepressant medication use and rate of suicide. Archives of General Psychiatry. 2005;62(2):165-172.
Olfson M, Shaffer D, Marcus SC, et al. Relationship between antidepressant medication treatment and suicide in adolescents. Archives of General Psychiatry. 2003;60(10):978-982.
Brown GK, Have TT, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. Journal of the American Medical Association. 2005;294(5):563-570.
Guthrie E, Patton GC, Kapur N, et al. Randomised controlled trial of brief psychological intervention after deliberate self poisoning - Commentary: Another kind of talk that works? British Medical Journal. 2001;323(7305):135.
Hawton K, Townsend E, Arensman E, et al. Psychosocial versus pharmacological treatments for deliberate self harm. The Cochrane Database of Systematic Reviews. 2000;2.
Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. American Journal of Psychiatry. 2002;159(6):909-916.
Mutter R, Lynch S, Ali MMA, et al. Suicide Prevention: Access To Behavioral Health Services Lacking. https://www.healthaffairs.org/do/10.1377/hblog20160810.056111/full/. Accessed August 10, 2016
Hom MA, Stanley IH, Joiner Jr TE. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: A review of the literature. Clinical Psychology Review. 2015;40:28-39.
Katz IR, Kemp JE, Blow FC, et al. Changes in Suicide Rates and in Mental Health Staffing in the Veterans Health Administration, 2005–2009. Psychiatric Services. 2013;64(7):620-625.
Fischer EP, McSweeney JC, Wright P, et al. Overcoming Barriers to Sustained Engagement in Mental Health Care: Perspectives of Rural Veterans and Providers. The Journal of Rural Health. 2016;32(4):429-438.
Ira R. Katz, Janet E. Kemp, Frederic C. Blow, et al. Changes in Suicide Rates and in Mental Health Staffing in the Veterans Health Administration, 2005–2009. Psychiatric Services. 2013;64(7):620-625.
Sher L. Does the physician density affect suicide rates among adolescents and young adults? International Journal of Adolescent Medicine and Health. 2013;25(3):315.
Hedegaard H, Curtin SC, Warner M. Suicide mortality in the United States, 1999–2017. NCHS Data Brief 330. Published November, 2018.
Han B, McKeon R, Gfroerer J. Suicidal ideation among community-dwelling adults in the United States. American Journal of Public Health. 2014;104(3):488-497.
Jones JM, Ali MM, Mutter R, et al. Factors that Affect Choice of Mental Health Provider and Receipt of Outpatient Mental Health Treatment. The Journal of Behavioral Health Services & Research. 2018;45(4):614-626.
Wooldridge JM. Econometric analysis of cross section and panel data. MIT press; 2010.
Sarchiapone M, Mandelli L, Iosue M, et al. Controlling access to suicide means. International Journal of Environmental Research and Public Health. 2011;8(12):4550-4562.
Ellen M. Comprehensive case management in the private sector for patients with severe mental illness. Psychiatric Services. 1997;48(7):911.
Marshall M, Lewis S, Lockwood A, et al. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Archives of General Psychiatry. 2005;62(9):975-983.
Mclaughlin CG. Delays in treatment for mental disorders and health insurance coverage. Health Services Research. 2004;39(2):221-224.
McKenna RM, Pintor JK, Ali MM. Insurance-Based Disparities In Access, Utilization, And Financial Strain For Adults With Psychological Distress. Health Affairs. 2019;38(5):826-834.
Mark TL, Olesiuk WJ, Ali MM, et al. Differential Reimbursement of Psychiatric Services by Psychiatrists and Other Medical Providers. Psychiatric Services. 2018;69(3):281-285.
Bishop TF, Press MJ, Keyhani S, et al. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181.
Mark TL, Olesiuk WJ, Sherman LJ, et al. Effects of the 2013 Psychiatric Current Procedural Terminology Codes Revision on Psychotherapy in Psychiatric Billing. Psychiatric Services. 2017;68(68):1197-1200.
Mickus M, Colenda CC, Hogan AJ. Knowledge of mental health benefits and preferences for type of mental health providers among the general public. Psychiatric Services. 2000;51(2):199-202.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The results in this paper are based on restricted access data from the National Survey on Drug Use and Health and the Mortality Data File. Interested readers can contact the authors for information on how to obtain access. No official endorsement by the Agency for Healthcare Research and Quality or the US Department of Health and Human Services is intended or should be inferred. This paper has not been subject to the Congressional Budget Office’s regular review and editing process. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Congressional Budget Office. No author reports any conflict of interest or financial support.
Rights and permissions
About this article
Cite this article
McClellan, C., Ali, M.M. & Mutter, R. Impact of Mental Health Treatment on Suicide Attempts. J Behav Health Serv Res 48, 4–14 (2021). https://doi.org/10.1007/s11414-020-09714-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-020-09714-4