Abstract
The relationship between depression and development of chronic illness among older adults is not well understood. This study uses data from the Health and Retirement Study to evaluate the relationship between depression at baseline and new onset of chronic illnesses including cancer, heart problems, arthritis, and diabetes. Analysis controlling for demographics (age, gender, race, education), health risk indicators (BMI and smoking), functional limitations (gross motor index, health limitations for work), and income show that working-age older people (ages 50–62) with depression at baseline are at significantly higher risk to develop diabetes, heart problems, and arthritis during the 12-year follow-up. No significant association was found between depression and cancer. Prevention efforts aimed at chronic illnesses among the elderly should recognize the mind–body interaction and focus on preventing or alleviating depression.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Depression is not a normal part of aging but it is the most prevalent yet least recognized and most untreated psychiatric disorder among older adults. The community sample estimates indicate a higher frequency of depression among older adults. While the prevalence of depression among people between 18 and 39 years old is 4.7%, the prevalence is 7.3% among people between 40 and 59 years old, with a peak in subjects in their 50s.1 The Surgeon General’s Mental Health Report points out that depression in older adults require particular attention because it is more likely to increase mortality from either suicide or somatic illnesses. How depression exerts these effects is not yet understood. Thus, the Surgeon General’s report concludes that an “increased understanding of depression in older people may be, literally, a matter of life and death.”1
In examining the reasons for changes in the rate of depression by age, researchers find significant associations between depression and biological (e.g., cardiovascular disease, diastolic hypertension, serotonin depletion, endocrine changes), psychological (e.g., behavioral, psychodynamic, and cognitive aberrations), social (e.g., impaired social support, loneliness, social disengagement), and spiritual (e.g., religious coping) factors.2 Although there are effective treatment options, researchers agree that mood disorders in older adults remain a notable public health issue.3 Symptoms of depression increase the risk of a decline in self-rated health while decreasing the likelihood of subsequent improvement in self-rated health.4 For example, a study among women over 50 years old found that women with persistent or new depression, relative to women with no depression, are more likely to report fair or poor self-rated physical health. In fact, the magnitude of the impact of depression on self-rated health is comparable to experiencing a major cardiac event.5 Similarly, among middle-aged men with low-health risk behaviors, those with depression are six times more likely to report average or poor health than those who were not depressed.6
There have been several studies relating depression to chronic illness among the elderly since the Surgeon General’s Mental Health Report, but relatively few start with a cohort of healthy older people to consider whether depression at baseline is associated with the development of one or more chronic illnesses.7 In the current study, a large, population-based 12-year follow-up dataset was utilized to evaluate whether there is an association between depression assessed prospectively among older persons without a history of four chronic conditions—arthritis, heart problems/stroke, diabetes, and cancer—and the subsequent development of one of these chronic illnesses as determined by self-report. This is the first study to examine the risk of developing one of the four chronic conditions by assessing clinical depression according to standardized diagnostic criteria applied to a community sample of older adults while controlling for confounding measures that allow us to adjust the risk estimates. Data in this study are enhanced by a follow-up period (12 years postbaseline) adequate to allow for an appropriate incubation period for most chronic conditions. Analyses were extended to examine whether baseline depression was associated with the number of chronic illnesses reported among older adults over the same follow-up period.
Data and Methods
Database
Data for this study are from the US Health and Retirement Survey (HRS). This survey includes a representative sample of non-institutionalized men and women born between 1931 and 1941 inclusive, and their spouses or partners. The first wave was conducted in 1992 on approximately 7,600 (12,652 individuals) households. The survey includes questions on health, functional ability, cognition, family structure, and intergenerational support within families, housing, employment, expectations, income and assets, marital history, health care utilization, major life events, insurance, and many other aspects of health and economic circumstances. This study uses RAND HRS version of the dataset since this version contains cleaned and processed variables with consistent and intuitive naming conventions, model-based imputations and imputation flags, and spousal counterparts of most individual-level variables.8
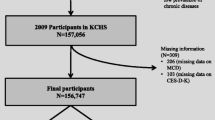
The HRS includes 12,652 subjects at the first wave (1992). The target population for wave 1 of the HRS includes all adults in the contiguous USA, aged 51–61, who reside in households. Through its unique and in-depth interviews with a nationally representative sample of adults over the age of 50, the HRS provides an invaluable, growing body of multidisciplinary data to help researchers address the challenges and opportunities of aging. The present study follows a sample of these older working age adults who are at risk for any of the four chronic conditions. Thus, the study sample is restricted to include only individuals who did not report any of the four chronic conditions at baseline (wave 1). This “no chronic illness” restriction reduces the sample size by 5,922 to a starting sample of 6,730 subjects. Then, subjects who did not participate in all six waves (12 years follow-up period) following the baseline were also excluded. This reduced the sample size by 2,427 individuals who dropped out during one of the subsequent waves. In addition, discarded sample includes 658 subjects who were less than 50 years old at baseline (n = 623) or who had missing observations (n = 35). The reason for such exclusions is to create a study population consisting of healthy individuals (absent of four chronic conditions) who are at risk for a chronic illness with complete information during the follow-up period. The final data set consists of 3,645 subjects who were between the ages of 50 and 62 at baseline and ages 62–74 at study conclusion. In terms of demographic, health, and other factors, subjects who had to be excluded due to missing data (n = 35) were very similar to the study sample (n = 3,645). The only statistically significant difference was a higher rate of heart problems reported during the follow-up period among the excluded subjects (35.4% vs. 19.0%). A cohort of 7,674 subjects who were not included in the analyses are more likely to have a chronic illness at baseline (7.3% with cancer, 52.0% with arthritis, 14.8% with diabetes, and 20.0% with heart problems), have a higher average age (65.4 years old), and are more likely to report baseline depression (12.7%). Thus, readers should be mindful throughout the study that the results, as intended, pertain to analyses of a relatively healthier population at baseline.
Variables
The HRS contains an extensive range of health measures, including self-report of chronic illnesses such as arthritis, heart problems, diabetes, cancer, and a depression index based on the Center for Epidemiologic Studies Depression Scale (CES-D). To study the onset of chronic illnesses, four dependent variables that are 0–1 indicators of whether a participant reports to have arthritis, heart problems, diabetes, or cancer are constructed. Self-reports are determined to be a valid and cost-efficient method to identify chronic illnesses.9,10 An additional dependent variable was created by summing the number of chronic illnesses reported for each individual. This dependent variable takes a value between 0 and 4 depending on the number of chronic illnesses individuals report.
The main independent variable of interest is depression status at baseline. The eight-item version of the CES-D was used to generate a 0–1 indicator of participant’s baseline depression.11 In this version of the CES-D, the depression score is the sum of six “negative” indicators minus two “positive” indicators. The negative indicators measure whether the respondent experienced the following symptoms all or most of the time (depression, everything is an effort, sleep is restless, felt alone, felt sad, and could not get going). The positive indicators measure whether the respondent felt happy and enjoyed life, all or most of the time.12 The eight-item version has been found to have good psychometric properties. Coefficient alpha for the eight-item scale was found to be 0.86 in the derivation sample, whereas the same sample’s alpha reliability coefficient for the full CES-D was 0.87. The correlation of the eight-item version with the 20-item scale was found to be 0.93 by its developers, and it distinguished well between depressed and nondepressed samples as defined by the 20-item version.13 A cut-off of three or more on the eight-item CES-D was used to generate a 0–1 indicator for subjects with depression at baseline. This cutoff point has been shown to have 72% sensitivity and 79% specificity when compared with a diagnosis by a clinician.14 In other words, 79% of individuals identified as depressed by this cut-off point would also be diagnosed as depressed by a clinician.
In multivariable analysis, other covariates that are expected to influence the onset of a chronic illness were included. Demographic characteristics include age at baseline, gender, race (Black, Hispanic), marital status, and education level (less than high school and high school graduate). Also, in all models a 0–1 indicator for body mass index greater than 29 is used to control for weight problems. A body mass index (BMI) of 30 is generally considered as the cut-off point to define obesity.15 A 0–1 indicator was defined to indicate self-report of any cigarette smoking at baseline. Other covariates to indicate health status are a functional limitations index and self-report of whether health factors limited the participant’s ability to work. Functional limitation was measured by a gross motor index with a value between 0 and 5 depending on the sum of the following difficulties: (1) difficulty walking one block, (2) walking across a room, (3) climbing one flight of stairs, (4) getting in or out of bed, (5) and bathing activities. Earlier studies show that lower household income is significantly associated with poor health outcomes.16 Therefore, a 0–1 dummy variable is used to indicate participant with an annual income of less than $20,000.
All estimated regression models allowed for separate regression intercepts for each of the four census regions, Northeast, Midwest, South, and West. These regional fixed effects control for unobserved or omitted factors (heterogeneities) specific to a location (e.g., dietary differences). A reference individual is an individual with no depression at baseline, female, non-black and non-Hispanic, single, with greater than a high school education, a body mass index of 29 or less, nonsmoker, with no health limitations for work, and resides in census region West.
Statistical Methods
In order to assess the correlation between depression and chronic illnesses a maximum-likelihood logit model was estimated for each of the four chronic illnesses and report the odds ratio as well as the marginal effects calculated at the mean of the independent variables. The odds ratio is the ratio of the odds (has a chronic condition/does not have a chronic condition) of an event occurring in the group of people with depression to the odds of it occurring in the group of people without depression. Marginal effects measure the instantaneous rate of change when all other variables are held constant at their mean value. It indicates a change in the probability of having one of the chronic illnesses when the independent variable increases by one unit. An ordinal logistic regression is estimated for the second outcome measure to investigate whether depression at baseline is associated with reporting higher number of chronic conditions during follow-up. A categorical variable is considered ordinal if there is a natural ordering of the possible values. Ordinal logistic regression is most often applied when the dependent variable includes ordinal categorical responses with more than two possible values.
Results
Table 1 presents the definitions of variables and descriptive statistics for the study sample. At baseline, 5.2% of the sample was depressed based on their scores on the eight-item CES-D instrument. Over the length of the 12-year follow-up, 45.4% developed arthritis, 19.0% developed heart problems, 13.9% reported diabetes, and 10.6% reported cancer. The average age at baseline (in 1992) was 55.8 years. The study sample included 51% males; 12.9% Black, and 1.3% Hispanic. While 79.6% were married, 20.6% have less education than a high school diploma, and 53.8% are high school graduates. Of the sample, 19.1% had a BMI over 29 and 23.5% were reported to be smokers at baseline interview. Eight point three percent reported that health limits their work and more than half (54%) of the sample (including those reporting no annual income, e.g., housewives, unemployed) had an annual income less than $20,000.
Table 2 presents marginal effects, odds ratios, and associated probabilities. Regression results indicate that individuals with depression are 1.50 times more likely to report arthritis, 1.69 times more likely to report heart problems, and 1.50 times more likely to report diabetes during the 12-year follow-up. Having depression increases the probability of reporting arthritis by 10.0%, the probability of reporting heart problems by 8.8%, and the probability of reporting diabetes by 5.0% (assuming all other covariates are held constant at the mean).
Males are significantly more likely to report any of the four chronic illnesses. As expected, age has a significant and positive association with heart problems and cancer. There are some striking findings regarding racial and ethnic background indicators. For example, Blacks are less likely to report cancer and Hispanics are more likely to report diabetes. In addition, older adults with less than a high school degree are more likely to report diabetes. Having a BMI greater than 29 increases the risk of having diabetes and arthritis. Smokers and those who report higher functional limitations at baseline are more likely to report heart problems. Participants who report that health limits their work at baseline are more likely to report arthritis during the 12-year follow-up. Depression is the most common baseline predictor of the chronic illnesses but age, gender variable (males), and obesity indicator (BMI > 29) are also appearing as combination of baseline characteristics that seem to be related to developing the chronic conditions when depression is present.
In terms of number of chronic conditions, older adults with depression (but without any of the four chronic illnesses) at baseline are 1.77 times more likely to have an additional chronic illness. In Table 3, age, male gender, less than high school or high school equivalent education, body mass index greater than 29, being a smoker, and reporting health limitations on work are all significant and increasing risk factors for reporting an additional chronic illness. Having an annual income less than $20,000 does not seem to be associated with any of the four chronic conditions and having less than high school education is associated with only developing diabetes. In part, these results may be related to the fact that study sample includes subjects who are over the age of 50 and who are relatively healthier. Low income and less education would have a reverse association with a lifelong accumulation of healthy knowledge and behaviors. People who have been in the low-income and less-educated group may have developed a chronic condition before age 50 and/or before the study baseline and may have been excluded from the study.
A sensitivity analysis was implemented to test whether the estimation results are sensitive to using only baseline depression indicator. It is plausible to suggest that some subjects may report temporary depressive symptoms (at the time of baseline survey) which may not really have long-term effects on physical health. Thus, an alternative measure was created to define “people with depression” if the subjects report depression both at waves 1 and 2. Results suggest that, other than changes in magnitudes of some coefficients, the findings were very similar to the ones presented in this study. The dataset does not include information on drug abuse. In addition, initial analyses including “excessive alcohol use” (drinking three or more drinks per day) as a covariate did not produce a significant coefficient in any of the multivariable estimations (See Table 4 in Appendix). This may be due to the static (snapshot) measurement of the alcohol use in wave 1. In light of this cautionary note, it should be noted that prolonged utilization of substance abuse will have profound negative impacts on health status of older adults.
Discussion
This study finds that depression is significantly associated with three of the four chronic illnesses examined during the 12-year follow-up among older adults. Significant and positive associations were noted with arthritis, heart problems, and diabetes. Cancer was not found to be related to baseline depression.
As demonstrated with this study, depression among older adults is a serious risk factor for disabling chronic conditions. This also has important implications for the economic costs of treatment among the elderly. Depression combined with another chronic disease tends to be particularly costly. A recent study reports that employees with a co-morbid general medical condition (e.g., back pain, diabetes, heart disease, or hypertension) and depression cost 1.7 times more to treat than those with either condition alone.17 Intervention programs that integrate employee assistance, wellness, and disease management can be an effective way to address co-morbid chronic illnesses. With integrated programs like these, health professionals help people make healthy lifestyle modifications, treat chronic diseases through a long-term disease management approach that aims to prevent worsening of chronic medical conditions, and evaluate and treat people for psychiatric issues through comprehensive health and behavioral health programs. Workforce wellness programs can be valuable both for the employees and employers due to the real impact on job performance. Employees would feel better when they exercise regularly and eat healthy meals, and can manage their daily stress and possible symptoms of depression. Employers’ positive outlook can increase productivity and reduce overall cost of their health care.
The co-occurrence of and bidirectional association between depression and chronic physical illnesses may make it difficult to provide effective treatment. For example, many individuals with chronic medical conditions have untreated, co-morbid mental health or substance use disorders, and these may complicate recovery from physical illness in a myriad of ways. A diagnosis of type 2 diabetes nearly doubles an individual’s risk for depression; an estimated 28.5% of diabetic patients in the USA meet criteria for clinical depression. Diabetic patients with depression are less likely to adhere to special diets or to refill medications, thus worsening their medical issues through poor care management. Approximately one in six patients treated for a heart attack experiences major depression soon after their heart attack, and at least one in three heart attack survivors have significant symptoms of depression. Patients with depression who suffer a heart attack are about 3.5 times more likely to die. The findings of the current study indicate that screening and early intervention for depression would likely improve healthcare management for several major physical health issues among older adults and, thus, would enhance quality of life for those living with chronic illness.
Implications for Behavioral Health
There is a clear relationship between depression and the development of some chronic illnesses. Prevention efforts aimed at reducing the impact and incidence of chronic physical illnesses among the elderly must also recognize the mind–body interaction and focus on preventing or alleviating depression while treating the concomitant physical health issue. Depression, as evidenced by this 12-year follow-up study, significantly increases one’s chances of developing physical illnesses.
Besides pharmacological interventions, the primary prevention of depression may involve multimodal strategies to enhance self-efficacy in older adults. For example, a study among an older population found that the provision of instruction on and information about mind–body relationships, relaxation training, cognitive restructuring, problem solving, communication, and behavioral treatment for insomnia, nutrition, and exercise resulted in significant decreases in symptoms of depression among older adults.18 A recent study suggests that “depression is commonly encountered in primary care settings yet is often missed or suboptimally managed.”19 It is critical to explore opportunities for effective depression screening and interventions for the elderly in settings frequented by them, such as primary care settings and senior centers. Of course, the growing Baby Boomer demographic is expected to create a significant increase in the number of older adults with mental health and/or substance use/abuse issues as well as expand the types of settings in which older adults may be encountered. This population was not captured in the current study.
This study has several strengths. The study data pertains to a large population-based dataset that allows for a 12-year follow-up post-baseline among older adults. This is the first study examining the risk of developing one of the chronic physical health conditions during a 12-year follow-up among older adults reporting depression but absent of any of the four chronic conditions at baseline. Moreover, the HRS database provides an adequate sample size that allows for a particular focus on chronic illnesses among older people. This dataset provides a rich set of information which enables to control for other variables via multivariate analysis that may significantly affect the development of a chronic illness.
The study findings are also subject to some caveats. First, analysis includes data on the individuals who were present at all seven waves of the survey, resulting in the loss of a large number of subjects from baseline. Future studies might construct and estimate a dynamic model to test the study findings. The study subjects were selected from the individuals who reported being healthy at baseline (i.e., no report of the four chronic illnesses examined here). Selecting individuals based on this health status may result in an underestimation of the association between depression and chronic illness since there may be more individuals among the excluded sample with poor health. Despite these caveats, study goal and timeliness, design and estimation methods, and the robust findings along with important policy implications, together represent a set of novel contributions in this line of research.
References
US DHHS (Department of Health and Human Services). Mental Health: A Report of the Surgeon General—Executive Summary. US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health. Rockville, MD. 1999.
Blazer DG. Depression in late life: review and commentary. The Journal of Lifelong Learning in Psychiatry. 2009. 7(1); 118–136
Reynolds III C, Charney D. Editorial: unmet needs in the diagnosis and treatment of mood disorders in late life. Biological Psychiatry. 2002; 52: 146.
Han B. depressive symptoms and self-rated health in community-dwelling older adults: a longitudinal study. Journal of the American Geriatrics Society. 2002; 50(9):1549–1556.
Ruo B, Bertenthal D, Sen S, et al. Self-rated health among women with coronary disease: depression is as important as recent cardiovascular events. American Heart Journal. 2006; 152(5):921.e1–921.e7
ZZ Naslindh-Ylispangar, A., Sihvonen, M., Sarna, S, et al. (2008), Health status, symptoms and health counselling among middle-aged men: comparison of men at low and high risk. Scandinavian Journal of Caring Sciences, 22:529–535.
Gallo, JJ, Armenian KH, Ford DE, et al. Major depression and cancer: the 13 year follow-up of the Baltimore Epidemiologic Catchment Area sample (United States). Cancer Causes and Control. 2000; 11: 751–758
St.Clair P, Blake D, Bugliari D, et al. RAND HRS Data Documentation: Version F. Rand Center for the Study of Aging. 2006.
Martin L, Leff M, Calonge N, et al. Validation of self-reported chronic conditions and health services in a managed care population. American Journal of Preventive Medicine. 2000; 18(3): 215–218.
Skinner, KM, Donald MR, Elizabeth L, et al. concordance between respondent self-reports and medical records for chronic conditions: experience from the Veterans Health Study. Journal of Ambulatory Care Management. 2005; 28(2): 102–110.
Huba GJ, Melchior LA. The Measurement Group and HRSA/HAB’s SPNS Cooperative Agreement Steering Committee Module 26B: CES-D8 Form (Interview). 1995. Available from: www.TheMeasurementGroup.com. Culver City, California: The Measurement Group.
Conti RM, Berndt ER, Frank RG. Early retirement and DI/SSI applications: exploring the impact of depression. NBER Working Paper #12237. 2006.
Melchior LA, Huba GJ, Brown VB, et al. A short depression index for women. Educational and Psychological Measurement. 1993. 53(4): 1117–1125
Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics 1999; 11(2):139–48.
CDC. Centers for Disease Control and Prevention. 2009. Defining overweight and obesity. Accessed on July 1, 2009. Available from: http://www.cdc.gov/
Kawachi I, Kennedy BP, Glass R. (1989). Social capital and self-rated health: a contextual analysis. American Journal of Public Health. 89(8):1187–1193
Druss GB, Rosenheck RA, Sledge WH. Health and disability cost of depressive illness in a major US corporation. American Journal of Psychiatry. 2000; 157(8): 1274–78.
Rybarczyk B, De Marco G, DeLa Cruz M, et al. Comparing mind–body wellness interventions for older adults with chronic illness: classroom versus home instruction. Behavioral Medicine. 1999; 24: 181–190
Gilbody S, Whitty P,Grimshaw J, et al. educational and organizational interventions to improve the management of depression in primary care. Journal of American Medical Association. 2003; 289: 3145–3151.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Karakus, M.C., Patton, L.C. Depression and the Onset of Chronic Illness in Older Adults: A 12-Year Prospective Study. J Behav Health Serv Res 38, 373–382 (2011). https://doi.org/10.1007/s11414-011-9234-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-011-9234-2