Abstract
Walking speed is shown to be an important indicator of the health status and function in older adults and part of the comprehensive geriatric assessment in clinical practice. The present study aimed to assess the influence of different assessment methods on walking speed and its association with the key aspects of poor health status, i.e., the presence of low cognitive performance and cardiopulmonary disease. In 288 community-dwelling elderly (mean age 82.2 ± 7.1 years) referred to a geriatric outpatient clinic, walking speed was assessed with the 4-m, 10-m, and 6-min walking tests. The mean walking speed assessed with the 10-m walking test was higher compared to the 4-m and 6-min walking tests (mean difference (95 % CI) 0.11 m/s (0.10; 0.13) and 0.08 m/s (0.04; 0.13), respectively). No significant difference was found in the walking speed assessed with the 4-m compared to the 6-min walking test (mean difference (95 % CI) −0.03 m/s (−0.08; 0.03)). ICCs showed excellent agreement of the 4-m with the 10-m walking test and fair to good agreement of the 6-min with the 4-m as well as 10-m walking test. The presence of low cognitive performance was negatively associated with walking speed, with the highest effect size for the 4-m walking test. The presence of cardiopulmonary disease was negatively associated with walking speed as well, with the highest effect size for the 6-min walking test. In conclusion, in the clinically relevant population of elderly outpatients, walking speed and its interpretation depends on the assessment method, which therefore cannot be used interchangeably in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Walking underlies many physical functions and reflects the interaction of several underlying systems, such as the central and peripheral nervous, sensory, muscular, skeletal, and cardiopulmonary (Ferrucci et al. 2000). A dysfunction in any system may slow walking speed. Therefore, walking speed is an important indicator of health status and function and can be used as a ‘vital sign’ (Fritz and Lusardi 2009; Studenski et al. 2011; Taekema et al. 2012). It has been shown that walking speed associates with aspects of poor health status or outcomes in older adults, such as mortality (Abellan van Kan et al. 2009; Cesari et al. 2005; Newman et al. 2006; Toots et al. 2013), mobility impairment (Newman et al. 2006; Purser et al. 2005; Rolland et al. 2004), falls (Abellan van Kan et al. 2009; Montero-Odasso et al. 2005), presence of cognitive impairment (Auyeung et al. 2008; Camicioli et al. 1998), cardiopulmonary diseases (Dumurgier et al. 2010; Ilgin et al. 2011; Newman et al. 2006; Rosano et al. 2011), hospitalization, and nursing home placement (van Abellan et al. 2009; Cesari et al. 2005; Giuliani et al. 2008; Montero-Odasso et al. 2005). Cut-off values for walking speed are used for the prediction of aforementioned health outcomes and underpin clinical decision making.
Walking speed is often measured in clinical practice as part of a comprehensive geriatric assessment (CGA) (Peel et al. 2013) and in clinical research (Graham et al. 2008a). It is a quick and easy measure and is not limited to specific equipment. Furthermore, it is a valid, sensitive, and specific measure with high inter-rater and test-retest reliability (Bellet et al. 2012; Munoz-Mendoza et al. 2011; Nasuti et al. 2013; Rydwik et al. 2012). Currently, there are many methods to assess walking speed varying in pace (i.e., normal or as fast as possible), static or dynamic start, and walking distance or time. Previous research showed conflicting results regarding methodologically induced variance in assessed walking speed in elderly (Ng et al. 2013; Peters et al. 2013). This hampers comparison of the different studies and may affect the clinical interpretation of walking speed (Graham et al. 2008b; Rydwik et al. 2012).
In this study, we assessed the influence of different assessment methods on walking speed in a clinically relevant population of community-dwelling elderly referred to a geriatric outpatient clinic. The walking tests varied in distance or time and static or dynamic start. Furthermore, we examined the association of walking speed assessed by different methods with the presence of low cognitive performance and cardiopulmonary disease as key aspects of poor health status influencing walking speed.
Methods
Setting
This cross-sectional study included 299 community-dwelling elderly referred to a geriatric outpatient clinic in a middle-sized teaching hospital (Bronovo Hospital, The Hague, the Netherlands) for a CGA between October 2010 and January 2012. CGA was performed during a 2-h visit including questionnaires and measurements of physical and cognitive performance. Trained nurses or medical staff performed all tests. Medical charts were evaluated retrospectively. As this study is based on regular medical care, the need for individual informed consent was waived. In the present analyses, 11 (3.7 %) patients were excluded due to missing data on all three walking tests (10 due to physical impairments and 1 due to time constraints), resulting in 288 patients.
Outpatient characteristics
The patients completed the questionnaires which provided the information on age, gender, marital status, living arrangements, smoking, and alcohol use. Body mass index (BMI) was calculated by dividing body weight in kilograms by the square of the height in meters. Medical charts were used to determine use of medication and presence of diseases, i.e., hypertension, myocardial infarction, chronic obstructive pulmonary disease (COPD), malignancy, diabetes mellitus, rheumatoid arthritis, (osteo)arthritis, and Parkinson’s disease. Multimorbidity was defined as having two or more diseases. The presence of cardiopulmonary disease was defined as having one or more diseases and risk factors relating to the cardiovascular and/or pulmonary system, i.e., hypertension, myocardial infarction, and COPD. Depressive symptoms were assessed by the Hospital Anxiety and Depression Scale (HADS) (Zigmond and Snaith 1983); a depression subscore higher than 8 out of 21 points indicated depressive symptoms. Cognition was assessed through the Mini-Mental State Examination (MMSE) (Folstein et al. 1975). A relative MMSE score was calculated by dividing the total MMSE score by the maximal possible MMSE score multiplied by 30. The presence of low cognitive performance was defined as scoring below the clinically used cut-off value of 24 points (Lezak et al. 2004). Physical functioning was assessed by handgrip strength, the Short Physical Performance Battery (SPPB) (Guralnik et al. 1994), and questionnaires about walking difficulties and the use of a walking aid.
Walking speed
Walking speed was assessed with the 4-m, 10-m, and 6-min walking tests. Patients wore non-slip socks during the 4- and 10-m walking tests and their regular shoes during the 6-min walking test. The walking tests were performed without walking aid, unless the patients were not able to.
The 4-m walking test was assessed as part of the SPPB and was performed twice. Patients started from standing position and were instructed to walk at their preferred speed over a length of 5 m, without slowing down before the 4-m line. Time was measured using a hand-held stopwatch from the moment the first foot passed the starting line until the moment the first foot passed the 4-m line completely. The shortest time was used for analysis.
The 10-m walking test was performed twice, and patients were instructed to walk at their preferred speed over a length of 15 m. Time was started at 2.5 m and stopped at 12.5 m, resulting in a steady-state measurement over 10 m. Time was measured using a hand-held stopwatch, and the shortest time was used for analysis.
The 6-min walking test was performed once and patients were instructed to walk as far as possible, without running, for 6 min. The test started from standing position and stopped after 6 min or if patients could not walk further. Patients walked down a corridor of 15 m, and the number of times patients walked down the corridor was recorded manually plus any residual distance. A Dynaport Hybrid (McRoberts B.V., The Hague, The Netherlands), a tri-axial accelerometer positioned on the lower back using an elastic strap at the height of the second lumbar vertebra, was used as a second measure of total walking distance. The number of turns was established off line by custom-written software using Matlab (The MathWorks Inc., Natick, MA, USA). Subsequently, the counted turns were multiplied by 15 and the reported residual distance was added. For the current analysis, the total distance calculated using the Dynaport Hybrid was used for further analysis. As the 6-min walking test was only performed between October 2010 and March 2011, data was available in 70 patients, of which 7 (12.9 %) patients were not able to finish the test due to fatigue or shortness of breath.
Statistical analysis
The continuous variables with Gaussian distribution are presented as mean and standard deviation (SD), otherwise as median and interquartile range (IQR) or as number (n) and percentage (%). Paired samples t tests were used to assess the systematic error, i.e., the mean difference, between the different methods to assess walking speed, i.e., 4- versus 10-m, 4-m versus 6-min, and 10-m versus 6-min walking test. The absolute agreement was assessed by the 95 % limits of agreement (95 % LOA), which were calculated by the mean difference ± 1.96 SD (Bland and Altman 1986, 1999) and visualized using Bland-Altman plots. The relative agreement was assessed by the intraclass correlation coefficient (ICC3,1) (Shrout and Fleiss 1979). The ICC values were interpreted as excellent (0.75 or higher), fair to good (0.40 to 0.75), or poor (0.40 or lower) (Peters et al. 2013). The association of cognitive performance and cardiopulmonary diseases with walking speed assessed by three different walking tests was tested using linear regression analysis without and with adjustments for age and gender. Data was analyzed using SPSS version 20.0 for Windows (SPSS Inc., Chicago, IL, USA). The p values below 0.05 were considered statistically significant.
Results
Outpatient characteristics
The characteristics of the elderly outpatients are shown in Table 1. Mean age (SD) was 82.2 years (7.1) and 35.1 % were men.
Comparison of walking speed assessed with different methods
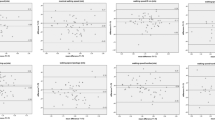
The mean differences between walking speeds assessed with different walking tests are presented in Table 2 and visualized in Fig. 1. Walking speed assessed with the 10-m walking test was significantly higher compared to the walking speed assessed with the 4-m and 6-min walking tests. Walking speed assessed with the 4-m and 6-min walking tests was not significantly different. The 95 % LOA of the comparison of the 4- and 10-m walking tests were lower than the 95 % LOA of the comparison of the 6-min walking test and the 4-m walking test, and the 95 % LOA of the comparison of the 6-min walking test and the 10-m waking test. The ICC between the 4- and the 10-m walking tests was excellent. The ICCs between the 4-m and 6-min walking tests and between the 10-m and 6-min tests were fair to good.
Bland-Altman plots of walking speed. Bland-Altman plot representing the comparison between a the 4 and 10-m walking speeds, b the 4-m and 6-min walking speeds, and c the 10-m and 6-min walking speeds. The solid line represents the mean difference in walking speed, while the dashed lines represent the upper and lower 95 % limits of agreement (mean difference ± 1.96 SD)
Association of underlying systems with walking speed
Table 3 shows the association of the presence of low cognitive performance and cardiopulmonary disease with walking speed assessed with different walking tests. The presence of low cognitive performance was significantly associated with a lower 4-m walking speed and 10-m walking speed after adjustments for age and gender, of which the 4-m walking speed showed the highest effect size. The presence of cardiopulmonary disease was significantly associated with a lower 4-m, 10-m, and 6-min walking speed after adjustments for age and gender, of which the 6-min walking speed showed the highest effect size.
Discussion
In a population of community-dwelling elderly referred to a geriatric outpatient clinic, the walking speed was assessed with three different methods, i.e., the 4-m, the 10-m, and the 6-min walking tests. The walking speed assessed with the 10-m walking test was significantly higher compared to walking speed assessed with the 4-m and 6-min walking tests. ICC values indicated excellent agreement for the comparison between the 4- and 10-m walking tests and fair to good agreement for the 4-m and 6-min walking tests and for the 10-m and 6-min walking tests. The presence of low cognitive performance showed the strongest association with walking speed assessed with the 4-m walking test, while the presence of cardiopulmonary disease showed the strongest association with walking speed assessed with the 6-min walking test.
No previous studies investigated the influence of different methods to assess walking speed in a clinically relevant population of elderly outpatients with comorbidities and mobility impairments. A previous study in a homogeneous population of healthy elderly showed an excellent agreement in walking speed assessed with the 4- and 10-m walking tests (Peters et al. 2013), which is comparable with our results. A lower ICC value with larger 95 % LOA compared with aforementioned study can be explained by a difference in the study population and sample size. In contrast to the present results, other previous studies performed in healthy older adults and older adults with neurologic conditions reported no effect of walking distance on walking speed (Graham et al. 2008b; Ng et al. 2013). Apart from the differences in study population, it is difficult to compare aforementioned studies due to differences in test protocols, especially in pace and static or dynamic start of the walking test.
The walking speed assessed with the 10-m walking test was significantly higher compared to the walking speed assessed with the 4-m walking test. The higher walking speed assessed with the 10-m walking test can be explained by the exclusion of the acceleration phase, which is included in the 4-m walking test, while the 10-m walking test measures only the steady-state phase. The results showed an excellent relative agreement between the 4- and 10-m walking tests by the ICC. This means a high consistency between tests, i.e., smaller difference between both assessed walking speeds compared with the differences between the patients within the group. A small range of the 95 % LOA indicated a low random error and precise assessments of walking speeds.
A systematically lower walking speed assessed with the 6-min walking test compared to the 10-m walking test was found, which can be explained by the inclusion of the acceleration phase and the endurance needed to perform the 6-min walking test. The difference between both assessed walking speeds is somewhat higher compared to the differences between the patients in the study population, as shown by the ICC values indicating fair to good agreement. The large range of the 95 % LOA indicated a high random error and less precise assessments of walking speeds. This may be explained by the introduction of more variability due to the differences in endurance between patients. Furthermore, available data of the 6-min walking tests was limited.
We found no systematic difference between walking speed assessed with the 4-m and the 6-min walking tests. Both tests include factors with a limiting effect on the assessed walking speed, i.e., an acceleration phase and endurance. The first factor has less effect on walking speed assessed with the 6-min walking test, as the duration of the 6-min walking test is longer compared with the 4-m walking test. Endurance has effect only on the 6-min walking test. The results showed a fair-to-good relative agreement between the tests due to a somewhat higher difference between the tests compared with the differences within the group reflected by the ICC. A large range of the 95 % LOA indicates a high random error and less precision between the two assessed walking speeds. An explanation for this may be the introduction of more variability due to differences in endurance as well as the lower number of patients who performed the 6-min walking test compared to the 4-m walking test.
The methodology to assess walking speed affects the association of cognitive performance with walking speed. In accordance with other studies performed in community-dwelling elderly and healthy elderly (Atkinson et al. 2007; Auyeung et al. 2008; Blankevoort et al. 2013; Camicioli et al. 1998; Rosano et al. 2005; Soumare et al. 2009), we found an association between the presence of low cognitive performance and walking speed assessed by respectively the 4- and 10-m walking tests. The largest effect size was found for the walking speed assessed with the 4-m walking test. This may be explained by the inclusion of the acceleration phase in the 4-m walking test. The initiation of movement requires cognitive processes and therefore cognitive impairment slows walking (Auyeung et al. 2008; Soumare et al. 2009), resulting in a larger effect size for the association between the presence of low cognitive performance and the walking speed assessed with the 4-m walking test.
The methodology also affects the association between the presence of cardiopulmonary disease and walking speed. In accordance with the previous studies showing a negative association between hypertension, myocardial infarction, and COPD and walking speed (Dumurgier et al. 2010; Ilgin et al. 2011; Newman et al. 2006; Rosano et al. 2011), we found an association between the presence of cardiopulmonary disease with a lower walking speed. The highest effect size was found for the walking speed assessed with the 6-min walking test. This may be explained by the cardiovascular determined endurance factor, which is obviously more prominent in the 6-min walking test.
The results found in this study are of high clinical relevance. Previous studies reported clinically meaningful changes in walking speed in community-dwelling older adults for the 4-m walking test of 0.12 m/s (Perera et al. 2006). More in general, small and substantial clinically meaningful changes in walking speed were reported from 0.05 to 0.10 m/s, respectively (Bohannon and Glenney 2014; Perera et al. 2006). In this study, we found differences in walking speeds of 0.11 m/s for the 10-m compared to the 4-m walking test and 0.06 m/s for the 10-m compared to the 6-min walking test. Especially for the 10-m compared to the 4-m walking test, the range of 95 % LOA is small (0.10;0.13 m/s) indicating that for 95 % of the patients, the difference between the 10- and 4-m walking tests will be between these values. So, the difference between both walking tests is large and precise enough to measure clinically meaningful changes in walking speed over time at the individual level when these methods are used interchangeably, which will have a direct influence on clinical decision making. Furthermore, this study emphasizes that when using cut-off values (Abellan van Kan et al. 2009; Montero-Odasso et al. 2005; Studenski et al. 2003, 2011) for clinical decision making, clinicians should be aware that they depend on the assessment method of walking speed.
The strength of this study is the large clinically relevant study population of elderly outpatients. No exclusion criteria were applied which further improves the generalizability of our results. Within the study population 64.9% were women, representing the geriatric outpatient population. Limitations were the limited availability of data on the 6-min walking test. This could have influenced our results, as this reduces the power in the comparison of the 4- and 10-m walking tests with the 6-min walking test and results in a methodologically induced enhancement of the 95 % LOA and lower ICC values.
This study showed that in the clinically relevant population of elderly outpatients, the walking test that has been used has the direct influence on the assessed walking speed as well as its validity, illustrated by the association with two major underlying systems, i.e., cognition and the cardiopulmonary system. The walking speeds assessed by different walking tests are therefore not interchangeable in this population. Clinicians assessing elderly outpatients should be aware of the effect of the used walking test on the assessed walking speed and its consequences for clinical decision making.
References
Abellan van KG, Rolland Y, Andrieu S, Bauer J, Beauchet O, Bonnefoy M, Cesari M, Donini LM, Gillette Guyonnet S, Inzitari M, Nourhashemi F, Onder G, Ritz P, Salva A, Visser M, Vellas B (2009) Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging 13(10):881–889
Atkinson HH, Rosano C, Simonsick EM, Williamson JD, Davis C, Ambrosius WT, Rapp SR, Cesari M, Newman AB, Harris TB, Rubin SM, Yaffe K, Satterfield S, Kritchevsky SB (2007) Cognitive function, gait speed decline, and comorbidities: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 62(8):844–850
Auyeung TW, Kwok T, Lee J, Leung PC, Leung J, Woo J (2008) Functional decline in cognitive impairment–the relationship between physical and cognitive function. Neuroepidemiology 31(3):167–173
Bellet RN, Adams L, Morris NR (2012) The 6-minute walk test in outpatient cardiac rehabilitation: validity, reliability and responsiveness–a systematic review. Physiotherapy 98(4):277–286
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat Methods Med Res 8(2):135–160
Blankevoort CG, Scherder EJA, Wieling MB, Hortobagyi T, Brouwer WH, Geuze RH, van Heuvelen MJG (2013) Physical predictors of cognitive performance in healthy older adults: a cross-sectional analysis. PLoS ONE 8(7):e70799
Bohannon RW, Glenney SS (2014) Minimal clinically important difference for change in comfortable gait speed of adults with pathology: a systematic review. J Eval Clin Pract 20(4):295–300
Camicioli R, Howieson D, Oken B, Sexton G, Kaye J (1998) Motor slowing precedes cognitive impairment in the oldest old. Neurology 50(5):1496–1498
Cesari M, Kritchevsky SB, Penninx BWHJ, Nicklas BJ, Simonsick EM, Newman AB, Tylavsky FA, Brach JS, Satterfield S, Bauer DC, Visser M, Rubin SM, Harris TB, Pahor M (2005) Prognostic value of usual gait speed in well-functioning older people–results from the health, aging and body composition study. J Am Geriatr Soc 53(10):1675–1680
Dumurgier J, Elbaz A, Dufouil C, Tavernier B, Tzourio C (2010) Hypertension and lower walking speed in the elderly: the Three-City study. J Hypertens 28(7):1506–1514
Ferrucci L, Bandinelli S, Benvenuti E, Di IA, Macchi C, Harris TB, Guralnik JM (2000) Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InCHIANTI study. J Am Geriatr Soc 48(12):1618–1625
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Fritz S, Lusardi M (2009) White paper: “walking speed: the sixth vital sign”. J Geriatr Phys Ther 32(2):46–49
Giuliani CA, Gruber-Baldini AL, Park NS, Schrodt LA, Rokoske F, Sloane PD, Zimmerman S (2008) Physical performance characteristics of assisted living residents and risk for adverse health outcomes. Gerontologist 48(2):203–212
Graham JE, Ostir GV, Fisher SR, Ottenbacher KJ (2008a) Assessing walking speed in clinical research: a systematic review. J Eval Clin Pract 14(4):552–562
Graham JE, Ostir GV, Kuo YF, Fisher SR, Ottenbacher KJ (2008b) Relationship between test methodology and mean velocity in timed walk tests: a review. Arch Phys Med Rehabil 89(5):865–872
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB (1994) A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 49(2):M85–M94
Ilgin D, Ozalevli S, Kilinc O, Sevinc C, Cimrin AH, Ucan ES (2011) Gait speed as a functional capacity indicator in patients with chronic obstructive pulmonary disease. Ann Thorac Med 6(3):141–146
Lezak MD, Howieson DB, Loring DW (2004) Neuropsychological assessment, 4th edn. Oxford University Press, New York
Montero-Odasso M, Schapira M, Soriano ER, Varela M, Kaplan R, Camera LA, Mayorga LM (2005) Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci 60(10):1304–1309
Munoz-Mendoza CL, Cabanero-Martinez MJ, Millan-Calenti JC, Cabrero-Garcia J, Lopez-Sanchez R, Maseda-Rodriguez A (2011) Reliability of 4-m and 6-m walking speed tests in elderly people with cognitive impairment. Arch Gerontol Geriatr 52(2):e67–e70
Nasuti G, Stuart-Hill L, Temple VA (2013) The six-minute walk test for adults with intellectual disability: a study of validity and reliability. J Intellect Dev Disabil 38(1):31–38
Newman AB, Simonsick EM, Naydeck BL, Boudreau RM, Kritchevsky SB, Nevitt MC, Pahor M, Satterfield S, Brach JS, Studenski SA, Harris TB (2006) Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA 295(17):2018–2026
Ng SSM, Ng PCM, Lee CYW, Ng ESW, Tong MHW, Fong SSM, Tsang WWN (2013) Assessing the walking speed of older adults: the influence of walkway length. Am J Phys Med Rehabil 92(9):776–780
Peel NM, Kuys SS, Klein K (2013) Gait speed as a measure in geriatric assessment in clinical settings: a systematic review. J Gerontol A Biol Sci Med Sci 68(1):39–46
Perera S, Mody SH, Woodman RC, Studenski SA (2006) Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 54(5):743–749
Peters DM, Fritz SL, Krotish DE (2013) Assessing the reliability and validity of a shorter walk test compared with the 10-meter walk test for measurements of gait speed in healthy, older adults. J Geriatr Phys Ther 36(1):24–30
Purser JL, Weinberger M, Cohen HJ, Pieper CF, Morey MC, Li T, Williams GR, Lapuerta P (2005) Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev 42(4):535–546
Rolland YM, Cesari M, Miller ME, Penninx BW, Atkinson HH, Pahor M (2004) Reliability of the 400-m usual-pace walk test as an assessment of mobility limitation in older adults. J Am Geriatr Soc 52(6):972–976
Rosano C, Simonsick EM, Harris TB, Kritchevsky SB, Brach J, Visser M, Yaffe K, Newman AB (2005) Association between physical and cognitive function in healthy elderly: the health, aging and body composition study. Neuroepidemiology 24(1–2):8–14
Rosano C, Longstreth WT Jr, Boudreau R, Taylor CA, Du Y, Kuller LH, Newman AB (2011) High blood pressure accelerates gait slowing in well-functioning older adults over 18-years of follow-up. J Am Geriatr Soc 59(3):390–397
Rydwik E, Bergland A, Forsen L, Frandin K (2012) Investigation into the reliability and validity of the measurement of elderly people’s clinical walking speed: a systematic review. Physiother Theory Pract 28(3):238–256
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86(2):420–428
Soumare A, Tavernier B, Alperovitch A, Tzourio C, Elbaz A (2009) A cross-sectional and longitudinal study of the relationship between walking speed and cognitive function in community-dwelling elderly people. J Gerontol A Biol Sci Med Sci 64(10):1058–1065
Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, Fox M, Guralnik JM (2003) Physical performance measures in the clinical setting. J Am Geriatr Soc 51(3):314–322
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, Guralnik J (2011) Gait speed and survival in older adults. JAMA 305(1):50–58
Taekema DG, Gussekloo J, Westendorp RG, de Craen AJ, Maier AB (2012) Predicting survival in oldest old people. Am J Med 125(12):1188–1194
Toots A, Rosendahl E, Lundin-Olsson L, Nordstrom P, Gustafson Y, Littbrand H (2013) Usual gait speed independently predicts mortality in very old people: a population-based study. J Am Med Dir Assoc 14(7):529–6
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67(6):361–370
Acknowledgments
This research is supported by the Dutch Technology Foundation STW, which is part of the Netherlands Organization for Scientific Research (NWO) and which is partly funded by the Ministry of Economic Affairs. Furthermore, this work is supported by an unrestricted grant from the Netherlands Organization of Scientific Research (ZonMw), the Ministry of Health, Welfare and Sports, the Netherlands Genomics Initiative/Netherlands Organization for scientific research (NGI/NWO; 05040202 and 050-060-810 Netherlands Consortium for Healthy Ageing (NCHA)) and the seventh framework program MYOAGE (HEALTH-2007-2.4.5-10).
Author information
Authors and Affiliations
Corresponding author
Additional information
Jantsje H. Pasma and Marjon Stijntjes contributed equally to this study.
About this article
Cite this article
Pasma, J.H., Stijntjes, M., Ou, S.S. et al. Walking speed in elderly outpatients depends on the assessment method. AGE 36, 9736 (2014). https://doi.org/10.1007/s11357-014-9736-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-014-9736-y