Abstract
Background
While several studies assessed the relation between cigarette smoking and sleep, there are still very few studies assessing the effect of nicotine in cigarette smoking on sleep.
Aim
This study aimed to compare higher vs lower nicotine levels in cigarette smoking on sleep quality.
Methods
We used data from the recently released dataset for the Randomized Trial of Reduced-Nicotine Standards for Cigarettes. We included three groups in the current study: the least nicotine concentration (i.e., 0.4 mg/g), a moderate nicotine concentration (i.e., 5.2 mg/g), and the highest nicotine concentration (i.e., 15.8 mg/g). For each participant, we included data regarding baseline and the last follow up at 6 weeks, where we compared insomnia, sleep problems, and awakening at night, in addition to different depression and affect scores.
Results
A total of 360 patients were included in this study, with a mean age of 42.4 (±13.4) years. For the three nicotine groups (i.e., 0.4 mg/g, 5.2 mg/g, and 15.8 mg/g), we included 119 (33%), 122 (34%), and 119 (33%) participants. Among the high-nicotine-dose group, the number of participants who had worsened sleep was significantly higher than the number of those who had improved sleep (p = 0.01) after 6 weeks of consumption, where 37 (31%) had worsened sleep score after 6 weeks while only 19 (16%) had improved score compared with baseline.
Conclusion
While previous studies established a relation either between cigarette smoking and sleep or between nicotine patches and sleep, the present study is the first to establish that higher nicotine doses in cigarettes were associated with more sleep disturbances.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cigarette smoking has long been associated with difficulty in initiating and maintaining sleep [1]. Animal studies have revealed a change in sleep quality caused by the nicotine dose [2, 3], and several studies have pointed to this dose-dependent fashion in humans [4]. Different review articles previously examined the effect of cigarette smoking on sleep [4, 5]. In these reviews, only a few studies focused on assessing the effect of nicotine on sleep quality, where almost none of them compared different nicotine doses in cigarettes and their effect on sleep in a longitudinal design. The aim of the current study was to assess the effect of high-, moderate-, and low-nicotine doses in cigarettes on sleep disturbances after 6 weeks of consumption.
Materials and methods
We used data from the recently released dataset for the Randomized Trial of Reduced-Nicotine Standards for Cigarettes [6], a double-blind, parallel, randomized clinical trial. In this trial, a sample of 840 participants randomized to smoke for 6 weeks either their usual brand of cigarettes or one of six types of investigational cigarettes with nicotine content ranging from 0.4 mg per gram of tobacco to 15.8 mg per gram. Dataset were released on the 14th of February 2020, available at the National Institute on Drug Abuse data share website (https://datashare.nida.nih.gov). No institutional review board was requested as we used openly accessible data.
Participants
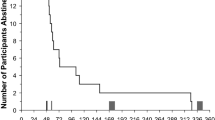
Included participants were adults above the age of 18 years, smoking of five or more cigarettes per day, and no current interest in quitting smoking. Of the six groups originally included in the randomized trial, we included three groups in the current study (Fig. 1); the least nicotine concentration (i.e., 0.4 mg/g), the moderate nicotine concentration (i.e., 5.2 mg/g), and the highest nicotine concentration (i.e., 15.8 mg/g). All included groups used the same cigarette paper, tipping paper, and dual plug (paper: cellulose acetate) filters. The number of cigarettes smoked was assessed through a handheld smoking topography device (CReSS Pocket, Borgwaldt), a commonly used device in clinical settings that measures the number and volume of puffs in real-time settings [7].
Variables
For each participant, we included data regarding baseline and the last follow-up at 6 weeks.
We included demographic variables, including age, gender, marital status (never married, married, separated, and widowed), living (alone, with family, with other than family), number of children and adults living with (more than 5 members is considered 6), education (up to high school, college undergraduate, college graduate), employment (full time, part-time, unemployed, or other, which include retirement, disability among others).
We measured depression via the Center for Epidemiologic Studies Depression Scale (CESD) [8]. We also used the Positive and Negative Affect Schedule (PANAS) scale to describe emotions, including positive and negative affect [9]. Our dependent variable was asking about insomnia, sleep problems, and awakening at night, where the participant grade his/her symptom on a scale from 0 to 4: 0 = none, 1 = slight, 2 = mild, 3 = moderate, 4 = severe. This question was asked as part of the Minnesota Nicotine Withdrawal Scale (MNWS) and was previously found to be an independent item that may be used to reflect sleep disturbances as part of nicotine withdrawal effects [10, 11].
Statistical analysis
We used SPSS version 21.0 (Chicago, USA) in our analysis. We used mean (± standard deviation) to describe continuous variables (e.g., age). We used count (frequency) to describe other nominal variables (e.g., gender).
We used one-way ANOVA to analyze the difference between the three nicotine consumption groups and each of age, or depression score. We also performed one-way ANOVA to analyze the difference between change in sleep quality with depression and PANAS scale. We used chi-square test to analyze the difference between the three nicotine consumption groups with baseline characteristics and also between sleep quality change with the change number of cigarettes consumed during the follow-up period. We used the Kruskal-Wallis test to analyze the difference in the number of cigarettes consumed between the three groups at baseline. We performed the Wilcoxon signed-rank test to analyze the difference in sleep score and other variables at baseline and after 6 weeks for each group and reported the findings as:
-
Positive difference, where the sleep score improved at 6 weeks.
-
Negative difference, where the sleep score worsened at 6 weeks.
-
Ties, where the sleep score was the same at 6 weeks.
We used linear regression to analyze the factors impacting the depression at 6 weeks, where nicotine dose, PANAS score, and sleep disturbances were the independent variables used. All underlying assumptions were met. We adopted a p value of 0.05 as a significant threshold.
Results
A total of 360 patients were included in this study, with a mean age of 42.4 (± 13.4) years. They were 202 (56%) men and 158 (44%) women. For the lowest-nicotine group (i.e., 0.4 mg/g), 119 (33%) participants were included, 122 (34%) for the moderate-nicotine group (i.e., 5.2 mg/g), and 119 (33%) for the highest-nicotine group (i.e., 15.8 mg/g). Participants in the three groups did not differ in the number of cigarettes consumed at baseline (p = 0.551). Table 1 compares baseline characteristics between the three nicotine groups, where it shows no significant difference between the three nicotine dose groups in regard to baseline characteristics.
Among the high-nicotine-dose group, the number of participants who had worsened sleep was significantly higher than the number of those who had improved sleep (p = 0.01) after 6 weeks of consumption, where 37 (31%) had worsened sleep score after 6 weeks while only 19 (16%) had improved score compared with baseline. We did not find a significant change in sleep score between baseline and after 6 weeks period among both moderate- and low-nicotine-dose groups (Table 2). There was no significant difference between groups regarding the change in the number of daily cigarettes consumed (p = 0.358), or depression score (p = 0.531).
We calculated the difference in sleep quality before and after the intervention, and we categorized the sleep change into improved, same, or worsened. We analyzed the difference in depression change and PANAS change between the three groups (Table 3). We found that worsened sleep quality was significantly associated with both higher depression score (p < 0.001) and higher PANAS score (p = 0.013). Moreover, the depression score was significantly associated with both sleep disturbances and PANAS score (p < 0.001), but not nicotine dose (p = 0.967).
Discussion
Although previous studies pointed to the relationship between sleep quality and nicotine consumption [5, 12,13,14,15], this is the first study that established a relationship between higher and lower doses of nicotine consumption and sleep disturbances. We found that significantly more sleep disturbances and insomnia were observed for the high-nicotine group only after 6 weeks of follow-up, an increase that was not observed for the moderate- and low-nicotine groups. We also found that those who had worsened sleep had higher depression and PANAS scores.
Several studies assessed the effect of nicotine patches on sleep in different cohorts. In a study that assessed the effect of different doses of nicotine patches on healthy non-smokers (n = 66), the authors found that higher nicotine doses are associated with insomnia and sleep disturbances [5]. A smaller study on non-smokers (n = 12) found that nicotine patches reduced REM sleep in a dose-dependent fashion compared with placebo patches [15]. A study on heavy smokers (n = 23) compared the duration of nocturnal nicotine patch exposure on quality of sleep [14] and found that a prolonged nocturnal nicotine patch exposure improved the quality of sleep, in terms of prolonged slow-wave sleep. A previous study that assessed the factors affecting sleep quality during exam periods found that nicotine generally leads to diminished sleep quality [13].
Sleep disturbances and poor sleep quality are known to impair different life domains affecting people’s life, where cigarette smoking has long been studied as an independent risk factor to affect sleep. In a recent population-based survey, researchers found that smokers demonstrated poorer sleep quality and more sleep disturbances compared with non-smokers [16]. A study assessing smoking intensity and sleep quality using a self-reported questionnaire found that 36% of smokers had a Pittsburgh Sleep Quality Index (PSQI) score > 5 and were therefore classified as having poor sleep quality [17]. Furthermore, in a survey done on smokers, the authors found that sleep quality was poorer on those dependent on nicotine [18]. On the other hand, quitting smoking itself may induce transient insomnia [4]; future studies should assess the effect of nicotine dose on post-abstinence insomnia.
Several limitations should be considered upon interpreting the results and their associated data. Although several measures were adopted to minimize smoking outside study settings, it will not be eliminated, which might impose an unmeasured confounding effect [6]. Moreover, the duration of the current study from the beginning to the endpoint was only 6 weeks, so further longer duration studies should be considered. The lowest nicotine dose was 0.4 mg/g, where further studies should consider assessing nicotine-free cigarettes in the future. Finally, the use of the sleep disturbances item of the Minnesota Nicotine Withdrawal Scale will yield a sub-optimal outcome compared with a dedicated sleep quality scale that assesses sleep quality multidimensionally.
Most studies assessing the effect of cigarette smoking on sleep have focused on the subjective number of cigarettes smoked per day and its relation to sleep. Although the higher the number of cigarettes smoked usually denotes a higher nicotine dose, this conclusion needed to be examined independently. Using high-quality data from a randomized controlled study, we showed that higher nicotine concentration in cigarettes was associated with more sleep disturbances compared with lower nicotine doses.
Data availability
The data used in this study is available at the National Institute on Drug Abuse (NIDA) data share website: https://datashare.nida.nih.gov/study/nidacenicp1s1?fbclid=IwAR3ZLh85fSq9cQbTDmJNuihJh3HXaMXhW8qmxsCjZCpKOOlTcL-wYKtbyXw
References
Underner M, Paquereau J, Meurice J-C (2006) Cigarette smoking and sleep disturbance. Rev Mal Respir 23(3 Suppl):6S67–66S77
Salin-Pascual RJ, Moro-Lopez ML, Gonzalez-Sanchez H, Blanco-Centurion C (1999) Changes in sleep after acute and repeated administration of nicotine in the rat. Psychopharmacology 145(2):133–138. https://doi.org/10.1007/s002130051041
Abd Rashid N, Hapidin H, Abdullah H, Ismail Z, Long I (2017) Nicotine-prevented learning and memory impairment in REM sleep-deprived rat is modulated by DREAM protein in the hippocampus. Brain Behav 7(6):e00704. https://doi.org/10.1002/brb3.704
Costa M, Esteves M (2018) Cigarette smoking and sleep disturbance. Addict Disord Treat 17(1):40–48. https://doi.org/10.1097/ADT.0000000000000123
Jaehne A, Loessl B, Bárkai Z, Riemann D, Hornyak M (2009) Effects of nicotine on sleep during consumption, withdrawal and replacement therapy. Sleep Med Rev 13(5):363–377. https://doi.org/10.1016/j.smrv.2008.12.003
Donny EC, Denlinger RL, Tidey JW, Koopmeiners JS, Benowitz NL, Vandrey RG, al’Absi M, Carmella SG, Cinciripini PM, Dermody SS, Drobes DJ, Hecht SS, Jensen J, Lane T, le CT, McClernon FJ, Montoya ID, Murphy SE, Robinson JD, Stitzer ML, Strasser AA, Tindle H, Hatsukami DK (2015) Randomized trial of reduced-nicotine standards for cigarettes. N Engl J Med 373(14):1340–1349. https://doi.org/10.1056/NEJMsa1502403
Jesus SD, Hsin A, Faulkner G, Prapavessis H (2015) A systematic review and analysis of data reduction techniques for the CReSS smoking topography device. J Smok Cessat 10(1):12–28. https://doi.org/10.1017/jsc.2013.31
Radloff LS (1991) The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc 20(2):149–166. https://doi.org/10.1007/BF01537606
Watson D, Clark LA, Tellegen A (1988) Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol 54(6):1063–1070. https://doi.org/10.1037//0022-3514.54.6.1063
Hughes JR, Hatsukami D (1986) Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry 43(3):289–294. https://doi.org/10.1001/archpsyc.1986.01800030107013
Kim SS, Gulick EE, Kim S-H, Seo H-G (2007) Psychometric properties of the Minnesota Nicotine Withdrawal Scale: a Korean version. J Nurs Meas 15(2):121–132. https://doi.org/10.1891/106137407782156354
Mathews HL, Stitzel JA (2019) The effects of oral nicotine administration and abstinence on sleep in male C57BL/6 J mice. Psychopharmacology 236(4):1335–1347. https://doi.org/10.1007/s00213-018-5139-6
Zunhammer M, Eichhammer P, Busch V (2014) Sleep quality during exam stress: the role of alcohol, caffeine and nicotine. PLoS One 9(10):e109490. https://doi.org/10.1371/journal.pone.0109490
Aubin H-J, Luthringer R, Demazières A, Dupont C, Lagrue G (2006) Comparison of the effects of a 24-hour nicotine patch and a 16-hour nicotine patch on smoking urges and sleep. Nicotine Tob Res 8(2):193–201. https://doi.org/10.1080/14622200500489989
Gillin JC, Lardon M, Ruiz C, Golshan S, Salin-Pascual R (Aug. 1994) Dose-dependent effects of transdermal nicotine on early morning awakening and rapid eye movement sleep time in nonsmoking normal volunteers. J Clin Psychopharmacol 14(4):264–267
Liao Y et al (2019) Sleep quality in cigarette smokers and nonsmokers: findings from the general population in central China. BMC Public Health 19(1):808. https://doi.org/10.1186/s12889-019-6929-4
Dugas E, Sylvestre MP, O'Loughlin EK, Brunet J, Kakinami L, Constantin E, O'Loughlin J (Feb. 2017) Nicotine dependence and sleep quality in young adults. Addict Behav 65:154–160. https://doi.org/10.1016/j.addbeh.2016.10.020
Ogeil RP, Phillips JG (Aug. 2015) Commonly used stimulants: sleep problems, dependence and psychological distress. Drug Alcohol Depend 153:145–151. https://doi.org/10.1016/j.drugalcdep.2015.05.036
Acknowledgments
Not applicable.
Author information
Authors and Affiliations
Contributions
Study design: SAA. Research concept: SAA, AAT MA BA. Literature review: SK OEK IH AAT MA BA. Statistical analysis: SAA. Drafting: SK OEK IH AAT MA BA. Revision of manuscript: SAA. Approval of final manuscript: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflict of interest.
Ethics approval and consent to participate
Exempted as the study used open access data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
AlRyalat, S.A., Kussad, S., El Khatib, O. et al. Assessing the effect of nicotine dose in cigarette smoking on sleep quality. Sleep Breath 25, 1319–1324 (2021). https://doi.org/10.1007/s11325-020-02238-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-020-02238-3