Abstract
Osteoporosis is a common systemic skeletal disease that predominantly affects people older than 50 years and often co-occurs with dementia. The purpose of this study was to evaluate the risk of dementia in osteoporosis patients in Taiwan. Using data from Taiwan's National Health Insurance Research Database (NHIRD), we identified 23,941 patients with osteoporosis from 2000 to 2010 and 47,579 nonosteoporosis control patients, frequency-matched for age, sex, and index year, excluding patients with dementia at the baseline. We conducted univariate and multiple Cox proportional-hazards regression analyses to calculate the hazard ratios (HRs) and 95 % confidence intervals (CIs) of the association between osteoporosis and risk of dementia. After adjustment for potential risk factors, the osteoporosis patients exhibited 1.46-fold and 1.39-fold higher risk of dementia (95 % CI = 1.37–1.56) and Alzheimer's disease (95 % CI = 0.95–2.02), respectively, compared with the matched nonosteoporosis patients. We observed increased risk of dementia in both men and women with osteoporosis. The osteoporosis patients receiving bisphosphonate treatment or estrogen supplementation were associated with significantly lower risk of dementia compared with the osteoporosis patients who did not receive any treatment. Overall, our results suggest higher risks of dementia in osteoporosis patients than in nonosteoporosis patients. Osteoporosis could thus be considered an early risk factor for dementia. Future large-scale double-blind randomized clinical trials are required to clarify the role of medication in osteoporosis-related dementia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a common systemic skeletal disease that predominantly affects people older than 50 years (Tysiewicz-Dudek et al. 2008) and often co-occurs with dementia (Weller and Schatzker 2004). Approximately 4.6 million people are diagnosed with dementia annually, with an approximate doubling of the dementia population every 20 years. By 2020, the dementia population is expected to have increased to 42.3 million worldwide, with 81.1 million people predicted to be affected by 2040 (Ferri et al. 2005). Alzheimer's disease (AD) is the most common form of dementia and constitutes approximately 50–70 % of all cases (Fratiglioni et al. 1991). In the United States, AD is the sixth leading cause of death in the general population, and the fifth leading cause of death in people aged 65 years and older (Alzheimer’s Association 2012). AD can induce falls, which can cause fractures, particularly in the hip (Fujiwara et al. 1997; Cummings et al. 1995; Buchner and Larson 1987; Weller 2000; Weller and Schatzker 2004). Among elderly people, hip fractures are associated with higher morbidity and mortality rates compared with other osteoporotic fractures (Kanis et al. 2001, 2008; Masud and Morris 2001). Chang et al. (2004) identified that hip fracture is the most common morbidity among osteoporosis patients. Osteoporosis and dementia have several common risk factors, including older age, female sex, smoking, excessive drinking, low levels of estrogen and vitamin D3, family history, and the ApoE genotype (Yaffe et al. 2012). Other clinical conditions, such as cardiovascular diseases, depression, head trauma, and diabetes, might also be associated with osteoporosis (Patterson et al. 2008). However, a possible causal relationship between osteoporosis and dementia has yet to be evaluated (Tan et al. 2005). Therefore, we conducted a retrospective cohort analysis to evaluate the association between osteoporosis and dementia in Taiwan.
Materials and methods
Data source and study population
The National Health Insurance (NHI) program is a single-payer compulsory health insurance system that has provided insurance coverage to almost every citizen in Taiwan since 1995. By the end of 2009, approximately 99 % of 23.74 million Taiwanese citizens were enrolled in this program. Those without enrollment include unemployed or self-employed people, or people living in remote areas or overseas (Cheng 2009; Lu and Hsiao 2003). The National Health Research Institutes (NHRI) maintains the National Health Insurance Research Database (NHIRD), which is accessible to investigators and the public in Taiwan. This study used a subset of the NHIRD containing comprehensive health care data on the ambulatory care claims, inpatient claims, and prescriptions of 1,000,000 people randomly selected from all insured beneficiaries. These data files are linkable through an encrypted and unique personal identification number, and thus provide a longitudinal medical history of each individual patient. Diagnoses were based on the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). This study was approved by the Institutional Review Board of China Medical University (CMU-REC-101-012).
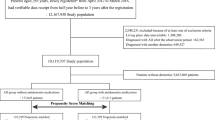
Study patients
A retrospective cohort analysis was conducted to evaluate the association between osteoporosis (including osteoporotic fractures) (ICD-9-CM codes 733.0 and 733.1) and dementia (ICD-9-CM codes 290, 294.1, and 331.0). Patients with osteoporosis (ICD-9-CM code 733.0) and osteoporotic fracture (ICD-9-CM code 733.1) were included in the study cohort because osteoporosis is an underdiagnosed disease (Haasum et al. 2012). A primary discharge diagnosis of osteoporosis was used to identify all patients diagnosed with new-onset osteoporosis from 2000 to 2010. The exclusion criteria were age <50 years and a history of dementia at baseline. Patients without osteoporosis were randomly selected from the NHIRD as the comparison cohort, frequency-matched to the study cohort according to age (every 5 years), sex, and index year, and subjected to the same exclusion criteria as the study cohort. Overall, this study included 23,941 osteoporosis patients and 47,579 control patients. All patients were followed up until December 31, 2010, or until loss to follow-up, death, or withdrawal from the insurance system.
Definitions
The following variables were considered: age (50–59, 60–69, 70–79, and ≥80 years) and sex (male or female). Premium-based income was categorized into three levels: <528, 528–640, and >640 US dollars (USD) (equivalent to <15,840, 15,840–19,200, and ≥19,200 New Taiwan Dollars [NTD]) (1 USD = 30 NTD). The occupation categories included public servants, workers in the labor sector (farmers, fishermen, and industry workers), businessmen, low-income earners, and others. A low income was defined as a monthly income lower than the level required for paying a premium. Patients with a baseline comorbidity were identified using the ICD-9-CM code and the Anatomical Therapeutic Chemical (ATC) code for medication. Comorbidities included stroke (ICD-9-CM codes: 430–438), head injury (ICD-9-CM codes: 850–854, 95901), depression (ICD-9-CM codes: 296.2, 296.3, 300.4, 31), estrogen supplementation (ATC codes: G03CA01, G03CA03, G03CA04, G03CA06, G03CA07, G03CA09, G03CA53, G03CA57), and bisphosphonate treatment (ATC codes: M05BA01, M05BA02, M05BA03, M05BA04, M05BA05, M05BA06, M05BA07, M05BA08), which is the primary treatment for osteoporosis.
Statistical analysis
The associations between the variables and osteoporosis were evaluated using the chi-square test (Table 1). The age-specific and comorbidity-specific incidence density rates of dementia were calculated in each cohort in person-years, and the incidence rate ratio (IRR) of each variable was estimated using a Poisson regression. Univariate and multiple Cox proportional hazards regression analyses were conducted to calculate the hazard ratios (HRs) and 95 % confidence intervals (CIs) of the association between the risk of dementia and osteoporosis, controlling for the sociodemographic characteristics and comorbid conditions. The plot of the Kaplan–Meier analysis was used to identify the probability of a person remaining without dementia, and the log-rank test was used to evaluate the differences in the risk of dementia between patients with and without osteoporosis. All analyses were performed using SAS 9.2 (SAS Institute Inc., Cary, NC, USA). The Kaplan–Meier survival curve was plotted using R software (R Foundation for Statistical Computing, Vienna, Austria). Statistical tests were considered significant if p < 0.05 for two-tailed values.
Results
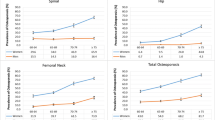
Table 1 shows the sociodemographic characteristics and baseline comorbidity statuses of the patients in the osteoporosis and nonosteoporosis cohorts. Because of frequency matching, the age and sex distributions in the two cohorts were well balanced. In both cohorts, approximately 46 % of the patients were labor sector workers. The osteoporosis patients were more likely to have a stroke (21.6 % vs. 15.2 %, p < 0.0001), head injury (5.01 % vs. 3.14 %, p < 0.0001), and depression (7.55 % vs. 4.30 %, p < 0.0001) compared with the nonosteoporosis patients. The percentage of patients receiving estrogen supplementation was significantly higher in the osteoporosis patients than in the nonosteoporosis patients. The incidence density rates of dementia were approximately 11.9 and 7.0 per 1,000 person-years in the osteoporosis and nonosteoporosis cohorts, respectively (Table 2). The overall IRR of dementia was 71 % higher in the osteoporosis cohort than in the nonosteoporosis cohort, with an adjusted HR of 1.46 (95 % CI, 1.37–1.56). Following age stratification, the incidence rate of dementia increased with age in both cohorts. We observed the highest IRRs and adjusted HRs in the patients aged 50–59 years.
The osteoporosis patients with or without comorbidities were associated with significantly higher risk of dementia than the nonosteoporosis patients were. Table 3 shows the incidence rates and adjusted HRs of dementia and AD in the osteoporosis and nonosteoporosis cohorts. The patients with osteoporosis or pathologic fracture exhibited 1.59-fold (95 % CI = 1.48–1.70) and 1.94-fold (95 % CI = 1.19–3.18) higher risk of developing dementia, respectively, compared with the patients without osteoporosis or pathologic fracture. The patients with osteoporosis were also associated with 1.47-fold higher risk of developing AD (95 % CI = 1.10–1.98) compared with the nonosteoporosis patients, although we did not observe the same trend in the patients with pathologic fracture. Figure 1 shows the Kaplan–Meier curves of freedom for dementia in patients with and without osteoporosis. The patients with osteoporosis were associated with significantly higher risk of dementia compared with the patients without osteoporosis (log-rank test, p < 0.0001). As shown in Table 4, when we analyzed the effects of medication on the risk of dementia in all osteoporosis patients, the osteoporosis patients receiving bisphosphonate treatment, estrogen supplementation, or both, exhibited 0.73-fold, 0.76-fold, and 0.53-fold lower risk of dementia, respectively, than did the osteoporosis patients not receiving any treatment (all p < 0.001).
Discussion
According to our research, our study is the first nationwide population-based study to investigate the risk of dementia in osteoporosis patients in Taiwan. We observed significantly higher risk of dementia in the osteoporosis patients compared with the nonosteoporosis patients. This finding was observed in men and in women. Our results were consistent with those from previous studies, in which low bone mineral density (BMD) and osteoporosis were associated with increased risk of AD (Chang et al. 2004; Loskutova et al. 2009; Häussler et al. 2007; Cheng 2009).
In Taiwan, a diagnosis of osteoporosis is based on the patient's BMD measurements, captured using dual X-ray absorptiometry (in the hip and spine) and ultrasound densitometry (in the heel), and defined as a BMD < (mean − 2.5 SD) of the population. Our findings contrasted with the results of some previous studies, in which osteoporosis was not associated with increased risk of dementia (Wright 2007; Haasum et al. 2012; Giangregorio et al. 2009). However, these studies used a patient's medication to identify a diagnosis of osteoporosis, which could have led to the underestimation of the sample size. We identified our osteoporosis patients using their medication and by referring to their clinical examination results to increase the validity of diagnoses.
Previous studies have observed a negative correlation between estrogen and the risk of osteoporosis or dementia (Tan et al. 2005; Yaffe et al. 1999; Henderson 2009). Jilka et al. (1992) described that reduced estrogen levels can promote the development of osteoclasts. Our evaluations of the effects of estrogen supplementation among the osteoporosis patients indicated lower risk of dementia in the patients receiving estrogen supplementation compared with those not receiving any treatment. However, because of estrogen supplementation for osteoporosis prevention, a person who receives estrogen supplementation is not necessarily an osteoporosis patient (Orimo et al. 2012). The most common medication prescribed to osteoporosis patients in Taiwan is bisphosphonates, which can cause apoptosis in osteoclasts (Hughes et al. 1995). Therefore, bisphosphonates would only be prescribed after a confirmed medical diagnosis of osteoporosis. Our results indicated a negative correlation between osteoporosis treatment and the risk of dementia among osteoporosis patients, particularly in those receiving both bisphosphonates and estrogen supplementation. In previous observational studies, hormone or estrogen therapy reduced the incidence, or delayed the onset, of dementia, primarily AD (Yaffe et al. 1998; Zandi et al. 2002). Estrogen receptors exist on cholinergic neurons and exert neurotropic, antioxidant, and anti-inflammatory effects (Schneider and Finch 1997; Turgeon et al. 2004). Patients with dementia are less likely to receive osteoporosis medication, such as bisphosphonates, than patients without dementia, and — if prescribed — the medication might be of low potency (Haasum et al. 2012).
Unhealthy behaviors, such as cigarette smoking and alcohol drinking, are associated with increased risk of AD and osteoporosis (Cheng 2009; Tysiewicz-Dudek et al. 2008; Zhou et al. 2011; Cataldo et al. 2011; Deng et al. 2010; Oddo et al. 2005; Juan et al. 2004; Peters et al. 2008). In previous studies, the prevalence rate of cigarette smoking and alcohol consumption was 3–4 % and 1 %, respectively, in women aged over 16 years (Deng et al. 2006; Anstey et al. 2009). In Taiwan, women are not encouraged to smoke or to drink alcohol, and are described as more able to reject offers of cigarettes and alcohol than men are (Annual Report of Tobacco, Alcohol Consumption Investigation in Taiwan Area 1993). Because of the differing prevalence of alcohol consumption and cigarette smoking between men and women in Taiwan, as well as the absence of detailed information on drinking and smoking habits in the NHIRD, we used sex as a proxy variable for alcohol drinking and cigarette smoking in our analyses.
This study has several limitations. First, the potential exists for the underdiagnosis and undertreatment of osteoporosis in people with dementia. Patients with severe dementia are less likely to receive osteoporosis treatment (Jilka et al. 1992). Second, the NHIRD does not contain detailed information on patients' smoking habits, alcohol consumption, socioeconomic status, or family history of systemic diseases, all of which could represent risk factors for osteoporosis or dementia (Orimo et al. 2012; Hughes et al. 1995). Third, the statistical quality of a retrospective cohort study is regarded as lower than that of a randomized trial because of potential biases related to adjustments for confounding variables. Fourth, our evaluations of the effects of estrogen supplementation among the osteoporosis patients indicated lower risk of dementia in the patients receiving estrogen supplementation compared with those not receiving any treatment. However, some of the estrogen supplementation could have been for local treatment; thus, not having any major systemic effects. Finally, all data in the NHIRD are anonymous and clinical variables such as blood pressure, estrogen levels, imaging results, pathology results, and serum laboratory data were unavailable for our study patients. However, the data on osteoporosis and dementia diagnoses were reliable.
To avoid the underdiagnosis of osteoporosis affecting our outcome estimation, we included patients with osteoporosis fracture (ICD-9 733.1) in the study cohort (Haasum et al. 2012). Study subjects with the diagnosis of osteoporosis from1996 to 1999 were excluded at the baseline to begin the identification of patients with osteoporosis newly diagnosed from 2000 to 2010. Therefore, most of prevalence cases of osteoporosis were not likely included in the study cohort. Furthermore, our follow-up period is long enough to identify incident patients of dementia.
Conclusion
The findings from our large retrospective population-based analysis indicate increased risk of dementia in patients with osteoporosis in Taiwan. However, estrogen supplementation and bisphosphonate treatment are associated with reduced risk of dementia among these osteoporosis patients. Further large double-blind randomized clinical trials are required to confirm these results.
References
Alzheimer’s Association (2012) 2012 Alzheimer’s disease facts and figures. Alzheimers Dement 8:131–168
Annual Report of Tobacco, Alcohol Consumption Investigation in Taiwan Area. Taipei, Taiwan: Bureau of Tobacco and Alcohol Monopoly, Taiwan Provincial Government, 1993
Anstey KJ, Mack HA, Cherbuin N (2009) Alcohol consumption as a risk factor for dementia and cognitive decline: meta-analysis of prospective studies. Am J Geriatr Psychiatry 17:542–555
Buchner DM, Larson EB (1987) Falls and fractures in patients with Alzheimer-type dementia. JAMA 257:1492–1495
Cataldo JK, Prochaska JJ, Glantz SA (2011) Cigarette smoking is a risk factor for Alzheimer’s disease: an analysis controlling for tobacco industry affiliation. J Alzheimers Dis 24:101–108
Chang KP, Center JR, Nguyen TV, Eisman JA (2004) Incidence of hip and other osteoporotic fractures in elderly men and women: Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 19:532–536
Cheng TM (2009) Taiwan’s National Health Insurance system: high value for the dollar. In: Okma KGH, Crivelli L (eds) Six countries, six reform models: the health reform experience of Israel, the Netherlands, New Zealand, Singapore, Switzerland and Taiwan. World Scientific, New Jersey, pp 71–204
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med 332:767–773
Deng J, Zhou DH, Li J, Wang YJ, Gao C, Chen M (2006) A 2-year follow-up study of alcohol consumption and risk of dementia. Clin Neurol Neurosurg 108:378–383
Deng J, Shen C, Wang YJ, Zhang M, Li J, Xu ZQ, Gao CY, Fang CQ, Zhou HD (2010) Nicotine exacerbates tau phosphorylation and cognitive impairment induced by amyloid-beta 25-35 in rats. Eur J Pharmacol 637:83–88
Ferri CP, Prince M, Brayne C, Brodaty H, Fratiglioni L, Ganguli M, Hall K, Hasegawa K, Hendrie H, Huang Y, Jorm A, Mathers C, Menezes PR, Rimmer E, Scazufca M, Alzheimer's Disease International (2005) Global prevalence of dementia: a Delphi consensus study. Lancet 366:2112–2117
Fratiglioni L, Grut M, Forsell Y, Viitanen M, Grafström M, Holmén K, Ericsson K, Bäckman L, Ahlbom A, Winblad B (1991) Prevalence of Alzheimer’s disease and other dementias in an elderly urban population: relationship with age, sex, and education. Neurology 41:1886–1892
Fujiwara S, Kasagi F, Yamada M, Kodama K (1997) Risk factors for hip fracture in a Japanese cohort. J Bone Miner Res 12:998–1004
Giangregorio LM, Jantzi M, Papaioannou A, Hirdes J, Maxwell CJ, Poss JW (2009) Osteoporosis management among residents living in long-term care. Osteoporos Int 20:1471–1478
Haasum Y, Fastbom J, Fratiglioni L, Johnell K (2012) Undertreatment of osteoporosis in persons with dementia? A population-based study. Osteoporos Int 23:1061–1068
Häussler B, Gothe H, Göl D, Glaeske G, Pientka L, Felsenberg D (2007) Epidemiology, treatment and costs of osteoporosis in Germany—the BoneEVA Study. Osteoporos Int 18:77–84
Henderson VW (2009) Aging, estrogens, and episodic memory in women. Cogn Behav Neurol 22:205–214
Hughes DE, Wright KR, Uy HL, Sasaki A, Yoneda T, Roodman GD, Mundy GR, Boyce BF (1995) Bisphosphonates promote apoptosis in murine osteoclasts in vitro and in vivo. J Bone Miner Res 10:1478–1487
Jilka RL, Hangoc G, Girasole G, Passeri G, Williams DC, Abrams JS, Boyce B, Broxmeyer H, Manolagas SC (1992) Increased osteoclast development after estrogen loss: mediation by interleukin-6. Science 257:88–91
Juan D, Zhou DH, Li J, Wang JY, Gao C, Chen M (2004) A 2-year follow-up study of cigarette smoking and risk of dementia. Eur J Neurol 11:277–282
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–427
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY, Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committee of Scientific Advisors of the International Osteoporosis Foundation (IOF) (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19:399–428
Loskutova N, Honea RA, Vidoni ED, Brooks WM, Burns JM (2009) Bone density and brain atrophy in early Alzheimer’s disease. J Alzheimers Dis 18:777–785
Lu JF, Hsiao WC (2003) Does universal health insurance make health care unaffordable? Lessons from Taiwan. Health Aff 22:77–88
Masud T, Morris RO (2001) Epidemiology of falls. Age Ageing 30(Suppl 4):3–7
Oddo S, Caccamo A, Green KN, Liang K, Tran L, Chen Y, Leslie FM, LaFerla FM (2005) Chronic nicotine administration exacerbates tau pathology in a transgenic model of Alzheimer’s disease. Proc Natl Acad Sci U S A 102:3046–3051
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S (2012) Japanese 2011 guidelines for prevention and treatment of osteoporosis—executive summary. Arch Osteoporos 7:3–20
Patterson C, Feightner JW, Garcia A, Hsiung GY, MacKnight C, Sadovnick AD (2008) Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ 178:548–556
Peters R, Peters J, Warner J, Beckett N, Bulpitt C (2008) Alcohol, dementia and cognitive decline in the elderly: a systematic review. Age Ageing 37:505–512
Schneider LS, Finch C (1997) Can estrogen prevent neurodegeneration? Drugs Aging 11:87–95
Tan ZS, Seshadri S, Beiser A, Zhang Y, Felson D, Hannan MT, Au R, Wolf PA, Kiel DP (2005) Bone mineral density and the risk of Alzheimer disease. Arch Neurol 62:107–111
Turgeon JL, McDonnell DP, Martin KA, Wise PM (2004) Hormone therapy: physiological complexity belies therapeutic simplicity. Science 304:1269–1273
Tysiewicz-Dudek M, Pietraszkiewicz F, Drozdzowska B (2008) Alzheimer’s disease and osteoporosis: common risk factors or one condition predisposing to the other? Ortop Traumatol Rehabil 10:315–323
Weller II (2000) The relation between hip fracture and Alzheimer’s disease in the Canadian national population health survey health institutions data, 1994–1995. A cross-sectional study. Ann Epidemiol 10:461
Weller I, Schatzker J (2004) Hip fractures and Alzheimer’s disease in elderly institutionalized Canadians. Ann Epidemiol 14:319–324
Wright RM (2007) Use of osteoporosis medications in older nursing facility residents. J Am Med Dir Assoc 8:453–457
Yaffe K, Sawaya G, Lieberburg I, Grady D (1998) Estrogen therapy in postmenopausal women: effects on cognitive function and dementia. JAMA 279:688–695
Yaffe K, Browner W, Cauley J, Launer L, Harris T (1999) Association between bone mineral density and cognitive decline in older women. J Am Geriatr Soc 47:1176–1182
Yaffe K, Tocco M, Petersen RC, Sigler C, Burns LC, Cornelius C, Khachaturian AS, Irizarry MC, Carrillo MC (2012) The epidemiology of Alzheimer's disease: laying the foundation for drug design, conduct, and analysis of clinical trials. Alzheimers Dement 8:237–242
Zandi PP, Carlson MC, Plassman BL, Welsh-Bohmer KA, Mayer LS, Steffens DC, Breitner JC, Cache County Memory Study Investigators (2002) Hormone replacement therapy and the incidence of Alzheimer disease in older women: the Cache County Study. JAMA 288:2123–2129
Zhou R, Deng J, Zhang M, Zhou HD, Wang YJ (2011) Association between bone mineral density and the risk of Alzheimer’s disease. J Alzheimers Dis 24:101–108
Acknowledgments
This study was supported by grants from the study hospital (DMR-102-014 and DMR-102-023), the Taiwan Department of Health Clinical Trial and Research Center and for Excellence (DOH102-TD-B-111-004), the Taiwan Department of Health Cancer Research Center for Excellence (DOH102-TD-C-111-005), and the International Research-Intensive Centers of Excellence in Taiwan (I-RiCE) (NSC101-2911-I-002-303).
Conflict of interest
The authors declare that they have no conflicts of interest.
Author contributions
Conception and design: Kuang-Hsi Chang, Chia-Hung Kao. Administrative support: Cheng-Li Lin, Fung-Chang Sung, Chi-Jung Chung, Trong-Neng Wu. Collection and assembly of data: Kuang-Hsi Chang, Cheng-Li Lin, Chi-Jung Chung, Chia-Hung Kao. Data analysis and interpretation: Kuang-Hsi Chang, Chi-Jung Chung, Chia-Hung Kao. Manuscript preparation: All authors. Final approval of manuscript: All authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
K.-H. Chang and C.-J. Chung contributed equally to this work.
About this article
Cite this article
Chang, KH., Chung, CJ., Lin, CL. et al. Increased risk of dementia in patients with osteoporosis: a population-based retrospective cohort analysis. AGE 36, 967–975 (2014). https://doi.org/10.1007/s11357-013-9608-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-013-9608-x