Abstract
The objective of this study was to examine the effectiveness of a weight loss program for individuals with schizophrenia in usual care. The study included 146 adults with schizophrenia from two mental health clinics of the Department of Veterans Affairs. The 109 individuals who were overweight or obese were offered a 16-week, psychosocial, weight management program. Weight and Body Mass Index (BMI) were assessed at baseline, 1 year later, and at each treatment session. Only 51% of those who were overweight or obese chose to enroll in the weight management program. Participants attended an average of 6.7 treatment sessions, lost an average of 2.4 pounds, and had an average BMI decrease of 0.3. There was no significant change in weight or BMI compared to the control group. Intervention strategies that both improve utilization and yield greater weight loss need to be developed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
While significant advances have been made in the pharmacological management of psychosis, gains are being offset by the increased liability of weight gain associated with newer second generation antipsychotic medications. At present, the vast majority of antipsychotic medication prescriptions are for the second generation medications. As a result, the most common, serious side effect that is seen in schizophrenia is weight gain and related diabetes, hyperlipidemia, and hypertension. Weight gain, obesity, and resultant medical problems are increasingly recognized as critical side effects and pervasive problems in schizophrenia. Although efficacy studies have shown support for weight loss programs in schizophrenia, studies examining the effectiveness of these interventions into routine care are lacking. This paper describes the effectiveness of an in-person, psychosocial, weight management intervention for individuals with schizophrenia.
Compared to the general population, individuals with schizophrenia are more likely to be overweight or obese. Between 40% and 60% of people with schizophrenia are obese compared to about 30% of the general population.1,2 Obesity increases the risk for cardiovascular morbidity, impaired quality of life, and death.3 It is also a risk factor for diabetes.4 The prevalence of diabetes is particularly high in schizophrenia (16–25%) compared to the general population (4%),5 and there is evidence that this prevalence has increased since the introduction of second generation antipsychotic medications.6 Ninety percent of diabetes cases are type II diabetes3, and obesity is a particularly important risk factor as 90% of individuals with type II diabetes are obese.7 Other medical consequences associated with weight gain are hyperlipidemia, hypertension, cardiovascular disease, gallstones, osteoarthritis, sleep apnea, and colon, breast, and endometrial cancer.8–12
Weight gain has been associated with the use of second generation antipsychotic medications, which differ in their weight gain liability.13 Second generation antipsychotic medications have almost entirely displaced older first generation medications. While these new medications offer certain advantages in terms of tolerability, this medication class has weight gain as a major side effect. Olanzapine and clozapine have, on average, the greatest risk for weight gain (an average of 10 lb during relatively brief efficacy trials).13 Risperidone and quetiapine are associated with moderate risk for weight gain, and ziprasidone and aripiprazole are associated with little or no risk.13,14
A review of empirically validated weight interventions for individuals with schizophrenia found that these programs emphasized nutrition, exercise, and behavioral change to stabilize or reduce weight.15–19 Subsequent reviews and results of meta-analyses support the efficacy of behavioral or psychoeducation-based interventions to stabilize weight and promote modest weight loss among individuals with schizophrenia.16,20–23 Components of these psychosocial interventions have included (1) psychoeducation regarding diet and exercise, (2) goal-setting, (3) self-monitoring of food and physical activity level, (4) caloric restriction, and (5) increase in physical activity. Clinical trials have found support for modest weight loss among individuals with severe mental illness who received the psychosocial intervention relative to those in the control condition.18,19,24–31 Weight loss in these studies ranged from 1 to 7 lb with a mean weight loss of 5 lb across all 10 studies. Even modest weight loss has been associated with health benefits, including improved cardiovascular health among individuals who are overweight or obese.32–37 Given the available evidence, the research team developed an implementation toolkit for a wellness program, with standardized protocols for weight management services specifically designed for clients with severe mental illness.
Study aims
Although efficacy studies have shown support for weight loss programs in schizophrenia, studies examining the effectiveness of these interventions in routine care are lacking. Efficacy studies address whether a treatment improves outcomes under controlled conditions that optimize separation of the treatment effect through design features such as randomization, control conditions, homogeneous samples, standardized treatment protocols, and blinding of participants, assessors, and clinicians. Although high in internal validity, such studies have limited external validity as they often deviate substantially from usual treatment conditions. For example, efficacy studies have enrolled highly motivated clients, provided free care, paid participating clients, used specialized clinicians, excluded clients with comorbid conditions, and used research staff to maintain compliance. In contrast, effectiveness research addresses whether these interventions work in usual care where clients may not want weight services, may be ambivalent regarding weight loss and are not compensated for participation, and where mental health clinicians may not have expertise in wellness services or believe in the efficacy of the intervention.
The present study evaluates the effectiveness of a psychosocial, weight loss program for individuals with schizophrenia in usual care. The specific aims are (1) to describe the prevalence of overweight and obese veterans, (2) to examine utilization of weight-loss services in usual care and identify predictors of utilization, and (3) to examine outcomes of the EQUIP Wellness Program compared to a control group.
Methods
Study design
“Enhancing QUality-of-care In Psychosis” (EQUIP) was a longitudinal VA project that included evaluation of a chronic care model for schizophrenia (see implementation paper for greater details regarding study design).38 Data were collected at mental health clinics within the Greater Los Angeles and Long Beach VA Healthcare Systems. Psychiatrists were randomized to the chronic care model (intervention group) or treatment as usual (control group). Veterans at these clinics were assigned to the same study arm as the psychiatrist with whom they were associated. Participants in this weight study were only those who were assigned to the intervention arm of the EQUIP study. Hence, this study is not a randomized trial.
EQUIP enrolled a random sample of adult clients who met the following criteria: (1) a diagnosis of schizophrenia or schizoaffective disorder as determined by an abbreviated version of the Structured Clinical Interview for the DSM-IV,39 and (2) at least one mental health clinic visit during a 4-month period. Real-time, visit-based sampling was used over a 5-month enrollment period to identify a random sample of clients that met criteria. To ensure that visit frequency did not affect the probability of being selected, clients were eligible only at their first visit during the enrollment period. Fifty-one percent of eligible clients consented to participate (N = 398). Written informed consent from clinicians and clients was obtained after the study had been fully explained.
The EQUIP Wellness Program was offered only to those individuals who were in the EQUIP intervention arm of the study. Therefore, this study includes only those who were randomized to the chronic care model (N = 146). Clients were interviewed in person upon enrollment in the EQUIP study and approximately one year later. They were offered the weight management intervention during this time if they were overweight. For the purpose of this study, those who were overweight/obese and chose to utilize the weight loss program are considered the intervention group, and those who were overweight/obese and did not enroll in the weight loss program are considered the control group. Veterans who did not enroll in this weight loss program did not have access to any other weight loss program. Those who attended the weight loss program were also weighed at each session. In addition, the research team facilitated monthly calls with each site’s opinion leader and nurse care coordinator in order to address barriers to implementation of the program.
Participants
Study participants (N = 146) were primarily male (93%) and averaged 50.8 ± 9.1 years old. Sixty-nine percent of participants were White, 18% were African-American, 8% were Hispanic, and 5% were from other ethnic groups. Most (89%) were unemployed, and approximately half of the sample had never married (49%).
Measures
The height and weight of all study participants were measured at baseline. Weight was measured again at the 12-month follow-up. Body mass index (BMI) was calculated at each assessment based on weight and height. Individuals who participated in the Wellness Program were also weighed weekly, and their BMI was calculated for their first and last weight sessions. Data on antipsychotic medication was also collected. Clozapine and olanzapine were classified as high weight liability medications. Risperidone, quetiapine, thioridizine, and thorazine were classified as moderate weight liability medications, and all other first generation antipsychotic medications were classified as none/low weight liability medications. If a participant was taking more than one antipsychotic medication, the medication with the highest weight gain liability was considered primary. Data regarding utilization of individual and group sessions were also collected.
Intervention
The EQUIP team developed an implementation toolkit for the Wellness Program which included standardized protocols for weight management services specifically designed for clients with severe mental illness. The Wellness Implementation Toolkit was based on the Solutions for Wellness program,40 a psychoeducational program of weight management topics designed for individuals with cognitive difficulties which included written handouts at a fifth grade reading level. The research team manualized Solutions for Wellness by slightly modifying two sections of its program (the Fitness and Exercise section and the Nutrition, Wellness, and Living a Healthy Lifestyle section) and assembling these topics into a 16-session, weekly, group program. Wellness sessions were led by the nurse care coordinator at each site, who had attended a 3-day training in Solutions for Wellness delivered by Partners for Excellence in Psychiatry at the University of Medicine and Dentistry of New Jersey–University Behavioral HealthCare.
The EQUIP Wellness Program sessions focused on healthful weight management techniques and light physical exercise. Sessions included education about fiber, water, fat, cholesterol, and sugar; education about portion sizes, the food pyramid, and alcohol; and behavioral techniques to adjust unhealthy eating and begin regular light exercise. Group sessions utilized handouts, knowledge quizzes, and learning principals that work in schizophrenia (i.e., repetition, writing out main points, reading aloud, concrete examples and frequent summaries and evaluation of learning status).41 Other adaptations for this population included increased structure and intensity of contacts, simple language, and smaller chunks of information delivered at any given time. In addition to weekly group sessions, nurse care coordinators were available to meet with clients individually to discuss weight matters as needed. Attendance and weight were taken at each group session.
Data analysis approach
Group differences in pretreatment characteristics were examined using chi-square tests for categorical variables and t tests for continuous variables. Logistic regression was used to further examine treatment enrollment, and linear regression was utilized to examine predictors of total sessions attended. In regard to outcome data, paired t tests were first used to assess whether changes in weight and BMI from the first to the last session were significantly different from zero. Because weekly weights were not available for those who did not participate in the wellness program, comparisons with the control group were based on data from the baseline and follow-up interviews. Paired t tests were used to assess changes in weight from baseline to follow-up among those who enrolled in the wellness program and among those in the control group. Lastly, repeated measures analysis controlling for site and medication weight gain liability were conducted to examine group difference (wellness program versus control) in treatment outcomes of weight and BMI.
Results
Prevalence of overweight/obese veterans and treatment utilization
Seventy-five percent of clients at these clinics (n = 109) were overweight or obese. Specifically, 36% (n = 52) were overweight with a BMI of 25–29.9 and 39% (n = 57) were obese with a BMI of 30 or greater. Only half of individuals who were overweight or obese chose to enter the wellness program, despite their clinician’s referral. Of the109 individuals who were overweight or obese, 51% (n = 55) of study participants enrolled in the EQUIP Wellness Program. Those who enrolled in the program were more likely to be obese according to BMI categories whereas those who did not enroll were more likely to be overweight (χ 2 = 4.0, p < 0.05) (see Table 1). Those who entered the program were also more likely to be receiving treatment at clinic A as compared to clinic B (χ 2 = 20.3, p < 0.001). Those who enrolled in the program did not differ from those who did not in regard to demographic variables, BMI (continuous), weight, or weight gain liability of their antipsychotic medication. A logistic regression predicting enrollment in the weight loss program was conducted with BMI category and clinic as predictors. Overweight individuals were significantly less likely than obese individuals to enroll in the weight loss program (odds ratio = 0.4; 95% CI 0.2–0.9; p < 0.05), and clients at clinic A were significantly more likely than clients at clinic B to enroll in the program (odds ratio = 7.2; 95% CI 3.0–17.4; p < 0.001).
Study participants were offered 16 group wellness sessions and as many individual sessions as needed. Among the 55 individuals who enrolled in the program, everyone attended at least one group session for an average of 3.8 (SD = 4.6) sessions. In addition, 75% (n = 41) attended at least one individual session for an average of 3.9 (SD = 3.0) sessions. In total, study participants received an average of 6.7 (SD = 5.2) in-person sessions (range 1–23). Linear regression was utilized to examine predictors of total sessions attended. Independent variables in the model were gender, age, ethnicity, years of education, marital and work status, BMI, weight, weight gain liability of antipsychotic medication, and treatment site. The overall model was not significant (F = 1.3, p = 0.3), and none of the independent variables were significant.
Change in weight and BMI from first to last weight session
Study participants were weighed at each group wellness session. Of the 55 people who received services, five attended only one session and were, therefore, dropped from these analyses. Participation in the wellness program resulted in an average weight loss of 2.4 lb (SD = 10.6) and an average BMI decrease of 0.3 (SD = 1.5). Paired t tests indicated that neither of these changes were significant (t = 1.6, p = 0.12 and t = 1.5, p = 0.13, respectively).
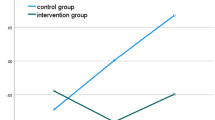
Weight outcomes compared to the control group
Because weekly weights were not available for those who did not participate in the wellness program, comparisons with the control group were based on data from the baseline and follow-up interviews (see Table 2). The wellness group lost an average of 2.3 lb (SD = 18.0), and the control group lost an average of 2.2 lb (SD = 11.9). When examining only those individuals who were categorized as obese at baseline (excluding those who were overweight), individuals in the wellness group lost an average of 4.8 lb (SD = 19.7), and the control group lost an average of 0.7 lb (SD = 9.8). A different pattern emerged when examining only those individuals who were categorized as overweight at baseline (excluding those who were obese). Those in the wellness group gained an average of 1.6 lb (SD = 14.6), and those in the control group lost an average of 3.2 lb (SD = 13.2).
The results were similar in regard to BMI. BMI in the wellness group decreased an average of 0.3 (SD = 2.6), and BMI in the control group decreased an average of 0.3 (SD = 1.7). When examining only those individuals who were categorized as obese at baseline (excluding those who were overweight), BMI in the wellness group decreased an average of 0.7 (SD = 2.9), and BMI in the control group decreased an average of 0.1 (SD = 1.4). Again, a different pattern emerged when examining only those individuals who were categorized as overweight at baseline (excluding those who were obese). BMI in the wellness group increased an average of 0.2 (SD = 2.0), and BMI in the control group decreased an average of 0.4 (SD = 1.9).
Mixed model, repeated measures analysis controlling for site and medication weight gain liability were conducted to examine group difference (wellness program versus control) in treatment outcomes of weight and BMI. Fixed effects of treatment, site, and medication were entered into the model as well as the random effects of subjects. Although there was a significant decrease in weight in both groups over time [F (1, 94) = 5.2, p < 0.05], the interaction between time and treatment group was insignificant [F (1, 94) = 1.2, p > 0.05], indicating the groups did not differ in their weight loss over time. There was, however, a significant interaction between time and site such that participants at clinic A lost weight over time while clients at clinic B gained weight over time [F (1, 94) = 6.3, p < 0.05]. The results were similar in regard to BMI. Although there was a significant decrease in BMI in both groups over time [F (1, 94) = 5.7, p < 0.05], the interaction between time and treatment group was insignificant [F (1, 94) = 1.3, p > 0.05], indicating the groups did not differ in BMI reduction over time. There was also a significant interaction between time and site such that participants at clinic A had a decrease in BMI over time while clients at clinic B had an increase in BMI over time [F (1, 94) = 7.1, p < 0.01].
Conclusions
The Schizophrenia PORT 42 is a national set of psychosocial treatment recommendations for schizophrenia which has undergone revision incorporating recent advances in knowledge. This update of treatment guidelines now includes psychosocial interventions for weight as an evidence-based practice. Hence, it is becoming increasingly important to develop and implement effective weight management programs for this population. This report examines the effectiveness of a psychosocial weight loss program for individuals with schizophrenia in routine care.
Study results indicate a great need for weight loss programs given the high prevalence of overweight and obese clients at these clinics (75%). Only half of individuals who were overweight or obese chose to enter the program, and those who did enroll attended sporadically, utilizing approximately 25% of the program. They attended an average of four of the 16 group sessions available to them and had an average of four individual sessions with the nurse care coordinator. Treatment utilization was lower than seen in most efficacy studies of psychosocial weight interventions. However, the vast majority of published studies in this area do not report utilization or drop out rates, and those that do report drop out rates show great variation (10–90%).23
Further, the utilization rates seen in efficacy studies are probably not generalizable to usual care. Although treatment dropout is substantial in efficacy studies as well, participants enroll and make an initial commitment to a certain number of sessions presumably because they are motivated to lose weight. In contrast, the present effectiveness study examined clients in usual care who did not make any commitment to participate in a weight loss program beyond attending one time. They could attend the weight loss program even if they were ambivalent about their weight, and hence, were more likely to drop out of treatment or attend sporadically.
The intervention had only a small effect on weight in usual care. Participation in the program resulted in an average weight loss of 2.4 lb and a BMI decrease of 0.3. These changes were not significant and did not differ from the control group. The effect of the intervention was not of the magnitude previously seen in efficacy studies. One potential reason for this may be differences in exclusion criteria between this study and prior efficacy studies. Prior studies excluded participants who had physical conditions that may complicate weight loss (e.g., a thyroid condition). Those with physical conditions were not screened out in this study as they would be in a rigorous efficacy study. A study limitation in regard to outcomes is the lack of outcome data prior to the 1-year follow-up. The EQUIP Wellness Program began approximately halfway through the larger clinical trial when it became clear that weight gain was a significant problem. The larger study from which this data are drawn was designed to collect data at baseline and one year. Hence, weight data is only available for the control group at those times.
An encouraging finding is that obese individuals who participated in the wellness program lost an average of 4.8 lb compared to the 0.7-lb reduction seen in the control group. The study lacked the sample size and the power to conduct subset analyses of only overweight individuals and only obese individuals. Although motivation to lose weight was not examined in this study, it is hypothesized that individuals who were obese rather than overweight had greater motivation to engage in the program and may have received more encouragement from their clinicians to participate. These possible distinctions in engagement between obese and overweight clients warrant further investigation in future studies.
Although implementation science was in its infancy at the time of this study, the research team utilized a number of strategies that have subsequently been found to maximize uptake and delivery of evidence-based practices.43 Examples of these strategies include engagement of mental health leadership from the very beginning of the project, monthly calls with clinicians and research staff to discuss and problem-solve barriers to implementation, and the provision of regular feedback to clinicians via patient reports that included weight outcomes. Organizational barriers addressed included a lack of staff time and expertise to provide wellness services to individuals with schizophrenia. Staff time was negotiated with leadership, resulting in a release of time for nurses to conduct the weight loss group. Lack of competency to provide wellness services was addressed with general education about weight problems in schizophrenia and training in the wellness intervention.
Compared to clinic B, clinic A was significantly more likely to enroll clients in the weight loss program and had better weight outcomes. Although clinician attitudes regarding weight loss programs were not formally assessed, it was clear from the beginning of this study that opinion leaders and clinicians at clinic A were more invested in implementing a weight loss program for schizophrenia. In fact, it was clinicians at clinic A who initially asked for weight loss services to be provided and who were interested in weight outcomes in response to the poor quality of care reports they received. Further, the opinion leader at clinic A volunteered to conduct a thorough literature review as part of the development of the EQUIP Wellness Program. In contrast, clinicians at clinic B did not express concern that their reports indicated a suboptimal quality of care nor did they express an interest in weight outcomes. It is possible that these differences in the organizational contexts where implementation took place affected treatment outcomes.
Previous research and the current study indicate the importance of getting administrative and frontline staff buy-in early and throughout the implementation process to improve implementation success.44 Further, leadership needs to be consistent in emphasizing the importance and value of implementing weight loss services so that frontline staff receive a clear message about expectations for the program. Future research should examine the impact of clinician attitudes and knowledge regarding the effectiveness of weight loss services on utilization and outcomes.
Client barriers to implementation included enrollment and inconsistent attendance. A limitation of the study is the lack of systematic assessment of client barriers, attitudes, and motivation to use weight loss services. However, the monthly meetings with research and clinical staff revealed that clients were often ambivalent regarding their need for weight loss, reluctant to participate in a group-based intervention, or had limited transportation options. These issues have been previously highlighted as barriers to utilization of weight loss services.45,46 Although the Wellness Program sessions were scheduled on days and at times when many clients had clinic visits, several clients still mentioned it was difficult for them to come to the clinic at the times that groups were held. Future research should focus on addressing barriers that may be associated with client utilization of wellness services, such as client self-efficacy, motivation, and readiness for change.
Methods to either increase the effect size of the intervention itself and/or change the implementation strategy need to be considered to improve the effectiveness of weight loss interventions in usual care. A prior study with individuals with schizophrenia reported a lack of knowledge about the health benefits of exercise among participants.47 Education regarding the benefits of diet and exercise and the addition of motivational interviewing techniques may improve motivation and increase treatment retention, and warrant further study in this population. Given the reported reluctance to use a group-based, weight loss program, the addition of individual sessions may also improve attendance.
Further modifications to the program would include content that is tailored to the individual’s living situation and ability to control his/her food intake (i.e., whether or not the majority of meals are prepared for them by a caregiver or a residential facility). Innovative approaches may also improve access. These may include providing a part of the intervention in community settings such as board and care homes or drop-in programs, adding in vivo activities such as shopping, cooking, plating, and paced eating, and making greater use of technology to augment in-person services, such as telephone, video, or computer-based learning. An assessment of patient preferences regarding the services offered and incorporation of their preferences into the intervention may also improve treatment adherence.
Another strategy that may potentially increase the effect size of the intervention is to improve implementation. Given the significant outcome differences and clinician attitudes between the sites, there is reason to believe that improvements in implementation at the provider level may impact patient outcomes. A better understanding of clinician attitudes and knowledge and better marketing of the intervention to staff may improve effectiveness.
Implications for Behavioral Health
The high prevalence of overweight and obese individuals at these clinics highlights the importance of weight monitoring and management in this population. Improved awareness of the efficacy of psychosocial weight loss programs and training in administering these interventions is needed among mental health clinicians. Given the challenges in implementation of such programs in routine care, weight loss is likely to be modest with existing interventions. Hence, strategies that improve implementation and increase treatment utilization and the effect size of weight loss services in usual care are needed.
References
Homel, P., Casey, D., & Allison, D. B. (2002). Changes in body mass index for individuals with and without schizophrenia. Schizophrenia Research, 55, 277-84.
Dickerson, F. B., Brown, C. H., Kreyenbuhl, J. A., et al. (2006). Obesity among individuals with serious mental illness. Acta Psychiatrica Scandinavica, 113, 306-313.
Marder, S. R., Essock, S. M., Miller, A. L., et al. (2004). Physical health monitoring of patients with schizophrenia. American Journal of Psychiatry, 161(8), 1334-1349.
Sokal, J., Messias, E., Dickerson, F. B., et al. (2004). Comorbidity of medical illnesses among adults with serious mental illness who are receiving community psychiatric services. Journal of Nervous and Mental Disease, 192, 421–427.
Mukherjee, S., Decina, P., Bocola, V., et al. (1996). Diabetes mellitus in schizophrenic patients. Comprehensive Psychiatry, 37, 68–73.
Reist, C., Mintz, J., Albers, L.J., et al. (2007). Second-generation antipsychotic exposure and metabolic-related disorders in patients with schizophrenia: an observational pharmacoepidemiology study from 1988 to 2002. Journal of Clinical Psychopharmacology, 27, 46–51.
McIntyre, R. S., McCann, S. M., & Kennedy, S. H. (2001). Antipsychotic metabolic effects: weight gain, diabetes mellitus and lipid abnormalities. Canadian Journal of Psychiatry, 46(3), 273-81.
Davidson, M. H., Hauptman, J., DiGirolamo, et al. (1999). Weight control and risk factor reduction in obese subjects treated for two years with orlistat: a randomized controlled trial. Journal of the American Medical Association, 281, 235-242.
Gordon, A. & Price, L. H. (1999). Mood stabilization and weight loss with topiramate. American Journal of Psychiatry, 156, 968-969.
Heck, A. M., Yanovski, J. A., & Calis, K. A. (2000). Orlistat, a new lipase inhibitor for the management of obesity. Pharmocotherapy, 20, 270-279.
McMahon, F. G., Fujioka, K., Singh, B. N., et al. (2000). Efficacy and safety of sibutramine in obese white and African American patients with hypertension: a 1-year, double-blind, placebo-controlled, multicenter trial. Archives of Internal Medicine, 160, 2185-91.
Sjostrom, L., Rissanen, A., Andersen, T., et al. (1998). Randomised placebo-controlled trial of orlistat for weight loss and prevention of weight regain in obese patients. Lancet, 352, 167-172.
Newcomer, J.W. (2007).Antipsychotic medications: metabolic and cardiovascular risk. Journal of Clinical Psychiatry, 68 Suppl 4, 8-13.
Newcomer, J.W., Campos, J.A., Marcus, R.N., et al. (2008). A multicenter, randomized, double-blind study of the effects of aripiprazole in overweight subjects with schizophrenia or schizoaffective disorder switched from olanzapine. Journal of Clinical Psychiatry, 69(7), 1046-1056.
Brown, C., Goetz, J., Van Sciver, A., et al. (2006). A psychiatric rehabilitation approach to weight loss. Psychiatric Rehabilitation Journal, 29, 267-273.
Faulkner, G., Cohn, T., & Remington, G. (2007). Interventions to reduce weight gain in schizophrenia. Schizophrenia Bulletin, 33(3), 654-656.
Littrell, K. H., Hilligoss, N. M., Kirshner, C. D., et al. (2003). The effects of an educational intervention on antipsychotic-induced weight gain. Journal of Nursing Scholarship, 35(3), 237-241.
Menza, M., Vreeland, B., Minsky, S., et al. (2004). Managing atypical antipsychotic-associated weight gain: 12-month data on a multimodal weight control program. Journal of Clinical Psychiatry, 65(4), 471-477.
Vreeland, B., Minsky, S., Menza, M., et al. (2003). A program for managing weight gain associated with atypical antipsychotics. Psychiatric Services, 54(8), 1155-1157.
Alvarez-Jimenez, M., Hetrick, S. E., Gonzalez-Blanch, C., et al. (2008). Non-pharmacological management of antipsychotic-induced weight gain: systematic review and meta-analysis of randomised controlled trials. British Journal of Psychiatry, 193(2), 101-107.
Faulkner, G., & Cohn, T. A. (2006). Pharmacologic and nonpharmacologic strategies for weight gain and metabolic disturbance in patients treated with antipsychotic medications. Canadian Journal of Psychiatry, 51(8), 502-511.
Faulkner, G., Soundy, A. A., & Lloyd, K. (2003). Schizophrenia and weight management: a systematic review of interventions to control weight. Acta Psychiatrica Scandinavica, 108(5), 324-332.
Loh, C., Meyer, J. M., & Leckband, S. G. (2006). A comprehensive review of behavioral interventions for weight management in schizophrenia. Annals of Clinical Psychiatry, 18(1), 23-31.
Brar, J. S., Ganguli, R., Pandina, G., et al. (2005). Effects of behavioral therapy on weight loss in overweight and obese patients with schizophrenia or schizoaffective disorder. Journal of Clinical Psychiatry, 66(2), 205-212.
Brown, S. & Chan, K. (2006). A randomized controlled trial of a brief health promotion intervention in a population with serious mental illness. Journal of Mental Health, 15, 543-549.
Jean-Baptiste, M., Tek, C., Liskov, E., et al. (2007). A pilot study of a weight management program with food provision in schizophrenia. Schizophrenia Research, 96(1-3), 198-205.
Kwon, J. S., Choi, J. S., Bahk, W. M., et al. (2006). Weight management program for treatment-emergent weight gain in olanzapine-treated patients with schizophrenia or schizoaffective disorder: a 12-week randomized controlled clinical trial. Journal of Clinical Psychiatry, 67(4), 547-553.
McKibbin, C. L., Patterson, T. L., Norman, G., et al. (2006) A lifestyle intervention for older schizophrenia patients with diabetes mellitus: a randomized controlled trial. Schizophrenia Research, 86(1-3), 36-44.
Melamed, Y., Stein-Reisner, O., Gelkopf, M., et al. (2008). Multi-modal weight control intervention for people with persistent mental disorders. Psychiatric Rehabilitation Journal, 31(3), 194-200.
Weber, M., & Wyne, K. (2006). A cognitive/behavioral group intervention for weight loss in patients treated with atypical antipsychotics. Schizophrenia Research, 83(1), 95-101.
Wu, M. K., Wang, C. K., Bai, Y. M., et al. (2007). Outcomes of obese, clozapine-treated inpatients with schizophrenia placed on a six-month diet and physical activity program. Psychiatric Services, 58(4), 544-550.
Cutler, J. (1997). Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure: the trials of Hypertension Prevention, Phase II. Archives of Internal Medicine, 157, 657-667.
Knowler, W. C., Barrett-Connor, E., Fowler, S. E., et al. (2002). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine, 346(6), 393-403.
Lean, M. E., Powrie, J. K., Anderson, A. S., et al. (1990). Obesity, weight loss and prognosis in type 2 diabetes. Diabetic Medicine, 7(3), 228-233.
National Institutes of Health. (1998). Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Washington: National Institutes of Health: NIH Pub #98-4083.
Sonne-Holm, S., Sorensen, T., Jensen, G., et al. (1989). Independent effects of weight change and attained body weight on prevalence of arterial hypertension in obese and non-obese men. British Medical Journal, 299, 767-770.
Tuomilehto, J., Lindstrom, J., Eriksson, J. G., et al. (2001). Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. New England Journal of Medicine, 344(18), 1343-1350.
Brown, A.H., Cohen, A. N., Chinman, M. J., et al. (2008). EQUIP: Implementing chronic care principles and applying formative evaluation methods to improve care for schizophrenia. Implementation Science, 15, 3-9.
First, M., Spitzer, R., Gibbon, M., et al. (1995). Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders (fourth ed, Patient Edition, version 2.0 ed.). New York, NY: New York State Psychiatric Institute.
Ryan, S., Littrell, K., Sowers, C., et al. (2000). Solutions for Wellness. Indianapolis, IN: Eli Lilly.
Schiefler, P. (2002). Partnership for Recovery: (Available from Center for Excellence in Psychiatry, University Behavioral Healthcare, 151 Centennial Avenue, Suite 1500, Piscataway, NJ, 08854).
Dixon, L. B., Dickerson, F., Bellack, A. S., et al. (2010). The 2009 Schizophrenia PORT Psychosocial Treatment Recommendations and Summary Statements. Schizophrenia Bulletin, 36, 48-70.
Damschroder, L. J., Aron, D. C., Keith, R. E., et al. (2009). Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science 4, 50.
Backer, T. E., Liberman, R. P., & Kuehnel, T. G. (1986). Dissemination and adoption of innovative psychosocial interventions. Journal of Consulting and Clinical Psychology, 54, 111–118.
Archie, S., Wilson, J. H., Osborne, S., et al. (2003). Pilot study: access to fitness facility and exercise levels in olanzapine-treated patients. Canadian Journal of Psychiatry, 48, 628-632.
Beebe, L. H. & Smith, K. (2010). Feasibility of the Walk, Address, Learn and Cue (WALC) intervention for schizophrenia spectrum disorders. Archives of Psychiatric Nursing, 24, 54-62.
Beebe, L. H., Tian, L., Morris, N., et al. (2005). Effects of exercise on mental and physical health parameters of persons with schizophrenia. Issues in Mental Health Nursing, 26, 661-676.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the Department of Veterans Affairs through the Health Services Research & Development Service (RCD 00-033, CPI 99-383, and MNT 03-213) and the VA Desert Pacific Mental Illness Research, Education and Clinical Center (MIRECC); and by the UCLA-RAND NIMH Partnered Research Center for Quality Care (P30MH082760). Any opinions expressed are only those of the authors and do not necessarily represent the views of any affiliated institutions.
Rights and permissions
About this article
Cite this article
Niv, N., Cohen, A.N., Hamilton, A. et al. Effectiveness of a Psychosocial Weight Management Program for Individuals with Schizophrenia. J Behav Health Serv Res 41, 370–380 (2014). https://doi.org/10.1007/s11414-012-9273-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-012-9273-3