Abstract
We aimed to verify whether different levels of training performed regularly and voluntarily for many years could have an impact on one of the main issues of immunosenescence: the poor response to vaccines. We recruited 61 healthy elderly men (65–85 years old), 23 with a moderate training (MT) lifestyle (for 17.0 ± 3.2 years), 22 with an intense training (IT) lifestyle (for 25.9 ± 3.4 years), and 16 without a training lifestyle (NT). Fitness was evaluated through the IPAQ and VO2max consumption. The participants were evaluated regarding cognitive aspects, nutritional status, depression, and quality of life. Antibody titers were determined by hemagglutination inhibition assay prior to influenza vaccination and at 6 weeks and 6 months post-vaccination. Strains used were B, H3N2, and H1N1. Our groups were matched for most characteristics, except for those directly influenced by their lifestyles, such as BMI, VO2max, and MET. In general, MT and IT elderly men showed significantly higher antibody titers to the three vaccine strains post-vaccination than NT elderly men. There were also higher titers against B and H1N1 strains in the trained groups before vaccination. Additionally, there were higher proportions of seroprotected (titers ≥1:40) individuals in the pooled trained groups both at 6 weeks (B and H3N2, p < 0.05) and 6 months (H1N1, p < 0.05; B, p = 0.07). There were no significant differences between the MT and IT groups. Either a moderate or an intense training is associated with stronger and longstanding antibody responses to the influenza vaccine, resulting in higher percentages of seroprotected individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunosenescence refers to changes that affect the competence of the immune system with advancing age. Its etiology is multifactorial and reflects exposure to external pathogens, persistent viral infections, obesity, physical and psychological stress, and thymic involution among other events over an individual’s life (de Araújo et al. 2013). Immunosenescence is a major cause of increased morbidity and early mortality (Larbi et al. 2008) and is characterized by changes in T cell subpopulations, reduced numbers of B cells, deficiencies in antibody isotype switching, and reduced ability to produce specific antibodies (Alam et al. 2013; Agarwal and Busse 2010), all of which compromise immunization responsiveness (Weiskopf et al. 2009). Because of this compromise, influenza remains a significant cause of mortality among the elderly. Recently, regular physical activity has been proposed as a low-cost and potentially effective strategy to retard or prevent immunosenescence (Senchina and Kohut 2007).
Several studies have suggested that regular exercise has a positive impact on the antibody response to the influenza vaccine in older adults (Grant et al. 2008; Keylock et al. 2007; Kohut et al. 2002, 2004; Schuler et al. 2003; Woods et al. 2009; Yang et al. 2007). However, the regular exercise protocols varied among the studies, from aerobic cardiovascular exercises to Tai-chi practices, thus making it difficult to establish which protocols were optimal (Pascoe et al. 2014). It was concluded from these studies that the necessary volume and relative advantages of endurance and/or resistance training have not been adequately investigated. Moreover, most studies were supervised, 4 to 10 months interventional studies (Grant et al. 2008; Kohut et al. 2004; Woods et al. 2009; Yang et al. 2007). Only three studies enrolled “spontaneously” high- and low-fitness participants. The criteria used to define and measure fitness were also variable and included a self-reported assessment of physical activity recorded through phone interview (Kohut et al. 2002; Schuler et al. 2003) or VO2max consumption testing (Keylock et al. 2007).
We thus aimed to verify whether different levels of exercise performed regularly and voluntarily for many years could have an impact on one of the main issues of immunosenescence: the poor response to vaccines.
Methods
Participants
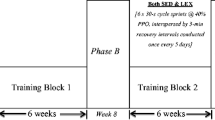
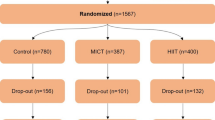
This was a cross-sectional study involving 61 healthy elderly men (65–85 years). They were recruited mainly at runners’ associations, sports clubs, community-based exercise programs for elderly, outpatient services, and the association of ex-functionaries of our institution. Exclusion criteria were the presence of co-morbidities that could interfere with the immune system (e.g., AIDS, cancer, rheumatoid arthritis, and uncontrolled diabetes mellitus), use of immunosuppressive drugs (e.g., corticosteroids), smoking habits, alcohol abuse, and lack of influenza vaccination in previous years. Participants underwent clinical evaluation by a physician (MTSM or LEGL) and answered the following questionnaires: global depression score (Yesavage et al. 1982), Mini Nutritional Assessment (Vellas et al. 1999), mini-mental state examination [MMSE] (Brucki et al. 2003), and quality of life SF-36 (Ciconelli et al. 1999). There were 16 participants who had never trained (NT), 23 who moderately trained (MT), i.e., who practiced two or three times/week volleyball, basketball, or running (less than 6 km/training), and 22 who intensely trained (IT), who trained ≥5 days/week (>50 km/week). The trained elderly were recruited among those who underwent regular training over at least the last 5 years. The study was approved by the Hospital das Clínicas Review Board (#0135/11), and all participants signed an informed consent form. Blood sampling in the trained groups was conducted ≥48 h after the last training session and at least 1 week after participation in any competition. Fitness status was assessed through the International Physical Activity Questionnaire (IPAQ) and a treadmill VO2 max consumption. The latter was done as previously described with modifications (Santos-Silva et al. 2007). Briefly, during the cardiopulmonary exercise testing, the individuals were monitored with a computerized electrocardiograph (HeartWare Instruments, Ergo 13, Belo Horizonte, Brazil), and heart rate was measured on the ECG recording (leads DI, DII, DIII, AVf, AVl, AVr, V1, V2, V3, V4, V5, V6) in rest, during exercise and recuperation phase at the end of each minute. The oxygen consumption (V̇O 2), carbon dioxide output (VCO2), and minute ventilation (V̇e) were measured and analyzed by using a metabolic analyzer (CPX/D, MedGraphics, USA) (Milani et al. 2004). The exercise testing was performed in treadmill (hp/Pulsar, Cosmos, Germany). A modified version of the Heck stress test protocol was used (Heck et al. 1985).
Influenza vaccination procedure and hemagglutination inhibition assay (HIA)
The influenza vaccine is provided freely to individuals over 60 every year by mid April, before the winter season in Brazil. In the years of 2012 and 2013, the vaccine was from Sanofi Pasteur (Vaxigrip, Sanofi Pasteur SA, Val-de-Reuil, France). It is administered intramuscularly at a single dose. The participants were asked to refrain from training in the 48 h previous to the vaccination. The influenza virus antigens used in the vaccine and for the HIA were A/California/7/2009 (H1N1)pdm09-like virus, A/Perth/16/2009 (H3N2)-like virus, and B/Brisbane/60/2008-like virus (lineage Victoria) for those vaccinated in 2012 and A/California/7/2009 (H1N1)pdm09-like virus, A/Victoria/361/2011 (H3N2)-like virus, B/Wisconsin/1/2010-like virus (lineage Yamagata) for those vaccinated in 2013. The HIA was performed according to WHO recommendations (Kendal et al. 1982). Viral concentrations were determined by hemagglutinin antigen titration, and the test was performed after removing naturally occurring, non-specific inhibitors from the sera, as described previously (Kendal et al. 1982). Titration of antigen, serum treatment, and the preparation of chicken erythrocytes were carried out as recommended by the WHO (Webster et al. 2002).
Statistical analysis
Statistical analysis was performed using SPSS-20.0 (IBM Corporation). A Kruskal-Wallis analysis with Dunn’s post-test was used to compare non-parametric data from the three groups, and ANOVA with Newman-Keuls post-test was used for parametric data. The reciprocal HIA titers were log transformed (log2) due to skewed distribution. Repeated-measures ANOVA was used to compare the antibody response within each group. The chi-square test was used to compare proportions of seroprotected subjects among the groups. Significance was set at p < 0.05.
Results
Participant characteristics
A summary of participant characteristics is shown in Table 1. All groups comprised independently living elderly men with positive self-perceived health, who performed their routine daily activities without difficulties. Fitness status, as assessed through both the IPAQ and VO2max, clearly distinguished the groups, in agreement with their reported lifestyles. Although the IT group was slightly older than the MT and NT groups, their mean ages were not significantly different. As expected, the IT group had the lowest BMI and highest metabolic equivalent score (METs). The MT group had a BMI comparable to that of the NT group but significantly higher METs. The average length of regular training reported by both the MT and IT groups was high and significantly different, 17.0 years and 25.9 years, respectively. All elderly participants reported yearly influenza vaccination in at least the previous 5 years; however, the total number of previous vaccinations could not be reliably confirmed.
The elderly groups did not differ in most of their psychosocial characteristics according to the MNA, GDS-15, and SF36 questionnaires. They presented with adequate nutritional status, and mild suspected depression was detected in only one subject within each group. Assessment of quality of life by the SF-36 showed that all three groups scored good, very good, or excellent in most parameters, except for the physical functioning score, which, as expected, showed a better performance in the MT and IT groups, even though the NT group mean score was still very good. Evaluation of mental status through the MMSE questionnaire showed mean values indicative of an intact status in all three groups, although the MT group’s score was significantly higher than that of the NT group.
Antibody responses to trivalent influenza vaccination
NT elderly showed low titers of anti-influenza strain B antibodies before vaccination (Fig. 1a). Neither at 6 weeks nor at 6 months post-vaccination was there an increase in these titers. In contrast, both the MT and IT groups showed a significant increase in the antibody titers at 6 weeks (p < 0.001, Fig. 1a). Interestingly, while the antibody titers remained elevated at 6 months in the MT group, in the IT group, they significantly decreased (p < 0.001). Thus, by 6 months, the titers in the MT group, but not in the IT group, were significantly higher than the pre-vaccination titers (p < 0.05). When we compared the three elderly groups, the trained groups reached higher titers than the NT group. At week 6, both the MT and IT groups had significantly higher titers than the NT group (p < 0.05), while at 6 months, the difference was significant only for the MT group (p < 0.5). Interestingly, higher titers were also observed pre-vaccination, although the difference was significant only for the IT group (p < 0.05).
Reciprocal anti-influenza B (a), H3N2 (b), and H1N1 (c) antibody dilution in untrained (white triangle) (n = 16), moderately trained (white circle) (n = 23), and intensely trained (white square) (n = 22) elderly, as determined by the hemagglutination inhibition assay, pre-vaccination and 6 weeks and 6 months post-vaccination. Asterisks indicate significant differences (p < 0.05) between the untrained elderly and the moderately and/or intensely trained elderly at the same time point. Plus sign indicates a significant difference between two time-points in the same group; the plus sign on the right indicates a significant difference between 6 months and pre-vaccination
NT elderly responses to the H3N2 strain followed a pattern similar to those with the B strain (Fig. 1b). There was a slight but significant rise (p < 0.05) in the titers at week 6, which dropped by 6 months (p < 0.05) to lower levels, similar to those at pre-vaccination. The trained groups displayed a much sharper rise in titers from pre-vaccination to week 6 (p < 0.001 for both). By 6 months, the titers in the MT group had dropped to pre-vaccination levels, while in the IT group, the drop was less steep and the antibody titers remained significantly higher than at pre-vaccination (p < 0.05). As for the B strain, comparison of the three groups showed significantly higher titers in the trained groups at both post-vaccination time points and a trend for higher titers even before vaccination.
Data for the three groups with the H1N1 strain also showed similar patterns to the previous two strains (Fig. 1c). Antibody titers rose significantly after vaccination (6 weeks) in the 3 groups (NT and MT, p < 0.001; IT, p < 0.05), which was followed by a slight but significant drop by 6 months (NT, p < 0.01; MT and IT, p < 0.05). Antibody titers were higher pre- and post-vaccination in the IT group, compared with the NT group (p < 0.05). The MT group also exhibited higher titers than the NT group, although this increase was significant only at pre-vaccination and 6 months post-vaccination (p < 0.05 and p < 0.01, respectively).
Of note, there were no significant differences between the MT and IT groups at any time point for all three strains. Thus, both moderate and intense exercise apparently improved, to a similar degree, the influenza vaccination antibody response. To extend further this finding, we analyzed the number of individuals in each group who achieved protective antibody titers (≥1:40) (Goodeve et al. 1983). Table 2 shows that both the MT and IT groups had higher percentages of seroprotected individuals at 6 weeks and 6 months post-vaccination. Thus, while by week 6 only 33 % of the NT elderly achieved seroprotection for the B strain, over 60 % of the elderly in the trained groups achieved this protection. The percentages of NT seroprotected individuals were higher with the H1N1 (60 %) and H3N2 (66 %) strains, but even higher in the trained groups, especially with the H3N2 strain (83 % in the MT group and 91 % in the IT group). Remarkably, while the percentages of seroprotection decreased slightly or modestly by 6 months, they were still higher in the trained groups, in which 62 to 81 % of the elderly persisted with protective titers against the H1N1 and H3N2 strains; again the B strain elicited weaker responses. However, due to the relatively small sample size, the differences among the groups were not statistically significant (Table 2). Thus, to increase the power of the statistical analysis, we pooled the two trained groups and compared this pooled group (MT/TI) with the NT group. The MT/TI group showed significantly higher percentages of seroprotected individuals at 6 weeks for the B (p = 0.035) and H2N3 (p = 0.025) strains and, remarkably, at 6 months with the H1N1 strain (p = 0.032) while with the B strain, the difference approached significance (p = 0.071). Thus, these data corroborate the finding of enhanced antibody response to influenza vaccination promoted by an exercise lifestyle.
Discussion
Although it has been postulated that regular exercise positively impacts antibody responses to vaccination in the elderly, the reported effects were heterogeneous in both intensity and duration, reflecting their methodological variability. Schuler et al. showed a positive effect at week 1, but not at weeks 2, 4, and 6 post-vaccination, and this effect was observed for only one of the components of the vaccine (Schuler et al. 2003). Yang et al. observed a positive effect only when data from the three vaccine components were pooled, probably as a consequence of their small sample size (Yang et al. 2007). On the other hand, more consistent findings were reported by Woods’ group, who showed that the high-fitness group responded with a higher antibody response to 2 of the 3 vaccine components, 6 and 24 weeks post-vaccination (Keylock et al. 2007). It should be noted, however, that the high-fitness elderly in that study were compared with very low-fitness elderly, selected mostly in the lower 10th percentile of the VO2max data for age and being somewhat older than the high-fitness elderly (67.9 ± 1.2 vs. 64.8 ± 1.2 years old). Two additional reports examined the effect on the primary antibody response to immunization with a novel antigen, KLH (Grant et al. 2008; Smith et al. 2004). One study was interventional (10-month cardiovascular exercise), and the other included endurance-trained elderly. Both studies showed enhancement of IgM and IgG1 but not IgG2 responses, compared with a flexibility exercise intervention group and sedentary elderly group, respectively. Interestingly, in the latter study, there was no correlation between the antibody response enhancement and the fitness improvement evaluated by METs and VO2max. In our study, we also could not find such correlation (data not shown).
Although controlled interventional studies have some advantages compared with cross-sectional studies, they also have the disadvantage that they represent unnatural, well-controlled scenarios (Rohrbach et al. 2006). Thus, aiming to be closer to the natural scenario, we focused our cross-sectional study on healthy elderly who spontaneously and regularly trained either vigorously (for an average of 26 ± 3 years) or moderately (17 ± 3 years), and compared them with healthy non-trained elderly. All participants had independent lives and managed their everyday activities without difficulty. Our results showed that sustained regular exercise, performed either at a moderate or a high intensity, enhanced the antibody responses to all three components of the influenza vaccine, resulting in higher percentages of seroprotected individuals at both 6 weeks and 6 months post-vaccination. Only one previous study has evaluated two elderly groups on different exercise intensities (Kohut et al. 2002) and found that the highly active elderly, but not the moderately active elderly, had higher antibody responses to influenza vaccine than the sedentary elderly. Several methodological differences between this study and our study may account for the different results. In the above-referenced study, the level of physical activity was self-reported by a phone interview and referred only to the previous year, and there was no information regarding the number of years the participants had been practicing vigorous or less vigorous (moderate) exercise. Additionally, IgM and IgG ELISA assays that measured total anti-influenza antibody reactivity at only one time point, 2 weeks post-immunization, were used. An interesting finding of our study is that the enhancement effect of exercise was not only observed at the peak response (6 weeks) but also persisted for at least 6 months post-vaccination. This effect seemed to persist for up to a year, as suggested by the trend for higher antibody levels already at pre-vaccination in the trained groups. In fact, the pre-vaccination levels correspond to the subsiding antibody titers produced by the previous year’s vaccination, and in both trained groups, the decay tended to be less steep.
Our three elderly groups clearly differed in their fitness status, whether measured through METs or VO2max, confirming their lifestyle history. It has been shown that psychosocial characteristics can also modulate elderly immune responses to influenza vaccine, although mainly the cell-mediated responses, and not the antibody responses, were affected (Kohut et al. 2005). We thus employed several questionnaires to assess in our groups the psychosocial characteristics that might affect their immunoresponsiveness. Overall, our groups were matched for most characteristics except for those directly influenced by their lifestyles, such as lower BMI in the IT group and lower physical functioning (SF-36) in the NT. Although there were no significant differences in the groups’ ages, the IT group was slightly older. However, this difference could potentially have impaired and not favored their higher antibody responses.
This study has limitations. We did not survey the prevalence of flu-like episodes in our elderly. However, the influence of the vaccine on the prevalence of flu-like episodes may be difficult to estimate because of the heterogeneous etiology of these episodes in our setting, with only a small percentage related to influenza virus, even in non-vaccinated populations, <5 % outside the peak season and <25 % at the peak season (Sistema de Vigilância Epidemiológica da Gripe 2012, Brazil). We also did not assess cell-mediated immune responses to the vaccine, which are also affected by aging (McElhaney et al. 2006). Some of the subjects enrolled in this study participated in a parallel study of the effects of aging on T cells, and in fact, there were several aspects of the biology of these cells that were improved in the trained groups [Silva and de Araújo, manuscript in preparation]; however, the cell-mediated responses to influenza antigens were not examined. Another issue is the size sample. This study allowed us to detect differences among groups, although in a number of instances, there were differences that were close but not significant. A larger sample size could possibly identify more subtle differences among the groups.
In conclusion, we show that either a moderate or an intense training lifestyle leads to stronger and longstanding antibody responses to the influenza vaccine components, resulting in higher percentages of seroprotected individuals.
References
Agarwal S, Busse PJ (2010) Innate and adaptive immunosenescence. Ann Allergy Asthma Immunol 104(3):183–190. doi:10.1016/j.anai.2009.11.009, quiz 190–2, 210
Alam I, Goldeck D, Larbi A et al (2013) Aging affects the proportions of T and B cells in a group of elderly men in a developing country—a pilot study from Pakistan. Age (Dordr) 35:1521–1530. doi:10.1007/s11357-012-9455-1
Brucki SM, Nitrini R, Caramelli P et al (2003) Okamoto. Suggestions for utilization of the mini-mental state examination in Brazil. Arq Neuropsiquiatr 61:777–781
Ciconelli RM, Ferraz MB, Santos W et al (1999) Brazilian-Portuguese version of the SF-36. A reliable and valid quality of life outcome measure. Rev Bras Reumatol 39:147–150
de Araújo AL, Silva LCR, Fernandes JR et al (2013) Preventing or reversing immunosenescence: can exercise be an immunotherapy? Immunotherapy 5:879–893. doi:10.2217/imt.13.77
Goodeve A, Potter CW, Clark A et al (1983) A graded dose study of inactivated surface antigen influenza B vaccine in volunteers. J Hyg Camb 90:107–115
Grant RW, Mariani RA, Vieira VJ et al (2008) Cardiovascular exercise intervention improves the primary antibody response to keyhole limpet hemocyanin (KLH) in previously sedentary older adults. Brain Behav Immun 22:923–932. doi:10.1016/j.bbi.2008.01.006
Heck H, Mader A, Hess G, Mucke S, Muller R, Hollmann W (1985) Justification of the 4 mmol/L lactate threshold. Int J Sports Med 6:117–130
Kendal AP, Pereira MS, Skehel JJ (eds) (1982) Concepts and procedures from laboratory-based influenza surveillance. Centers for Disease Control and Prevention, Atlanta
Keylock KT, Lowder T, Leifheit KA et al (2007) Higher antibody, but not cell-mediated, responses to vaccination in high physically fit elderly. J Appl Physiol 102:1090–1098
Kohut ML, Cooper MM, Nickolaus MS et al (2002) Exercise and psychosocial factors modulate immunity to influenza vaccine in elderly individuals. J Gerontol A Biol Sci Med Sci 57:M557–M562
Kohut ML, Arntson BA, Lee W et al (2004) Moderate exercise improves antibody response to influenza immunization in older adults. Vaccine 22:2298–2306
Kohut ML, Lee W, Martin A, Arnston B et al (2005) The exercise-induced enhancement of influenza immunity is mediated in part by improvements in psychosocial factors in older adults. Brain Behav Immun 19:357–366
Larbi A, Franceschi C, Mazzatti D et al (2008) Aging of the immune system as a prognostic factor for human longevity. Physiology 23:64–74. doi:10.1152/physiol.00040.2007
McElhaney JE, Xie D, Hager WD et al (2006) T cell responses are better correlates of vaccine protection in the elderly. J Immunol 176:6333–6339
Milani RV, Lavie CJ, Mehra MR (2004) Cardiopulmonary exercise testing. How do we differentiate the cause of dyspnea? Circulation 110:e27–e31
Pascoe AR, Fiatarone Singh MA, Edwards KM (2014) The effects of exercise on vaccination responses: a review of chronic and acute exercise interventions in humans. Brain Behav Immun 39:33–41. doi:10.1016/j.bbi.2013.10.003
Rohrbach LA, Grana R, Sussman S, Valente TW (2006) Type II translation: transporting prevention interventions from research to real-world settings. Eval Health Prof 29(3):302–333
Santos-Silva PR, Fonseca AJ, Castro AW, Greve JMD, Hernandez AJ (2007) Reproducibility of maximum aerobic power (VO2max) among soccer players using a modified Heck protocol. Clinics 62:391–396
Schuler PB, Leblanc PA, Marzilli TS (2003) Effect of physical activity on the production of specific antibody in response to the 1998–99 influenza virus vaccine in older adults. J Sports Med Phys Fitness 43:404
Senchina DS, Kohut ML (2007) Immunological outcomes of exercise in older adults. Clin Interv Aging 2:3–16
Sistema de vigilância epidemiológica da gripe SIVEP-GRIPE. Vigilância Sentinela Circulação Viral (2012). http://portalsaude.saude.gov.br/index.php/situacao-epidemiologica-dados-influenza. Accessed 21 May 2015
Smith TP, Kennedy SL, Fleshner M (2004) Influence of age and physical activity on the primary in vivo antibody and T cell-mediated responses in men. J Appl Physiol 97:491–498
Vellas B, Guigoz Y, Garry PJ, Nourhashemi F et al (1999) The Mini Nutritional Assessment (MNA) and its use in grading the nutritional state of elderly patients. Nutrition 15:116–122
Webster R, Cox N, Stohr K (2002) World Health Organization manual on animal influenza diagnosis and surveillance. WHO, Geneva, pp 37–40
Weiskopf D, Weinberger B, Grubeck-Loebenstein B (2009) The aging of the immune system. Transpl Int 22:1041–1050. doi:10.1111/j.1432-2277.2009.00927.x
Woods JA, Keylock KT, Lowder T et al (2009) Cardiovascular exercise training extends influenza vaccine seroprotection in sedentary older adults: the immune function intervention trial. J Am Geriatr Soc 57:2183–2191. doi:10.1111/j.1532-5415.2009.02563.x
Yang Y, Verkuilen J, Rosengren KS et al (2007) Effects of a Taiji and Qigong intervention on the antibody response to influenza vaccine in older adults. Am J Chin Med 35:597–607
Yesavage JA, Brink TL, Rose TL et al (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Acknowledgments
This work was supported by Fundação de Amparo à Pesquisa do Estado de São Paulo (#2011/08817-0 [GB] and #2011/18268-4 [LCRS]), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (#14952/13-0 [ALA]), and Conselho Nacional de Desenvolvimento Científico e Tecnológico (LEGL and GB). We thank Terezinha M. Paiva of the Respiratory Diseases Center, Adolf Lutz Institute, São Paulo, for providing the influenza antigens, Magali Ruivo from the Cotia’s county program “Saber Viver” for helping with recruitment of the participants, Paulo RS Silva for the ergospirometry testing, and Isac de Castro for statistics advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Author contributions
Adriana L de Araújo, Léia CR Silva, and Juliana R Fernandes contributed to the recruitment of the participants, questionnaires application, blood sampling and processing of the data; Manuella ST Matias and Luiz E Garcez-Leme contributed with the recruitment and clinical evaluation of the participants; Lucy S Boas and Clarisse M Machado standardized and carried out the HIA; Gil Benard and Luiz E Garcez-Leme designed and coordinated the study; Gil Benard, Luiz E Garcez-Leme, Adriana L de Araújo, and Léia CR Silva wrote the paper.
Additional information
Adriana Ladeira de Araújo and Léia Cristina Rodrigues Silva contributed equally to this work.
About this article
Cite this article
de Araújo, A.L., Silva, L.C.R., Fernandes, J.R. et al. Elderly men with moderate and intense training lifestyle present sustained higher antibody responses to influenza vaccine. AGE 37, 105 (2015). https://doi.org/10.1007/s11357-015-9843-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-015-9843-4