Abstract
Most substance abuse treatment occurs in outpatient treatment centers, necessitating an understanding of what motivates organizations to adopt new treatment modalities. Tichy’s framework of organizations as being comprised of three intertwined internal systems (technical, cultural, and political) was used to explain treatment organizations’ slow adoption of buprenorphine, a new medication for opiate dependence. Primary data were collected from substance abuse treatment organizations in four of the ten metropolitan areas with the largest number of heroin users. Only about one fifth offered buprenorphine. All three internal systems were important determinants of buprenorphine adoption in our multivariate model. However, the cultural system, measured by attitude toward medications, was a necessary condition for adoption. Health policies designed to encourage adoption of evidence-based performance measures typically focus on the technical system of organizations. These findings suggest that such policies would be more effective if they incorporate an understanding of all three internal systems.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Technology, in the form of new pharmaceuticals, devices, and procedures, has accounted for roughly one half of the growth in health expenditures and for most of the difference between the higher annual growth in health care expenditure and annual overall growth in the US economy since 1960.1 While a number of studies have assessed the overuse of technologies based on clinical evidence, there are also studies that point to the underuse of medical technologies and new knowledge, both medical therapies and clinical standards.2–4
Understanding the determinants of the use or nonuse of new technologies is critical for achieving a more efficient and higher-quality US health care system. The variation in response to new knowledge among health care entities gives credence to the statement that medicine is both a science and an art. The art of medicine includes how organizations and individual physicians respond to external changes including new information and new technologies as well as financial incentives. This study uses the organizational theory and in particular Tichy’s descriptive framework of organizations consisting of three internal systems—technical, cultural, and political—to explain which substance abuse treatment organizations adopted a new medication to treat opiate addiction.5 The application of Tichy’s three internal systems may be particularly relevant in these organizations because of the well-documented philosophical differences in treating people with opiate addiction.6 To the authors’ knowledge, this is the first time that the Tichy framework has been used in a quantitative model depicting the adoption decision of substance abuse treatment organizations.
A Congressional amendment to the Controlled Substance Abuse Act in 2000 approved the use of buprenorphine to treat opiate addiction, and the Food and Drug Association (FDA) approval in 2002 allowed office-based physicians who participate in a brief training program and receive a waiver to prescribe buprenorphine to people with opiate addiction for detoxification or treatment. Despite numerous studies on the effectiveness of buprenorphine, adoption has been slower than expected. The consequences of underuse of this therapy are substantial for society, since buprenorphine has been shown to be more effective than counseling alone in reducing opiate addiction.7–9 It also provides an effective alternative to methadone maintenance, avoiding the burden of dispensing medications through a methadone treatment program, with the resulting potential to bring more people into treatment. In addition to personal consequences, opiate addiction is associated with increased criminal activity, increased morbidity and mortality (particularly related to human immunodeficiency virus infection/acquired immune deficiency syndrome, hepatitis, and tuberculosis), and increased unemployment. An National Institutes of Health Consensus Statement estimates that the cost of untreated opiate dependence is about $20 billion per year.10 Furthermore, treatment of addiction provides 1.3 to 23 times its medical costs in savings to society in terms of lower medical expenditures, lost productivity, and costs of criminal activity.11
Background on the diffusion of technology
The earliest models on the diffusion of medical knowledge and innovations used an epidemiological model in which early physician adopters influenced the decision of other physicians.12 There were no constraints, other than effective communication among well-informed physicians. This characterization, however, has been shown to be inadequate.13 Rogers’ seminal work found that a significant proportion of the rate of technological adoption by physicians depends on a number of factors, including the attributes of the innovation and how the innovation compares with the existing techniques.14 In addition, Rogers found that significant contributors to adoption include the technology’s compatibility with existing values and treatment norms, the complexity or difficulty of putting the innovation into practice, trialability or limited use at first, and the observability of outcomes.14
While individual physicians make the decision to prescribe, physician decisions are affected by health care organizations in the USA. Physicians, while striving to be autonomous, practice in an insured market environment. In this environment, health plans and health care organizations attempt to motivate physicians to adhere to their goals using tactics such as rules, drug formularies, and payment incentives; thereby, organizations have become critical in either encouraging or thwarting technology adoption.15
Thus, the rate of diffusion of new technologies in health care must be viewed as a complex process involving several highly interrelated levels of decision makers: individual physicians, treatment organizations, health insurance plans, and patients. Physicians’ adoption decisions are influenced by their treatment orientation, training and education, knowledge, attitudes, prior experience, and patient demographics and clinical characteristics. Furthermore, they are influenced by the organizations within which they work.16–18 At the organizational level, environmental pressures including market and regulations, treatment philosophy, resource constraints, service objectives, and patient mix influence decisions regarding the adoption of a new technology.19 These factors can influence not only organizational decisions to incorporate a technology or add a medication to its formulary but also the degree to which the organization encourages physicians to adopt them.
Focus of study
In this paper, we evaluate the adoption of a new evidence-based medication treatment for opiate dependent persons, buprenorphine (Suboxone®), by substance abuse treatment organizations. Buprenorphine was approved by the FDA in 2002 to treat opiate addiction in outpatient settings. Outpatient treatment facilities are particularly important for the treatment of substance use disorders, since only 13% of individuals who receive treatment do so in a private physician’s office.20 Varying treatment modalities are available to individuals with opiate addiction: medications (methadone or buprenorphine), outpatient counseling, and residential and 12-step programs requiring abstinence, although the most successful treatment modality is medication substitution.10 Methadone is the most commonly available substitution treatment for opiate addiction. However, the number of opiate-dependent individuals far exceeds the number of methadone maintenance slots, and in some states, methadone is not available at all.21,22
Buprenorphine has both clinical and nonclinical advantages over methadone,7–9 although abstinence occurs with both when used in conjunction with counseling. Buprenorphine is a partial opiate agonist as well as an opiate antagonist. As such, it has benefits over opiate agonists such as methadone, primarily in protecting against severe withdrawal symptoms when maintenance use is abruptly stopped and in reduced potential for overdose. In addition to these advantages over methadone, daily dosing in the presence of treatment staff is not required, removing the social stigma and work-related issues of going to a methadone center daily. Finally, clients report a better quality of life and safety with buprenorphine, from decreased lethargy to no detectable “high”.23,24
While disappointing to many supporters desiring better access to opiate treatment, the slow rate of adoption of buprenorphine is not surprising. An Institute of Medicine study in the area of substance abuse treatment recognized the need to build bridges to fill the gap between research and practice.25 Previous work on a new medication approved for alcohol use in the late 1990s, naltrexone, also showed significant underuse.18,26 While adoption was higher by physicians who worked in organizations that supported naltrexone, organizations per se were not the unit of analysis.18
In the current health services delivery system, including the specialty substance abuse sector, physician treatment decisions are influenced by the organizations in which they work. Organizations of any kind are complex systems, and successful adoption of innovations and thus new therapies depends upon varying features of health care organizations.27,28 This variation across complex organizations is likely to produce different reactions to external policies, including the adoption of new technologies. Previous studies of the acceptance of evidence-based clinical measures and of health organizations’ reactions to financial incentives have found significant variation at both the health insurance plan and physician practice levels.29–32 This paper seeks to understand the reasons for this variation using the organizational theory, as applied to substance abuse treatment.
Using organizational theory to help explain the variation in adoption
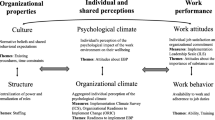
Organizational theorists have blended multiple insights into a comprehensive framework of organizational dynamics and how organizations respond to external changes. This framework builds on the historical work of technical and bureaucratic models of organizations and incorporates employee preferences and feedback between employees and organizations.33–38 One comprehensive conceptualization, which seems particularly relevant given the “art” of medicine, describes organizations as being comprised of three internal, intertwined systems that influence behavior and must be managed: a technical treatment production system, a social and cultural system, and a political system.5,39,40
Tichy used and developed this framework in the conduct of detailed case studies of organizations in a variety of industries, including electronics, banking, and health care.40 Though each one of the three elements of an organization was described as a “system,” Tichy found that together they reduced uncertainty by offering solutions to problems such as: How do we organize work? Who is responsible? What are our goals? What are our procedures? Who makes these decisions? How are we performing?
The technical system is designed to handle the day-to-day routines: processing information and problems to serve patients. In health care, the technical system resolves many clinical uncertainties including the competencies and role of the people, job and facility design, coordinating mechanisms, operating capacity, service performance, and quality management.
The social and cultural system inculcates assumptions, beliefs, and shared values into all participants who associate together,41 resolving many uncertainties about norms of behavior. Some core values embedded in the culture include a sense of ownership, mutual trust, risk taking, learning and innovation, concern for social justice, and perceptions of fairness. Generally, these norms and values guide social relationships, the way work is organized, the exercise of authority, rule following, rewards, and the acquisition of status.
There is also a political system that allocates power and influence, resolving uncertainties about decision rights, relationships that affect resource allocation, internal status and careers paths, and conflicts affecting the technical and cultural system.42 Inside every organization, the social arrangements also give rise to coalitions of powerful, influential people (stakeholders). The political system can influence whether or not decisions erupt, problems are solved cooperatively or by fiat, and conflicts are left to escalate into crises.
Tichy pointed out that some balance needs to occur across these three systems to achieve harmony inside an organization and that the three systems are unlikely to be of equal importance within an organization. One system may dominate the others, which is most likely to be observed when a critical capacity constraint or significant change in operations is being considered. For example, religious organizations are likely to have culture dominate, government agencies and unions are a good example of where the political system dominates, and business firms are often dominated by the technical system.5 However, separating the technical from the cultural and political systems is difficult because they are intertwined.
Tichy’s framework has been used recently to evaluate how hospitals responded to Medicare’s diagnosis-related group (DRG) system.43 This framework, however, has not been quantitatively assessed for outpatient treatment settings, perhaps because of the historical importance of physician autonomy and their conceived position as “captain of the ship.” However, substance abuse treatment offers an opportunity for conducting such a study, because of its reliance on treatment organizations rather than individual providers to serve people with addictive disorders. Moreover, Tichy’s three-system framework seems particularly relevant to understand the different behavior among substance abuse treatment providers due to the strong philosophical differences or values about the appropriate use of medication assisted treatment. For example, the major informal treatment system, the 12-step program, requires abstinence, and this philosophy is reflected in many formal treatment settings. Obviously, differences in the attitude towards substitution medications are reflected in different organizational cultures, and consequently, one would expect a differential organizational response with regard to using a medication like buprenorphine.28
This three-system organizational framework is useful in quantitative studies because it is a parsimonious way to understand complex organizations. Specific measures of these systems are used to analyze treatment organizations’ decisions to adopt buprenorphine. The technical, cultural, and political systems relevant to treatment organizations adopting a new medication are described briefly below, as are our major hypotheses regarding how these systems are likely to affect the adoption of buprenorphine.
Technical
A treatment center’s technical system, such as the organization’s size, capacity, and resources, affects an organization’s ability and willingness to adopt a new program.44 Thus, office-based treatment settings that are knowledgeable about the benefits of buprenorphine and have relevant processes and competency in treating addictions should make them more likely to embrace this medication in addiction treatment.
Cultural
The cultural system shapes the social norms of a treatment organization. An organization’s culture has been described as including attitudes, philosophy, and goals.45 Organizational culture has been shown to play a major role in determining the mix of services available at treatment centers.28,46 In particular, attitudes toward medications, either for detoxification or long-term treatment, vary sharply in substance abuse treatment organizations and are expected to be significant predictors of adoption.
Political
The political or power structure within an organization, particularly its leadership and process for decision making, determines the ability and willingness to adopt new programs.47,48 Physician “opinion leaders” have been used to explain variation in practices as well as the likely norms of professionally based organizations. An alternative, bottom-up perspective is client- or patient-driven. D’Aunno and Vaughn found that methadone treatment units serving higher percentages of younger, male, minority, and unemployed clients were less likely to receive the most recent treatments.49
It is hypothesized that all three systems are likely to be important in determining the likelihood that a substance abuse treatment program will adopt buprenorphine. The clinical superiority of buprenorphine should make those organizations with a technical capacity for medication-assisted treatment and knowledge of buprenorphine more likely to adopt. In addition, a supportive cultural system or positive attitude toward medication-assisted treatment would seem to be a necessary condition for adoption. Indeed, the cultural system may be the dominant one in this setting.
Data
To test the hypotheses relating organizational characteristics to buprenorphine use, a web-based survey was developed for program administrators. The survey included sections about the organization’s technical capacity (e.g., setting, scope of care, size of staff, for-profit status, knowledge of buprenorphine), culture (e.g., attitude toward medications, attitude about use of medications specifically for detoxification and maintenance of opiate addicts), and political (e.g., the leadership of the medical director, management structure, and characteristics of clients served). Treatment organizations were surveyed in four of the ten market areas with the highest rates of heroin use, with the intent of also attaining geographic and population diversity. The four survey locations were: Boston, Chicago, Miami, and San Francisco.
Facilities that offered outpatient substance abuse treatment within each market area were identified from the National Survey of Substance Abuse Treatment Services (N-SSATS) 2003 respondent sample.50 Facilities were ineligible if they did not provide outpatient substance abuse treatment; if they only treated driving under the influence or driving while intoxicated clients, if they only treated incarcerated clients, or if they did not have any medical staff and thus would be unable to prescribe buprenorphine. Letters were sent to all facilities inviting them to participate in the survey; a $25 honorarium was offered for completion. Follow-up letters and phone calls were conducted, and paper copies of the survey were provided if the identified person did not have access to the web or preferred not to use it.
The survey was conducted between September 2004 and January 2005. Thus, this study of diffusion is a cross-section at one point in time rather than a time series analysis. This survey took place 4 years after the legislation was passed that enabled buprenorphine to be prescribed in office practice and more than 2 years after FDA approval and marketing launch for this indication. The diffusion of medications occurs over time. However, the time path has largely been attributed to the level of knowledge among the provider community. Drug companies’ marketing efforts to inform physicians generally occurs soon after FDA approval, to achieve rapid diffusion. In the case of buprenorphine, significant efforts were made by the federal government to inform treatment providers about buprenorphine’s efficacy and advantages for the 2 years prior to this survey. To the extent that there are significant differences in the knowledge of buprenorphine among adopters and nonadopters, this cross-section analysis is reflective of what had occurred 2 years after introduction.
Of the 245 eligible or undetermined facilities, 87 could not be contacted to determine eligibility, 33 refused to participate, and 125 responded, for a response rate of 51% overall with little difference across the geographic areas. Using responder and nonresponder characteristics from N-SSATS 2003, which provided the sample frame, no significant differences were found between the two groups. Variables tested included state, treatment modalities available, services offered, ownership, availability of substance abuse medications, payment sources, managed care contracts, licensure, accreditation, and facility size (number of clients). Respondents were less likely to treat adolescents (p < 0.003), but by design, adolescent-only facilities were excluded. Respondents were also slightly more likely to have state funding as a payment source (p < 0.05).
While a higher response rate is clearly preferred for generalizability, this rate of response is commonly found in analyses of surveys of organizational administrators.51,52 The number of responding organizations was sufficient for testing the importance of the three internal systems in an exploratory study such as this.
Methods
The 125 responding facilities were matched to the 2003 N-SSATS data set, supplementing the survey data with information from that national survey. Domains for analysis were created reflecting the three organizational systems in Table 1. The third column in Table 1 indicates the four variables chosen as proxies for each of the three systems. These variables were chosen from the survey responses to provide a parsimonious representation of each system. They are highly correlated with other potential system proxies in the survey (not used in this analysis), and the correlation between the selected 12 proxies is low (the largest Pearson correlation coefficient is 0.42 for role of prescription drugs in treatment approach and knowledge of buprenorphine’s effectiveness).
A six-point scale was used to rate the response for most of the survey questions, ranging from 1 = not at all/very little to 6 = very much. The response used to classify facilities as buprenorphine adopters or nonadopters was the answer to the question, “How long has your organization been using buprenorphine?” to assure that all treatment organizations that ever used the medication were identified as adopters. This measure identified 26 out of 125 facilities in the sample as buprenorphine adopters (or 21%) and 99 as nonadopters (79%).
Bivariate and multivariate probit regression analyses were used to determine the importance of the technical, cultural, and political characteristics of organizations that adopted buprenorphine as compared to those that did not. Since bivariate analysis included response values that were dichotomous, ordinal, and continuous, chi-square, Wilcoxon, and t test statistics were used to test for significant differences. Stata/SE (v. 9.2) was used to estimate the probit regression model, providing maximum likelihood estimates of the parameters with robust standard errors, treating ordinal responses as continuous variables. The sample size for probit regression analysis, after accounting for missing values in various responses, included 87 facilities, of which 23 were adopters (or 26%, slightly higher than in the full sample) and 64 were nonadopters.
Results
Sample characteristics
More than half of the treatment organizations indicated that they were free-standing substance abuse treatment programs, while almost a quarter were housed within a hospital. Only one in 20 indicated that their treatment setting was a group practice. These organizations offered multiple services to their clients, including outpatient services (87%), intensive outpatient services (52%), and early intervention (38%). In addition, residential treatment and outpatient detoxification were offered by almost 30% of the organizations surveyed. Organizations stated they were best suited to serve alcoholic clients (85%), followed by the dually diagnosed (79%), other substance abusers (79%), heroin users (73%), and prescription opiate users (68%). The average years in operation was 18 (median of 20) with a standard deviation of nine years.
Adopting versus nonadopting organizations
Survey responses were tested for significant differences between identified adopters and nonadopters. Results for variables included in the probit regression are presented in Table 2.
Technical
Two of the four variables, knowledge of effectiveness and mean number of services, were significant at the p < 0.01 confidence level. In addition, the difference in mean total full-time equivalents (FTEs or scale of the operations) between adopters and nonadopters was marginally significant (p < 0.09). It is not surprising to note that clinicians in those organizations that had used buprenorphine were more aware of its effectiveness, with 14 of 23 adopting organizations indicating that its clinicians were well informed about buprenorphine (a 4 or higher on the scale). However, it was surprising that five of the entities adopting had limited knowledge (scoring themselves with a 1 or 2). If the larger number of staff is an indication of more in-house technical experience and the greater breadth of treatment options is an indication of more in-house technical knowledge, these attributes might create the favorable conditions necessary for the adoption of a new technology. Taken together, the adopting treatment organizations demonstrate the technical capacity and knowledge necessary to manage both clientele and their new medication.
Cultural
Three of the four variables representative of the cultural system indicate significant differences between the adopters and nonadopters (p < 0.05). Adopting organizations more strongly supported prescription medications in their treatment approach compared to the nonadopting organizations, with mean scores of 4.8 and 3.4. No treatment organizations adopting buprenorphine scored a 1 or 2 on this question, which would indicate a reluctance to use medications. In addition, adopters indicated that they more strongly encouraged the use of medications (mean scores 4.7 adopters and 3.05 nonadopters) to reduce craving. In addition, adopting organizations indicated stronger support of behavioral therapy (5.4 versus 4.8 for nonadopters). It is interesting to note that there was no significant difference between adopters and nonadopters with respect to encouraging abstinence (with scores of 5.7 and 5.3, respectively). These findings suggest that a treatment organization’s strategic choice regarding the adoption of buprenorphine is a reflection of the cultural system of the organizations, and in particular, it is influenced by the norms and values regarding treatment philosophy as it pertains to medication-assisted treatment.
Political
Two of the variables used to represent the political system had p values less than 0.05. The only significant differences between adopters and nonadopters were that adopters treated a greater percentage of white patients than nonadopters (58% vs. 38%) and that patient demand played a more important role in the decision making for adopters. No significant difference was found with respect to the extent that medical directors shared new information or with respect to the type of ownership (public vs. private). It is not surprising that adopters indicated greater responsiveness to consumer demand for buprenorphine; however, the importance of the percentage of white patients suggests that the characteristics of the population are significant. The percentage of white patients might be a proxy for those opiate-dependent patients who are likely to be employed, given significantly higher rates of employment and private insurance among whites, and who thus find the less frequent treatment visits particularly attractive.
Multivariate probit regression
All variables in Table 2 were included in the probit regression, with the dependent variable being a dichotomous indicator of adoption. Table 3 presents the coefficient estimates, marginal effects, and z scores for the probit regression predicting adoption of buprenorphine. The marginal effects reported are the average of the individual effects and thus yield an average change in the probability of adoption at the margin of the system characteristics. This provides a direct comparison of the importance of each characteristic in the organizations’ decision regarding whether or not to adopt buprenorphine.
Within the technical system, the coefficients of FTE, number of services, and knowledge of buprenorphine’s effectiveness were significant (with at least p < 0.05) with positive signs. The estimated marginal effects for these three are significant at p < 0.01, and the knowledge has the largest positive effect on adoption among the technical characteristics. Total FTEs, while significant, has a smaller marginal effect, suggesting that the scope or diversity of an organization’s treatment options is more important than its size for predicting the adoption of new technologies.
Two of the cultural variables have significantly estimated coefficients and marginal effects, and each has a larger impact on the probability of adoption than the significant technical variables in this model. For example, the marginal effect on the probability of adopting buprenorphine increases by 5.3% in organizations that encouraged the use of medications to reduce cravings. Similarly, the probability of adopting buprenorphine increases by 4.6% in response to increases in the degree to which prescription medications played a stronger role in substance abuse treatment. Neither of the variables representing encouragement of behavioral therapy nor abstinence was significant. This is not surprising as both adopters and nonadopters indicated strong support of both treatment approaches in the survey.
The political system proxies yielded only one significant characteristic. However, the marginal effect of an increased percent of white patients had a small effect on the probability of buprenorphine adoption, comparable to that of total FTE.
Discussion
The first hypothesis—that all three organizational internal systems would impact the adoption of buprenorphine—was supported by the quantitative findings. Variables representing each of the three systems were significant predictors of buprenorphine adoption.
Technical
Patients with opiate addictions are likely to be clinically and socially complex, with comorbid mental and physical conditions. Thus, having knowledge of the effectiveness and safety of buprenorphine was found, in general, to be of significance. In addition, the treatment organization must have the ability to manage or triage these patients and, ideally, to coordinate their care. Thus, substance abuse treatment organizations in our survey that had a high level of knowledge regarding buprenorphine’s effectiveness, greater scope of services (specifically inpatient and outpatient detoxification, mental and general health services), and more FTEs were more likely to adopt buprenorphine. While physician knowledge of effectiveness and an organization’s positive attitude toward medications are important, physicians are dependent on structural and procedural supports in their office settings to allow for the necessary buprenorphine induction and follow-up.
Cultural
Substance abuse treatment organizations vary in their treatment philosophy. The most critical factor that affects the organization’s culture is related to the role of medications; it is recognized in the treatment community that this ideology has a bimodal distribution, with sharply demarcated opinions on the role of medication in achieving recovery and, indeed, in the definition of recovery itself and the importance of harm reduction.6,53
Political
Although the political system was less important in this analysis, the fact that patient race/ethnicity was significantly associated with adoption suggests that there may be underlying political barriers to the use of buprenorphine. Being nonwhite is likely to be a proxy measure for socio-economic status, employment status, and insurance status in a drug treatment setting. In another study offering office-based buprenorphine treatment, it was found that those clients had significantly different demographics and substance abuse characteristics than did methadone maintenance clients in the same community.54 The findings of the current study suggest that office-based buprenorphine treatment will attract different individuals than methadone maintenance treatment programs and treatment organizations that serve the unemployed or those without private insurance will be less motivated to adopt buprenorphine.
The second hypothesis was that the cultural system would be the dominant system in determining the adoption of buprenorphine. The results support this hypothesis, showing that the attitude toward the use of medications for addiction treatment was the most important variable, but clearly, attitude and knowledge of a medication’s effectiveness go hand-in-hand. The bivariate and multivariate results showed the technical and cultural systems were both considerably more important than the political system. While the magnitude of the marginal effect size for the specific measures included for the technical and cultural systems were comparable, two of the cultural variables, the role of prescription drugs in treatment approach and the use of medications to reduce craving, had the highest marginal values in the predictive, multivariate probit regression (see Table 3). Moreover, the actual rankings provided by the treatment sites on the technical and cultural system measures—knowledge of buprenorphine’s effectiveness and attitude toward medications—provide the strongest case for the cultural system being dominant. In particular, while adopting organizations ranked their knowledge of buprenorphine throughout the six-point range (with five organizations having a score of 3 or less), none of the adopting organizations ranked themselves either a 1 or 2 with regard to their attitude toward medications. Thus, it appears that significant awareness of buprenorphine’s effectiveness is not a necessary condition for adoption, yet a positive attitude toward medication-assisted treatment is necessary.
Implications for Behavioral Health
The finding that the cultural system, as measured by a positive attitude toward addiction treatment medications, was a highly influential condition for the adoption of buprenorphine, suggests that the availability of even better medications, in terms of side effects or ease of delivery, may have little impact on many substance abuse treatment programs in the USA. Moreover, when an addiction treatment organization is financially viable and fulfilling its core mission while maintaining deeply held beliefs about abstinence, altering its treatment or production regimens is very unlikely. Even when Congress passed legislation permitting buprenorphine to be used for opiate treatment in outpatient settings, about three quarters of the treatment organizations (in the four large metropolitan areas surveyed) chose not to adopt buprenorphine 4 years after the legislation.
The epidemiological model of the diffusion of technology, which is grounded in the technical system, suggests that new evidence-based treatments that provide an improvement over existing practice will be preferred, and thus diffusion will occur over time following a predictable pattern. For substance abuse treatment organizations, the prevailing belief at many treatment sites is that medication-assisted therapy is not consistent with recovery.6 This cultural position is an obstacle to medication-assisted treatment. While more than 80% of the adopting organizations scored the role of medications in treatment at 4 or higher (out of 6), this was true for only half of the nonadopters. This difference in attitude about the appropriate use of medications suggests that the widespread diffusion of buprenorphine is unlikely to occur under the existing operating policies of the outpatient treatment system. This finding is also likely to hold true for all the improved medications for substance abuse currently under development. The adoption behavior of addiction treatment organizations will not change unless the philosophy of outpatient treatment organizations is altered.
Given both the high cost imposed on society by a low level of adoption of improved evidence-based addiction treatments and the high levels of public funding for these organizations, exceptional efforts are needed by the government to encourage adoption. A policy of simply educating treatment providers about the benefits of new medications is not enough given prevailing cultural attitudes about the use of medications in the specialized substance abuse treatment system. At the same time, requiring all publicly funded treatment organizations to adopt buprenorphine has the risk of destabilizing the addiction treatment system. Choosing a public policy that lies between educating and requiring seems to be the preferred strategy. The government needs to give more direction or “voice” to accomplish cultural change and responsiveness within treatment organizations. Making some percentage of federal funding contingent on the use of medication-assisted therapy or other evidence-based measures to reduce opiate addiction among their clients is another alternative. Under either policy scenario, the government would recognize the role of organizations in the successful diffusion of evidence-based medicine and would be adopting policies that have the flexibility to address organizational differences in cultural, technical, and political systems.
One important initiative through the private sector in promoting the diffusion of new technologies in the substance abuse field is the Advancing Recovery program, a collaboration between the Network for the Improvement of Addiction Treatment, the Treatment Research Institute, the Robert Wood Johnson Foundation, and six payer–provider partnerships.55 This program provides support to states to work with providers to promote the use of evidence-based practices. Recognizing the importance of organizations and the political context within which they exist, Advancing Recovery aims to “improve clinical and administrative practices that impede the use of evidence-based practices.” A major focus is the use of medication-assisted treatment.
The significant barrier posed by the prevailing cultural system in addiction treatment organizations for medication adoption cannot be generalized to all health care organizations. However, by analyzing an area of medical care where treatment organizations are critical in influencing physician practice patterns, the importance of substance abuse treatment organizations’ attitudes are made evident. The complexity of organizations and the interplay of medical organizations with their independent professionals, particularly physicians, necessitates that policies reflect an understanding of organizational capabilities and beliefs and the variations in these factors among organizations. What this study has shown in terms of the readiness to adopt a more effective treatment is symptomatic of how substance abuse treatment organizations will respond to a host of changes imposed upon them.
The importance of these findings for the treatment of opiate dependence and abuse and other substance abuse problems in the USA is clear. Policymakers, both public and private, need to understand the conditions under which the availability of new services and modes of treatment or other changes in the environment are likely to lead to behavioral changes in addiction treatment organizations. Treatment organizations must constantly evolve, and the decision to do so may be internal or may come from outside the organizations. However, the desired response of an organization to external policies is not automatic. Substance abuse treatment organizations weigh the rewards against the cost and benefits of changes for their organizations: When the required changes are at odds with the prevailing culture, capacity, or clientele, the change may be rejected or be very difficult to realize. The variation in adoption of substance abuse medications by treatment organizations has a direct relation to physician practice patterns. In a partner survey of physicians conducted as part of this research, physicians affiliated with organizations supportive of buprenorphine were more likely to prescribe it, and for nonprescribers as well as prescribers, attitudes toward buprenorphine were associated with the affiliated organization’s support of its use.56 As well, in a 2002 survey of adoption of naltrexone for alcoholism treatment, physicians were significantly more likely to prescribe the medications if their organizations were supportive of its use.18
The variation in organizational responses to the changes in their external environment is not restricted to new substance abuse treatment technologies. For example, when national payment policies for Medicare were established, such as DRG payments to hospitals and capitation payments to health plans, these health organizations did not respond uniformly. Administered payment systems seem to be based on the idea that health care organizations are simply a technical system that translates inputs into outputs and therefore can change their inputs readily to meet the desired policy outcomes. The reaction to many specific quality measures varies across health care plans and delivery systems, as do the responses of medical organizations to undertaking specific actions in pay-for-performance programs.31
Thus, the findings in this paper on the variation in adoption of a new medication for opiate addiction are consistent with other studies that have evaluated how health care organizations responded to external changes. The willingness and ability of organizations to change their practice’s behavior will vary according to an organization’s history, culture, and technical and political systems.5,39,40 For the social goals of improved quality, efficiency, and effectiveness to be realized in substance abuse treatment, policymakers need to adopt policies that recognize the importance of the influence of organizations in physician practice, as well as the differences among organizations. The inclusion of how organizations will react to policy approaches will, in turn, allow substance abuse treatment organizations to meet the objectives by taking actions that best fit their technical, cultural, and political internal systems.
References
Newhouse J. How much welfare loss? Journal of Economic Perspectives. 1992;6(3):3021.
Belongia EA, Schwartz B. Strategies for promoting judicious use of antibiotics by doctors and patients. British Medical Journal. 1998;317(5):668–671.
Ma J, Sehgal N, Ayanian JZ, et al. National trends in statin use by coronary heart disease category. PLoS Medicine. 2005;2(5):e123.
Stafford RS, Monti V, Ma J. Underutilization of aspirin persists in US ambulatory care for the secondary and primary prevention of cardiovascular disease. PLoS Medicine. 2005;2(12):e353.
Tichy NM. Networks in Organizations. New York: Oxford University Press; 1981.
Ducharme LJ, Knudsen HK, Roman PM. Evidence-based treatment for opiate-dependent clients: availability, variation, and organizational correlates. The American Journal of Drug and Alcohol Abuse. 2006;32:569–576.
Bickel WK, Stitzer ML, Bigelow GE, et al. A clinical trial of buprenorphine: comparison with methadone in the detoxification of heroin addicts. International Journal of Clinical Pharmacology and Therapeutics. 1988;43:72–78.
Johnson RE, Jaffe JH, Fudala PJ. A controlled trial of buprenorphine treatment for opioid dependence. Journal of American Medical Association. 1992;267:2750–2755.
Kosten T, Schottenfeld R, Ziedonis D, et al. Buprenorphine versus methadone maintenance for opioid dependence. Journal of Nervous and Mental Diseases. 1993;181:358–364.
National Institutes of Health. National consensus development panel on effective medical treatment of opiate addiction, Effective medical treatment of opiate addiction. Journal of American Medical Association. 1998;280(22):1936–1946.
McCollister KE, French MT. The relative contribution of outcome domains in the total economic benefit of addiction interventions: a review of first findings. Addiction. 2003;98(12):1647–1659.
Coleman JS, Katz E, et al. The diffusion of an innovation among physicians. Sociometry. 1957;20:253–270.
Starbuck WH. Organizations and Their Environments. Chicago, IL: Rand McNally; 1976.
Rogers E. Diffusion of Innovations, 5th Edition. New York: Simon & Schuster; 1995.
Kadushin C. Frontiers of Research in Network Theory and Method. New York: CUNY Graduate Center; 1979.
Chilingerian JA, Glavin M. Temporary firms in community hospitals: elements of a managerial theory of clinical efficiency. Medical Care Research and Review. 1994;51:289–335.
Fendrick M, Schwartz JS. Physicians’ Decisions Regarding the Acquisition of New Technology. Washington, DC: National Academy; 1994.
Thomas CP, Wallack S, Lee S, et al. Research to practice: adoption of naltrexone in alcoholism treatment. Journal of Substance Abuse Treatment. 2003;24:1–11.
Scott WR. The organization of medical care services: toward an integrated theoretical model. Medicare Care Review. 1993;50(3):271–303.
SAMHSA. Results from the 2004 National Survey on Drug Use and Health: Detailed Tables. Accessed online: http://oas.samhsa.gov/NSDUH/2k4nsduh/2k4tabs/2k4tabs.pdf 2006.
McCarty D, Frank RG, Denmead GC. Methadone maintenance and state Medicaid managed care programs. The Milbank Quarterly. 1999;77(3):341–362.
Office Of Applied Studies, eds. Substance Abuse and Mental Health Services Administration. N-SSATS 2004 (United States). Arlington, VA: Synectics for Management Decisions (producer); Ann Arbor, MI: Inter-university Consortium for Political and Social Research (distributor); 2005:11–14.
Jasinski DR, Pevnick JS, Griffith JD. Human pharmacology and abuse potential of the analgesic buprenorphine: a potential agent for treating narcotic addiction. Archives of General Psychiatry. 1978;35(4):501–516.
Law PD, Bailey JE, Allen DS, et al. The feasibility of abrupt methadone-buprenorphine transfer in British opiate addicts in an outpatient setting. Addiction Biology. 1997;2:191–200.
Institute of Medicine. Bridging the Gap Between Practice and Research: Forging Partnerships with Community-based Drug and Alcohol Treatment. Washington, DC: National Academy; 1998.
Mark TL, Kranzler HR, Song X, et al. Physicians’ opinions about medications to treat alcoholism. Addiction. 2003;98:617–626.
Etzioni A. A Comparative Analysis of Complex Organizations. New York: Free; 1961.
Roman PM, Johnson JA. Adoption and implementation of new technologies in substance abuse treatment. Journal of Substance Abuse Treatment. 2002;22:211–218.
Conrad DA, Christianson JB. Penetrating the “black box”: financial incentives for enhancing the quality of physician services. Medical Care Research and Review. 2004;61(3 Suppl):37S–68S.
Institute of Medicine. Crossing the Quality Chasm, A New Health System for the 21st Century. Washington, DC: National Academy; 2001.
Rosenthal MB, Frank RG, Zhonghe L, et al. Early experience with pay-for-performance from concept to practice. Journal of American Medical Association. 2005;294(14):1788–1793.
Shortell SM, Zazzali JL, Burns LR, et al. Implementing evidence-based medicine the role of market pressures, compensation incentives, and culture in physician organizations. Medical Care Research and Review. 2001;39(7, Physician–System Alignment Supplement):162–178.
Argyris C, Schon DA. Organizational Learning. Reading, MA: Addison-Wesley; 1978.
Cyert RM, March JG. A Behavioral Theory of the Firm. Englewood Cliffs, NJ: Prentice Hall; 1963.
Granovetter M. Economic action and social structure: the problem of embeddedness. American Journal of Sociology. 1985;91:53–81.
Lawrence PR, Lorsch JW. Organization and Environment. Boston, MA: Graduate School of Business Administration, Harvard University; 1967.
March JG, Simon HA. Organizations. New York: Wiley; 1958.
Taylor FW. The Principles of Scientific Management. New York: Harper & Row; 1947.
Tichy NM. Managing Strategic Change. New York: Wiley; 1983.
Tichy NM, Devanna MA. The Transformational Leader. New York: Wiley; 1990.
Schein E. Organizational Culture and Leadership. 2nd edn. San Francisco, CA: Jossey-Bass; 1997.
Bacharach SB. Power and Politics in Organizations. San Francisco, CA: Jossey-Bass; 1980.
Chilingerian JA. Origins of DRGS in the United States: a technical, political and cultural story. In: Kimberly J, ed. The Globalization of Managerial Innovation: The Interplay of Politics, Policy and Functionality in Health Care. Cambridge: Cambridge University Press; 2008.
March JG. Ambiguity and Choice in Organizations. Bergen, Norway: Universitetsforlaget; 1976.
Schein E. What is culture? In: Frost PLM, Lousi M, Lundberg C, Martin J, eds. Reframing Organizational Culture. Thousand Oaks: Sage; 1991:10.
Willenbring ML, Kivlahan D, Kenny M, et al. Beliefs about evidence-based practices in addiction treatment: a survey of Veterans Administration program leaders. Journal of Substance Abuse Treatment. 2004;26:79–85.
Cohen MD, March JG. A garbage can model of organizational choice. Administrative Science Quarterly. 1972;17:1–25.
House R, Baetz M. Leadership: some empirical generalizations and new research. In: Staw B, ed. Research in Organizational Behavior. Greenwich: JAI; 1979:341–423.
D’Aunno T, Vaughn TE. Variations in methadone treatment practices. Results from a national study. Journal of American Medical Association. 1992;257(2):281–282.
Office of Applied Studies, eds. Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS): 2003. Vol DASIS Series: S-24: Data on Substance Abuse Treatment Facilities; 2004.
Gittell JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Management Science. 2002;48(11):1408–1426.
Gittell JH, Fairfield K, et al. Impact of relational coordination on quality of care, post-operative pain and functioning, and length of stay: a nine hospital study of surgical patients. Medical Care. 2000;38(8):807–819.
Marlatt GA. Harm reduction: come as you are. Addictive Behaviors. 1996;21(6):778–788.
Michaels J, Galanter M, Resnick R, et al. Community based heroin addicts who turn to experimental treatment rather than conventional care. Journal of Addictive Diseases. 1995;14(2):33–42.
Advancing Recovery. www.advancingrecovery.net. Accessed March 3, 2008.
Thomas CP, Reif S, Haq S, et al. Adoption of buprenorphine by psychiatrists and addiction specialists: results of a national survey. Psychiatric Services (in press).
Acknowledgments
This organizational analysis was one of studies conducted under a grant from NIH, NIDA R01DA014578. The NIDA project officers, Drs. Jerry Flanzer and Richard Denisco, have provided encouragement on understanding the impact of treatment organizations. Of course, we take full responsibility for the conduct of the study and interpretation of the findings. NIDA had no role in the conduct of the study, data collection, management, analysis, and interpretation of the data, or the preparation, review, or approval of the manuscript. A number of our colleagues contributed to the survey design, web-based collection of information, and creation of the analytical files. We wish to thank ElizabethTighe, Ph.D., Brandeis University, as well as Sayeda Haq and Alex Hoyt, Ph.D. candidates. Grant Ritter, Ph.D. provided assistance on the sampling frame, survey instrument, and variable construction. Wendy Colnon provided assistance throughout the study, and Sarita Bhalotra, M.D., Ph.D. made numerous contributions to the study. Finally, we would like to thank Jody Hoffer Gittell, Ph.D. for her substantive comments on an earlier draft. Tim Martin, Ph.D. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analyses.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wallack, S.S., Thomas, C.P., Martin, T.C. et al. Substance Abuse Treatment Organizations as Mediators of Social Policy: Slowing the Adoption of a Congressionally Approved Medication. J Behav Health Serv Res 37, 64–78 (2010). https://doi.org/10.1007/s11414-008-9132-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-008-9132-4