Abstract
Clubhouses and consumer-run drop-in centers (CRDIs) are two of the most widely implemented models of consumer-centered services for persons with serious mental illness. Differences in structure and goals suggest that they may be useful to different types of consumers. Information on what types of consumers use which programs would be useful in service planning. This study analyzes data from the authors’ NIMH-funded research on 31 geographically matched pairs of clubhouses and CRDIs involving more than 1,800 consumers to address the following question: are there significant differences in the characteristics and outcomes of members of clubhouses versus CRDIs? Results from multilevel analyses indicated that clubhouse members were more likely to be female, to receive SSI/SSDI, to report having a diagnosis of schizophrenia, and to live in dependent care; and they reported both a greater number of lifetime hospitalizations and current receipt of higher intensity traditional MH services. Controlling for differences in demographic characteristics, psychiatric history, and mental health service receipt, clubhouse members also reported higher quality of life and were more likely to report being in recovery. CRDI consumers were more likely to have substance abuse histories. Possible reasons for the differences are discussed. The results suggest that CRDIs are a viable alternative to more traditional mental health services for individuals who might not otherwise receive mental health services.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since the beginning of deinstitutionalization in the 1960s and the ex-patient movement of the 1970s, mental health consumers have become increasingly involved in mental health service provision at a number of different levels. Consumers have worked as advocates fighting for systems change, developed peer-led self-help groups, been hired as case managers (CM) and counselors within mental health service agencies, and established services run completely by and for consumers.1,2 In recent years, consumer-centered services have played an increasingly important role in the array of publicly funded mental health and support services that are available. Consumer-run drop-in centers (CRDIs) are one of the most common group-based types of these programs and are becoming increasingly more important as an option in the continuum of publicly funded mental health and support services.
The interest in CRDIs is evident in the abundance of information available about CRDIs in journals and on the Internet; however, relatively few of these sources provide empirical information about the characteristics of users of CRDIs, and even fewer compare CRDI users to those who use other types of consumer-centered services. Such studies could provide important information to consumers, their families, and other service providers. This study begins to fill this gap by describing the characteristics of consumers from 31 CRDIs in Michigan and comparing them to members of 31 clubhouses serving individuals in the same geographic areas.
Consumer-centered services focus on consumers’ needs and goals, as defined by the consumer. In this regard, CRDIs and clubhouses are similar. However, basic differences in the structure and goals of CRDIs and clubhouses suggest that they may serve different types of consumers. What follows is a review of the sample characteristics of a small number of studies of CRDIs and self-help programsFootnote 1 as well as studies of clubhouses. This review suggests differences between the two sets of users—patterns upon which the hypotheses for this study are based.
Some studies indicate that the characteristics of individuals who use CRDIs and clubhouses closely match the population of adults with serious mental illnesses in the public mental health service system.3–7,10–13,22 For example, there is a higher proportion of males than females in the population as a whole. On average, adults with serious mental illness in general and those attending CRDIs and clubhouses are in their late thirties and early forties, and about half have a high school education or less. The racial and ethnic mix of the programs generally reflects the geographic location of the program.3–7 However, some other research, although limited, indicates differences. First, compared to CRDIs, clubhouses appear to have an even larger preponderance of men.7–10 Second, consumers in clubhouses seem more likely to have or report having a psychiatric diagnosis with the diagnosis reported most often being schizophrenia.7,11–13 Consumers in CRDIs seem to be more often diagnosed with affective disorders, personality disorders, and/or substance abuse disorders.4,6
These differences in gender distribution and diagnoses may be related to differences in the focus and structure of CRDIs versus clubhouses. The main goal of CRDIs is to provide a safe and supportive environment where consumers with a history of psychiatric problems or high risk for psychiatric hospitalization can develop a peer support network. CRDIs do this by providing social and recreational activities, both organized and informal, and a forum for consumers to help each other with problems of daily living. They emphasize the shared experience of mental illness and acceptance of individuals as valued and respected members of a community. Clubhouses are more routinized than CRDIs, revolving around the “work ordered day” with a greater focus on vocational rather than other rehabilitative goals. This greater vocational focus may be related to the higher proportion of men in clubhouses compared to CRDIs. Similarly, the nature of schizophrenia, in particular a greater need for predictability and daily routine, may make the relatively structured routine in clubhouses more appropriate for these consumers, whereas the less-routinized CRDIs may be more consonant with the needs of those with a diagnosis of personality disorder or substance abuse.
In addition, in CRDIs, the program is run by service users. In contrast, clients in clubhouses (members) take part in the operation of the program, but the ultimate decision-making authority rests with the staff who are most often not mental health consumers themselves.
To compare the characteristics of users of CRDIs and clubhouses, this study focuses on six domains: demographic characteristics, psychiatric history, disability status, current service usage, symptomatology, and personal outcome variables. Based on the literature reviewed, the following hypotheses are proposed:
-
1.
Consumers in clubhouses are more likely to be men than women, but there will be no differences in age, education, or race/ethnicity.
-
2.
Consumers in clubhouses are more likely to have a diagnosis of schizophrenia than those in CRDIs.
-
3.
Consumers in CRDIs will have had less interaction with traditional mental health and support services including fewer hospitalizations and lower intensity of mental health service usage, and they are less likely to currently reside in supervised living arrangements.
In addition to these hypotheses, the question of whether a greater proportion of consumers in either program model would consider themselves “in recovery” is examined. Recovery in the context of mental illness and for the purposes of this paper is defined as a process that is personal in nature29 and is operationalized in terms of functioning or community adjustment rather than as an absence of psychiatric symptoms.7,30
Methods
This study uses a multilevel analysis strategy with hierarchical linear modeling (HLM) software with cross-sectional data from an NIMH-funded grant, Assessing Consumer-centered Services (ACCS) (#R24 F003470). Data were originally collected to develop fidelity criteria and measures for CRDIs; for comparative purposes, parallel data were collected from clubhouses serving the same geographic areas (see Mowbray et al.14 for additional information). Data collection took place at 31 CRDI centers and 31 clubhouses located in diverse geographical areas of the state of Michigan. All programs had been in operation for at least 2 years. To ensure that the samples of CRDIs and clubhouses were similar on community-level variables, each drop-in was matched to a clubhouse within the same geographic location. Of 45 CRDIs in Michigan that had been in operation 2 years or more, 31 could be geographically matched with a clubhouse serving the same area. All 31 clubhouses and 31 CRDIs were funded by the public mental health system, under the auspices of local county community mental health (CMH) boards. The total sample of CRDIs and, consequentially, clubhouses, had an equal distribution of urban and rural locations (59.7% urban and 40.3% rural). Because programs did not keep formal attendance records, directors at each site were asked to estimate how many members come to the program on a typical day. For clubhouses, the median number served per day was 30 with a range of 12 to 90. For CRDIs, the median number served per day was 22 with a range of 5 to 103.
Procedures
In-person site visits by a research team of three trained project staff members were made to each clubhouse and CRDI center; each visit lasted 2 days. Data for this paper came from consumer interviews conducted during these visits; 787 consumers were interviewed in CRDIs and 892 in clubhouses.
The site visits were arranged in advance and were publicized through flyers posted at each program. At the beginning of the site visit, the field research director gave a short, informal, friendly introduction to the group of consumers present to provide an overview of the purpose of the visit and to put them at ease with the presence of the research team as well as with the data collection procedures. In appreciation for their participation, each program received $100 compensation.
All consumers in attendance during the site visit were given the opportunity to complete a questionnaire and were paid $5 for their participation. Consumers chose whether they wanted to self-administer the questionnaire (53%) or complete it as an interview with one of the field research team (47%). Ten percent of consumers at the clubhouses and 9% at CRDIs refused to be interviewed. The questionnaire/interview encompassed: demographics, psychiatric history (including diagnosis), disability status, current mental health and support services, current symptomatology, self-reports of personal experiences, and questions about consumers’ involvement with and assessment of their programs.
Measures
Demographic data
Data collected included date of birth, sex, race/ethnicity, and level of education (1 = less than high school, 2 = high school or equivalent, 3 = vocational or technical training, 4 = some college, 5 = graduated college). Consumers were also asked how long they had been attending the program (1 = a few weeks, 2 = a couple of months, 3 = more than 6 months, 4 = over a year); to ensure that respondents had reasonable familiarity with the program, analyses were limited to those who had attended more than a few weeks (92.3% of those who completed questionnaires).
Psychiatric history
Information was based on these questions: “Has anyone ever told you that you had a drug or alcohol problem?” (yes/no); “Counting all the times in your life, how many times have you ever been hospitalized for mental problems?” (from “0” to “more than 10”); “How old were you when you were first hospitalized or first saw a psychiatrist?”
Diagnosis
Participants were asked, “What name best describes your mental illness diagnosis?” Answers were coded as psychotic disorder, depression, bipolar disorder, anxiety-related disorder, any other mental/emotional disorder, or a medical disorder. Out of 1,835 respondents, 564 (or 30.7%) failed to specify a diagnosis.
Psychiatric disability
Participants were asked if they received Social Security Income or Disability Income (yes/no). “Do you have a mental illness?” was an item from the Recovery Attitude Questionnaire with “yes/no/don’t know” responses; the latter two were coded as “no.”18
Mental health and support services
Participants were considered to be in a supervised living situation if they indicated they were currently living in a group home, adult foster care, or supervised/supported housing. Service use level was based on participants’ answers as to the number of times they saw a doctor/nurse about mental health medications or saw their CM/therapist during the last 30 days (1 = no contacts, 2 = only saw doctor/nurse, 3 = CM/therapist once, 4 = CM/therapist twice, 5 = CM/therapist three times, 6 = CM/therapist four or more times).
Current symptomatology
Symptomatology was assessed using the Colorado Symptom Inventory (CSI),15 which is comprised of 15 items addressing symptoms of anxiety, depression, and psychosis, each rated as “not at all,” “a little,” or “a lot” (e.g., “How often do you feel nervous, tense worried, frustrated or afraid?,” “How often do you feel depressed?,” “How often do you hear voices or hear or see things that other people don’t think are there?,” “How often do you feel out of place or like you don’t fit in?”) (α = 0.90).
Personal outcomes
Global Quality of Life16 was measured using a single question (“Which of the following best describes how you feel about your life as a whole?”) presented at the beginning and end of the questionnaire with response options from 1 = terrible to 7 = delighted; responses to the two questions were averaged to produce a single score. The State Hope Scale17 measures hopefulness and optimism (six items; four-point scale: 1 = definitely false to 4 = definitely true; e.g., “Right now I see myself as being pretty successful,” “At the present time, I am energetically pursuing my goals”; α = 0.81). The extent to which consumers believed they are in recovery was measured using a single item (“Do you consider yourself to be in recovery from a mental health problem?”; 1 = yes, 0 = no/don’t know), which was taken from the Recovery Attitude Questionnaire.18
Analysis plan
Analyses were conducted using data from respondents who had been in attendance at their program for more than a few weeks (N = 892 or 93% of those interviewed from clubhouses and 787 or 90% from drop-in centers). A multilevel analysis strategy was used to reflect the fact that participants were nested within 62 individual programs and to appropriately handle variables at 2 levels—program attributes and consumer characteristics. Consumers at CRDIs and clubhouses were compared on a series of characteristics, using random effects analysis of covariance (ANCOVA).19 Using random effects ANCOVA, the group effect (in this study, variability among the 62 individual programs) on a dependent variable (e.g., a consumer characteristic) was conceived as random with individual program means varying around a grand mean. The effect of program type (CRDI versus clubhouse) was reflected in the analysis as a fixed effect at the program level, and the effects of potentially confounding consumer characteristics (e.g., demographics) were incorporated as fixed covariates at the consumer level. Analyses were done with the HLM software using full maximum likelihood estimation.20 Generalized HLM was used to estimate models involving nonnormally distributed dependent variables; the Bernoulli link function was used for dichotomous dependent variables (e.g., sex) and the multinomial link function for polychotomous variables (e.g., diagnosis).
We conducted the analyses in an ordered, hierarchical fashion, whereby theoretically ordered blocks of consumer characteristics were tested for differences by program type and then incorporated as covariates (i.e., control variables) in subsequent ANCOVAs, thereby reducing redundancy of findings because of correlations among consumer characteristics. Blocks of dependent variables were ordered by increasing mutability—that is, relatively unchanging, historical variables were in early blocks and more malleable, current variables in later blocks. Thus, the analysis allowed for statistical control of the effects of stable characteristics (e.g., for consumer age, race, and sex) when testing for program type differences on more mutable characteristics (e.g., symptomatology and quality of life). The initial block contained consumer demographics (age, race, sex, and education). The second block contained psychiatric history variables (substance abuse history, lifetime hospitalizations, age at mental illness onset, and diagnosis). These were followed by blocks in this order: psychiatric disability (self-identified mental illness, receipt of SSI/SSDI), mental health and support services (service intensity, supervised living), symptomatology, and personal outcomes (State Hope, recovery orientation, and quality of life). ANCOVAs on individual psychiatric history variables controlled for the effects of demographics; ANCOVAs on psychiatric disability variables controlled for both demographics and psychiatric history, and so on; ANCOVAs on personal outcome variables controlled for all of the consumer characteristics in previous blocks. To verify the robustness of findings to the influence of the control variables, random effects ANOVAs by program type were also performed on all consumer characteristics without covariates; findings were generally consistent with the ANCOVA results presented below. In addition, the method of completing the questionnaire was included in the analysis as a control variable but was dropped from the final models because, although interviews were more common in CRDIs, the method was not significantly related to any of the outcome variables.
Results
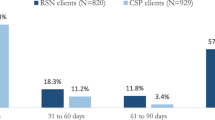
Characteristics of consumers in clubhouses and CRDI centers are presented in the left-hand columns of Table 1. The first four columns in the table present the averaged, within-program means and standard deviations (for continuous variables) and percents and subgroup ns (for categorical variables) for clubhouse and CRDI consumers. The remainder of Table 1 presents the results of the random effects ANCOVAs utilized to determine the extent to which consumer characteristics at the two types of programs differed significantly. In the table, positive coefficients indicate that a particular consumer characteristic was associated with clubhouse membership, whereas negative coefficients indicate associations with CRDI membership. Odds ratios are presented for dichotomous and categorical variables. The first block of analyses (ANOVAs with no covariates), reported in the first four rows, focuses on demographic variables. Clubhouses and CRDIs differed significantly on the sex of participants with those coming to CRDIs significantly more likely to be males. However, according to the analyses, clubhouse members did not differ from CRDI members on any other demographic variables (age, race, or education).
The second block of ANCOVAs, labeled psychiatric history variables, is reported in the next section of the table (six rows). According to these analyses, clubhouse membership is a significant negative predictor of having a substance abuse problem and a significant positive predictor of number of lifetime hospitalizations and of having a schizophrenia diagnosis. Interpreting the odds ratios, members of clubhouses (versus CRDIs) are only about 60% as likely to have had a substance abuse problem and more than two times as likely to report a schizophrenia diagnosis as are consumers at CRDIs. These findings take into account controls for the demographic characteristics (age, race, sex, and education).
The ANCOVAs in the third block examine psychiatric disability variables. Both disability variables are significantly predicted by program type, even after controlling for demographics and psychiatric history. Members in clubhouses are nearly twice as likely to report having a mental illness and more than three times as likely to be on SSI/SSDI as consumers at CRDIs. The next block of ANCOVAs involves current service use variables, controlling for variables from the previous three blocks. Both supervised living arrangement and current service intensity are predicted by program type. Individuals receiving services from clubhouses are getting more intensive services and are about three times more likely to be living in a supervised setting (group home, supported housing, etc.).
In the fifth block of ANCOVAs, program type differences on current symptomatology is examined, controlling for the previous blocks of variables. There is no significant difference between consumers in the two types of programs. In the last block, the analyses examine differences by program type on personal outcome variables, controlling for variables from all previous blocks. Program type is significantly predictive of recovery orientation and quality of life, but not of the State Hope Scale score. Consumers in clubhouse programs self-report a significantly higher quality of life and are also about one and a half times more likely to say they are in recovery from mental illness as were those in CRDIs; this association controls for consumers’ report about whether they have a mental illness and for other psychiatric history, disability, symptomatology, and service use variables.
Discussion
The analyses reported used cross-sectional data to provide a snapshot of the differing characteristics of users of two publicly funded program models, clubhouses versus CRDI centers, in the same geographic locations—all within the State of Michigan. Based on a few limited and separate studies, hypotheses were presented of the expected differences, which were partially supported, as follows.
Hypothesis 1 stated that consumers in clubhouses are more likely to be men than women, but there would be no differences in age, education, or race/ethnicity. The analyses found no differences on any of the demographics except sex. Both programs appear to involve consumers whose characteristics match those typical of a population with serious mental illnesses. That is, as reported in research on CRDIs, clubhouses,21 and the overall seriously mentally ill population,22 the average age of consumers in the study was midforties. This Michigan sample of consumers with serious mental illness, however, did appear to differ from others described in the psychiatric rehabilitation literature in terms of having fewer individuals with less than high school/GED education levels (approximately 25% for this sample compared to approximately 41%),22 and more individuals with some college preparation. It is possible that this is a reflection of Michigan’s ongoing economic difficulties and the significant and continuing loss of jobs in the state. That is, individuals with a high school education or some college, who were previously employed, may find themselves without an income or health coverage and turn to the public system for mental health care.
Contrary to prediction, there was a significantly higher percentage of males in CRDI centers than in clubhouses in this study. In fact, most participants in this study were male, as is the case with other studies of consumer-centered programs.3,4,21,23 This is in contrast to samples of people with serious mental illnesses in which females predominate.22 It appears that women are less likely to be enrolled in vocational programs 24,25 and more likely to get services from mental health outpatient or crisis/emergency programs.26 Women clients usually have lower rehabilitation needs than men,27 and they or their providers may be less interested in vocational programs. The reason for the greater proportion of males at the drop-in centers is open to speculation; perhaps the less structured nature of the setting makes women uncomfortable or the location of drop-in centers may make them less accessible to women because of transportation or safety issues. These findings are consistent with other differences found between CRDIs and clubhouses. That is, consumers in clubhouses reported coming to the center for a longer period of time and attending more frequently than consumers in drop-ins, suggesting a more stable, structured atmosphere. In addition, according to participants, clubhouses in the sample tended to be in safer locations.
The second hypothesis was that consumers in clubhouses are more likely to have a diagnosis of schizophrenia than those in CRDIs. This hypothesis was confirmed, even after controlling for consumer age, sex, race, and education—variables that are sometimes confounded with a schizophrenia diagnosis. In clubhouses, more than a third of those interviewed reported a schizophrenia diagnosis, in contrast to only about one-fifth in the drop-in centers. This is consistent with the research on clubhouses; in fact, in some studies, the majority of clubhouse members had schizophrenia and/or other psychotic disorder diagnoses.7,10–13,21
The final hypothesis, that consumers in CRDIs have less interaction with traditional mental health and support services, was also confirmed. Congruent with the above, members of CRDI centers were found to have fewer lifetime hospitalizations. Similarly, consumers in clubhouses were nearly twice as likely to admit having a mental illness, more than three times as likely to be on SSI/SSDI, and received significantly higher levels of case management services. We also found that CRDI users were significantly more likely to report a substance abuse history.
We also explored whether consumers in either program have more of a recovery-oriented focus because of the different program emphases within each setting. In fact, clubhouse members were more likely to endorse a belief that they were in recovery from mental illness, even after controlling for the fact that clubhouse members were more likely to report having a mental illness. There were no differences on the State Hope Scale, suggesting that consumers from both programs were equally hopeful and optimistic about their outcomes. However, the clubhouse-based consumers did report a significantly higher quality of life than those in CRDIs.
Implications for Behavioral Health
The results indicate that there are some statistically significant and meaningful differences between users of CRDI centers and clubhouses. Overall, the pattern of results suggests that those consumers who utilize clubhouses are more likely to be disabled—at least, based on their psychiatric history (i.e., SSI/SSDI receipt, past psychiatric hospitalizations, schizophrenia diagnoses) and more immersed in the public mental health system—receiving more case management services monthly, more apt to indicate that they do have a mental illness, and more likely to reside in supervised living arrangements. In contrast, consumers in drop-in centers were more likely to be male and to report substance abuse histories—a fact which would make them more likely to be excluded from traditional mental health programs.2,28 They were also less satisfied with their global quality of life—perhaps because of having a more difficult past or current life circumstances.
There are a number of possible reasons for these differences. As indicated in the introduction, individuals who go to clubhouses may have a higher need for structure; the reported differences appear to reflect this. Or, perhaps, consumers who have less disability feel constrained by the more routinized clubhouse environment and/or are less compliant, and therefore, more likely to visit consumer-run programs. It could also be that the population differences in service use are based on referral patterns; for example, those individuals who are more immersed in the mental health system are more likely to be referred to clubhouses and prioritized for admission. In comparison, individuals without regular case management contacts may be less likely to be referred and less likely to hear about such programs and refer themselves, and/or self-referrals may be less likely to result in admissions. In a cost-conscious CMH system, referral patterns would be likely to differ for those with significantly greater psychiatric hospital utilization, as keeping people out of inpatient care is an extremely effective cost-saving method. The results clearly indicate the utility of funding CRDIs as an alternative to more traditional mental health services as they seem to serve individuals who might not otherwise receive mental health services.
Further research is needed to determine the extent to which the differences found in this study are replicated in other states and, if so, to understand the underlying causes. It is interesting to note that despite the fact that there were no differences in symptom levels for consumers in CRDIs versus clubhouses, consumers in clubhouses were receiving more frequent case management services. Whether this is because of the choices of consumers using CRDIs, to exclusionary practices of the more traditional programs in the public mental health system (i.e., clubhouses), or because receipt of services reduces symptomatology cannot be discerned through this cross-sectional data.
Certain limitations of the present study should be acknowledged. First, although data was collected from a large number of CRDIs and clubhouses, they were all located within the same Midwest state. CRDIs, in particular, show wide variation in their operations and effectiveness, even their very existence, state by state. Clubhouses, however, have a national organization (the ICCD) which sets standards and certifies clubhouse programs according to how well they meet the standards. Thus, these results on the characteristics of users of CRDI centers may not be replicated in other locations. In particular, several aspects of the Michigan mental health system should be kept in mind. The state of Michigan has a history of supporting consumer-centered initiatives and encouraging mental health professionals to incorporate consumer groups into the continuum of treatment options.31 More recently, a governor-appointed Mental Health Commission initiated a series of public hearings and meetings to develop a plan for overhauling the Michigan mental health system. The Commission’s final report highlights recovery-oriented and consumer-centered vision for the system. This must, however, be placed within the context of Michigan’s current economic difficulties. The loss of automotive and other manufacturing jobs has left many people without an income or health coverage and has hindered the state’s ability to adequately fund many mental health services.
Second, the limitations of self-report data need to be acknowledged. Although the measures were completed by nearly 2,000 consumers, they still reflect only the perceptions of the consumers themselves and, therefore, may be subject to more error than multisource, multimethod data. Future studies should attempt to obtain data from records, observations, and reports of knowledgeable others. In addition, whereas the multi-item measures (symptomatology and the State Hope Scale) had good reliabilities, many of the other measures were single-item, reflecting the fact that the consumer interviews were one piece of a larger data collection effort intended to develop CRDI fidelity criteria. Finally, the cross-sectional nature of the data does not allow us to consider how the characteristics of consumers in CRDIs and clubhouses may fluctuate over time. This is important given the dynamic nature of the recovery process and the ways in which consumers move in and out of services over time.
Conclusion
This study provides service providers with important information about the characteristics of consumers who use these two widely implemented models of consumer-centered services. The results suggest that users of CRDIs are less willing or unable to use more structured mental health services, indicating a need for the provision of both models. We recommend that much more research is needed on service use by individuals with psychiatric disabilities, particularly related to consumer-centered services, so that some definite conclusions can be established about consistencies and variations in patterns of service use across subgroups and across geographic locations. We should then be able to look at ways to optimize the match between consumer needs and program availability, accessibility, and acceptability. In this continuing era of extremely constrained resources for mental health and support services, the most efficient and effective allocation of limited resources must be taken as a mandate.
Notes
Like CRDIs, self-help agencies are completely consumer-run. These studies are included in the review of the literature because of the small number that focused specifically on CRDIs.
References
Mowbray CT, Moxley DP, Jasper CA, et al. (Eds.). Consumers as Providers in Psychiatric Rehabilitation. Columbia, MD: International Association of Psychiatric Rehabilitation Services; 1997.
U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services; 1999.
Chamberlin J, Rogers ES, Ellison ML. Self-help programs: a description of their characteristics and their members. Psychiatric Rehabilitation Journal. 1996;19(3):33–42.
Hodges JQ, Segal SP. Goal advancement among mental health self-help agency members. Psychiatric Rehabilitation Journal. 2002;26(1):78–85.
Segal SP, Silverman C. Determinants of client outcomes in self-help agencies. Psychiatric Services. 2002;53(3):304–309.
Segal SP, Hardiman ER, Hodges JQ. Characteristics of new clients at self-help and community mental health agencies in geographic proximity. Psychiatric Services. 2002;53(9):1145–1152.
Yanos PT, Primavera LH, Knight EL. Consumer-run service participation, recovery of social functioning, and the mediating role of psychological factors. Psychiatric Services. 2001;52(4):493–500.
Accordino MP, Herbert JT. Treatment outcome of four rehabilitation interventions for persons with serious mental illness. Journal of Mental Health Counseling. 2000;22(3):268–282.
Oliver J, Huxley P, Bridges K, et al. Quality of Life and Mental Health Services. London: Routledge; 1996.
Warner R, Huxley P, Berg T. An evaluation of the impact of clubhouse membership on quality of life and treatment utilization. The International Journal of Social Psychiatry. 1999;45(4):310–320.
Macias C, Barreira P, Alden M, et al. The ICCD Benchmarks for clubhouses: a practical approach to quality improvement in psychiatric rehabilitation. Psychiatric Services. 2001;52(2):207–213.
Rosenfield S, Neese-Todd S. Elements of a psychosocial clubhouse program associated with a satisfying quality of life. Hospital and Community Psychiatry. 1993;44:76–78.
Stein LI, Barry KL, Dien GV, et al. Work and social support: a comparison of consumers who have achieved stability in ACT and clubhouse programs. Community Mental Health Journal. 1999;35(2):193–204.
Mowbray CT, Holter MC, Stark L, Pfeffer C, Bybee D. A fidelity rating instrument for consumer-run drop-in centers (FRI-CRDI). Research on Social Work Practice. 2005;15(4):278–290.
Shern D, Lee B, Coen A. The Colorado Symptom Index: A Self-Report Measure for Psychiatric Symptoms. Tampa, FL: Louis de la Parte Mental Health Institute; 1996.
Lehman AF. A quality of life interview for the chronically mentally ill. Evaluation And Program Planning. 1998;11:51–62.
Snyder CR, Sympson SC, Ybasco FC, et al. Development and validation of the state hope scale. Journal of Personality and Social Psychology. 1996;2:321–335.
Nelson G, Hall GB, Walsh-Bowers R. The relationship between housing characteristics, emotional well-being, and the personal empowerment of psychiatric consumer/survivors. Community Mental Health Journal. 1998;34(1):57–69.
Raudenbush SW, Bryk AS. Hierarchical Linear Models in Social and Behavioral Research: Applications and Data-Analysis Methods (2nd ed.). Newbury Park, CA: Sage; 2002.
Raudenbush S, Bryk A, Cheong YF, et al. HLM 6: Hierarchical Linear and Nonlinear Modeling. Chicago, IL: Scientific Software International; 2004.
Macias C, Jackson R, Schroeder C, et al. What is a clubhouse? Report on the ICCD 1996 survey of USA clubhouses. Community Mental Health Journal. 1999;35(2):181–190.
Roth D, Crane-Ross D. Impact of services, met needs, and service empowerment on consumer outcomes. Mental Health Services Research. 2002;4(1):43–56.
Mastboom J. Forty clubhouses: model and practices. Psychosocial Rehabilitation Journal. 1992;16(2):9–23.
Menz FE, Hansen G, Smith H, et al. Gender equity in access, services, and benefits from vocational rehabilitation. Journal of Rehabilitation, 1989;(January/February/March)55(1):31–40.
Mowbray CT, Oyserman D, Lutz C, et al. Women: the ignored majority. In: Spaniol L, Gangue C, Koehler M, eds. Psychological and Social Aspects of Psychiatric Disability. Boston: Center for Psychiatric Rehabilitation; 1997:171–194.
Swartz MS, Wagner HR, Swanson JW. Comparing use of public and private mental health services: the enduring barriers of race and age. Community Mental Health Journal. 1998;34(2):133–144.
Seeman MV. Women and schizophrenia. Medscape Women’s Health. 2000;5(2):2.
Watkins KE, Hunter SB, Wenzel SL, et al. Prevalence and characteristics of clients with co-occurring disorders in outpatient substances abuse treatment. The American Journal of Drug and Alcohol Abuse. 2004;30(4):749–764.
Frese FJ, Stanley J, Kress K, et al. Integrating evidence-based practices and the recovery model. Psychiatric Services. 2001;52:1145–1152.
Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal. 1993;16(4):11–23.
Mowbray CT, Chamberlain P, Jennings M, et al. Consumer-run mental health services: results from five demonstration projects. Community Mental Health Journal. 1988;24(2):151–156.
Acknowledgement
This study was funded, in part, by a grant from the National Institute of Mental Health to the first author (#R24-MH51363, to the University of Michigan School of Social Work, Center for Poverty, Risk and Mental Health).
Author information
Authors and Affiliations
Corresponding author
Additional information
Carol T. Mowbray is deceased.
Rights and permissions
About this article
Cite this article
Mowbray, C.T., Woodward, A.T., Holter, M.C. et al. Characteristics of Users of Consumer-Run Drop-In Centers Versus Clubhouses. J Behav Health Serv Res 36, 361–371 (2009). https://doi.org/10.1007/s11414-008-9112-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-008-9112-8