Abstract
Purpose
Daytime sleepiness is associated with several medical problems. The aim of this paper is to provide normative values for one of the most often used questionnaires measuring daytime sleepiness, the Epworth Sleepiness Scale (ESS).
Methods
A large sample of 9711 people from the German general population took part in this study. In addition to the ESS, several other questionnaires were used, and sociodemographic and behavioral factors were recorded.
Results
Normative values for the ESS are given. According to the generally accepted criterion ESS > 10, 23 % of the sample showed excessive daytime sleepiness. Males reported significantly more daytime sleepiness than females (effect size d = 0.19). In the age range of 40–80 years, a continuous decline of daytime sleepiness was observed. Psychometric properties of the ESS were good. Alcohol intake and nicotine consumption were marginally associated with daytime sleepiness, and obese people reported significantly more sleepiness than people of normal weight (OR = 1.39).
Conclusions
The normative tables allow clinicians and researchers to assess the degree of their patients’ daytime sleepiness, especially in the upper range of scores.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Daytime sleepiness is defined as a difficulty in maintaining the alert awake state during the wakeful phase of the 24-h sleep-wake cycle [1]. It is associated with several medical problems [2] and mortality [3]. Diurnal sleepiness may be a consequence of poor sleep quality, especially insufficient sleep duration [4] and may lead to accidents [5, 6] and reduced cognitive performance [7]. It proved to be a risk factor for depression [8], cognitive dysfunction [9], and cardio-cerebrovascular diseases [10].
Several questionnaires have been developed for measuring sleepiness. The most often used method is the Epworth Sleepiness Scale (ESS), developed by Johns [11]. Multiple studies analyzed psychometric properties of the ESS, e.g., [12–14], for a summarizing review see [15]. A number of epidemiological studies have tested the ESS in large general population samples from several countries: Norway [16], the USA [17, 18], New Zealand [19], Korea [20], China [21], and Germany [22]. These studies provided reference data for clinical samples and tested the influence of sociodemographic and behavioral factors on sleepiness. Measured with this instrument and applying the criterion ESS > 10 for excessive daytime sleepiness (EDS), prevalence in the general population ranged between 10.8 % [17] and 22.2 % [21].
In some studies, males reported more daytime sleepiness than females [16, 19, 22], while other studies found either an inverted gender relationship or none at all [21, 23, 24]. Concerning age differences, one study reported increased sleepiness with increasing age [19], and one found decreased sleepiness [16], while yet other studies detected no linear age trends [21, 23, 24]. Socioeconomic status was also inconsistently related to sleepiness. The Korean study [23] found higher levels of sleepiness in groups with lower educational levels, but other studies failed to detect this relationship [17, 18, 21]. Obese people generally report experiencing more daytime sleepiness than people of normal weight [21, 25].
Daytime sleepiness is weakly associated with reduced quality of life [18, 21] and mental health problems [18, 20]. Though patients suffering from sleep disorders or symptoms such as sleep apnea, restless leg syndrome and snoring generally report higher levels of daytime sleepiness, the general association between daytime sleepiness and nocturnal sleep quality was found to be relatively weak with correlation coefficients between 0.11 [17] and 0.13 [18].
Most studies dealing with the ESS report mean values and standard deviations of the ESS. This helps clinicians decide whether a patient’s score is above or below this mean score. The generally used criterion of ESS > 10 for exaggerated daytime sleepiness is also helpful for such assessments. However, it is difficult to evaluate the degree of sleepiness at the upper end of the range of high scores because normative values are lacking. Furthermore, there is insufficient knowledge about the relationship between daytime sleepiness and behavioral factors.
The aims of this study were
-
1.
To test age and sex differences and to provide normative values for the ESS
-
2.
To test psychometric properties
-
3.
To examine the relationship between sociodemographic and behavioral factors and daytime sleepiness, based on a large German sample
Methods
Sample
The Leipzig Center for Civilization Diseases (LIFE) conducted a population-based study (LIFE-Adult-Study) with an age and gender stratified random sample of residents of the city of Leipzig, Germany. The main objective of that study was to investigate prevalences, genetic predispositions, early onset markers, and the role of lifestyle and mental health factors of major civilization diseases. The examination was conducted between August 2011 and November 2014. The sample with an age range of 18–80 years was obtained from the local residents’ registration office. Insufficient command of the German language and pregnancy was the exclusion criteria. According to the study protocol, the focus was on the age group 40–80 years; the 18–39-year age range was included but underrepresented. Letters of invitation were sent out by mail. At the study center, the participants underwent a set of assessment batteries, including several medical examinations, and the collection of information about their sociodemographics, medical history, and lifestyle factors. The participants received a lump sum of 20 EUR to compensate for their travel expenses. Further details of the study design are published elsewhere [26]. Informed consent was obtained from all participants. The study was approved by the ethics committee of the University of Leipzig.
Instruments
The Epworth Sleepiness scale (ESS) consists of eight items. The respondents are asked to use a four-point scale to rate their chances of falling asleep in eight different situations that people encounter in their daily lives. The ESS total score is the sum of the item scores (recoded from 0 to 3). This results in a scale range of 0 to 24. For this study, we used the German version of the ESS [27, 28].
In addition to the ESS, other questionnaires were administered to the study participants: the Pittsburgh Sleep Quality Index PSQI [] (subjective sleep quality), the Short Form Health Survey-8 SF-8 [29] (quality of life), and the Patient Health Questionnaire PHQ-15 [30] (physical complaints).
Statistical methods
The effects of age and gender on daytime sleepiness were statistically tested with a two-factorial ANOVA, using the factors age group (five categories) and gender (two categories). Post hoc comparisons between age groups were calculated with t tests, aggregating across males and females. Associations between the ESS scores and other scales were expressed in terms of Pearson correlations. Internal consistency was calculated with Cronbach’s α. The effects of education, occupational situation, alcohol consumption, tobacco smoking, body mass index, and sleep duration on daytime sleepiness were tested with logistic regression analyses, adjusted for age and gender. The analyses were performed separately for each factor with the Enter method. Effect sizes d for the comparison between subgroups were calculated according to Cohen, relating the mean score difference to the pooled standard deviation. The calculations were performed with SPSS version 20.
Results
Sample characteristics
The total sample of the study program comprised 10,000 people. Among all invited persons, 33 % did actively participate, 30 % declined to participate, and 37 % did not respond despite a reminder letter. Further details of the study sample are reported elsewhere [26]. Of the 10,000 people included in the study, 9771 filled in the ESS. The number of participants with complete ESS data was 9407. If only one ESS item was missing (304 participants), it was replaced with the rounded mean of the other seven items. This procedure resulted in a sample of 9711 people with valid data. Table 1 presents the sociodemographic characteristics of this sample. The mean age of the total sample was M = 56.7 years (SD = 12.4). On average, the males (M = 57.2, SD = 12.6) were slightly older than the females (M = 56.2, SD = 12.2).
ESS mean scores
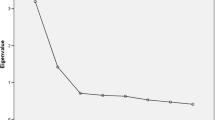
The ESS mean score of the total sample was M = 7.89 (SD = 3.67). The means are presented in Fig. 1 broken down by age and gender. Males reported generally more sleepiness than females, with the exception of the youngest age group. The effect size for the gender difference in the total sample was d = 0.19. In the age range of 40 to 80 years, sleepiness decreased continuously. Age and gender effects were statistically significant, the ANVOA results were as follows: age group, F = 89.3, p < 0.001; gender, F = 44.9, p < 0.001; and interaction age group × gender, F = 8.5, p < 0.001. Post hoc significance tests of the age decades (males and females combined) revealed that all ESS mean score differences among the age decades 40 to 80 years were statistically significant (p < 0.009) with the exception of the comparison of 60–69 and 70–80 years (p = 0.14).
Normative scores of the ESS are given in Table 2, separately for males and females. According to the criterion ESS > 10 for heightened scores, 2206 participants (22.7 % of the total sample) had excessive daytime sleepiness (see Table 2). A 24.2 % of the males and 20.1 % of the females had scores of 11 and above, while only 0.8 % of the total sample reported no daytime sleepiness at all (ESS = 0). The distribution of ESS scores deviated only slightly from normality: Skewness was 0.405 and kurtosis was 0.184.
Psychometric properties
The eight items of the ESS are described in Table 3. Two items (items 6 and 8) had very low mean scores (0.14 each), while the other mean scores were between 0.77 and 2.06. The most frequent situation for sleepiness is “lying down to rest in the afternoon when circumstances permit” (item 5). The internal consistency (Cronbach’s α) was 0.72 in this study. Each item contributed positively to the total score, and the corrected item-total correlations for the eight items were between 0.33 and 0.51.
Associations with other factors
Correlations between sleepiness (ESS) and the other scales were as follows: PSQI (sleep quality), r = 0.09; SF-8 Physical summary score, r = −0.10; SF-8 Mental summary score, r = −0.14; and PHQ-15 (physical complaints), r = 0.16. Among the dimensions of the PSQI, sleep duration seems to be most relevant for daytime sleepiness; the correlation between ESS and sleep duration was r = −0.13. All these correlation coefficients were statistically significant with p < 0.001. The mean scores of the PSQI and the PHQ-15 were as follows: PSQI, M = 5.0, SD = 3.4; and PHQ-15, M = 5.5; SD = 3.9.
Table 4 presents associations between daytime sleepiness and several sociodemographic and behavioral factors. While education had no significant influence on daytime sleepiness after controlling for age and gender, alcohol consumption and smoking were weakly associated with sleepiness. Retired people reported low degrees of sleepiness (OR = 0.53), and obesity was positively associated with sleepiness (OR = 1.39). Sleep duration as measured with the PSQI was divided into three categories: <6 h, 6–6.99 h, and ≥7 h (Table 4). Short sleep duration (<6 h) was strongly associated with daytime sleepiness (OR = 1.79), the effect size of the difference between normal sleepers and short sleepers was d = 0.30.
Discussion
The first aim of this study was to provide new normative values for the ESS. The mean score (M = 7.89) was higher than the means obtained in other general population studies, M = 6.95 in Norway [16], M = 6.11 in Korea [20], M = 6.75 in China [21], and M = 6.1 in the USA [18]. Cultural differences may play a role in the reporting of sleepiness (cf. [24]), and the low mean value of the American sample can be due to the high mean age of that sample. According to the ESS > 10 criterion, 23 % of our sample were characterized by excessive daytime sleepiness, while other studies found prevalence rates between 10.8 [17] and 22.2 % [21]. Our sample included people from the general population, and it was not restricted to healthy people. Samples that exclude people with sleep problems or illnesses are expected to obtain lower ESS mean scores. Two German examinations excluded such people and arrived at lower mean scores (M = 5.7 [31] and M = 6.6 [22]) compared with our general population study.
Males reported significantly more daytime sleepiness than females (effect size d = 0.19). Similar gender effects were also found in Norway [16], France [32], New Zealand [19], and Germany [22], while the examinations in Singapore [24] and China [21] failed to detect such differences. In Korea, the relationship was reversed, with higher scores for females. We observed a continuous decline in sleepiness in the age range 40 to 80 years. This was observed in Norway [16] as well but not in any of the other studies [18, 19, 21, 24]. Though the other studies of ESS in the general population [16–19, 21, 23, 24] had large sample sizes (n between 2000 and 6000), the differences between the results of these studies indicate that the generalizability of the findings is limited and that replication studies are essential.
It is an advantage that ESS > 10 is a generally accepted criterion for excessive daytime sleepiness because it makes the results of different studies comparable. However, there are no established cutoff scores for extreme sleepiness in the upper range of the scale. Table 2 shows normative scores that can be used to assess the degree of sleepiness in terms of percentiles. Because of the slight nonnormality of the distribution, such assessments are not possible when only mean scores and standard deviations are reported.
The correlations with the other questionnaires were in the expected direction but low in magnitude. The highest association was found for physical complaints (PHQ-15, r = 0.16). Quality of life was also associated with daytime sleepiness, and the coefficient of the mental component was slightly stronger (r = −0.14) than that of the physical component (r = −0.10). An even weaker relationship was found for sleep quality, though ESS is known to be associated with sleep apnea [33]. The PSQI total score correlated with the ESS with r = 0.09. This coefficient is even somewhat lower than the scores reported by the two large American studies (r = 0.11 [17] and r = 0.13 [18]). Obviously, daytime sleepiness and sleep quality are nearly independent variables, and bad sleep quality should not be considered a substantial factor evoking daytime sleepiness. Nevertheless, there was a significant relationship between sleep duration and daytime sleepiness. The effect size of the difference between short sleepers (<6 h) and sufficient sleepers (≥7 h) in daytime sleepiness was d = 0.30, which is more than the gender effect.
In the univariate analyses, high degrees of daytime sleepiness were found for respondents who had higher degrees of education and who were working full-time. However, all of these demographic variables depend on age. In the multivariate logistic regression analyses, only retirement remained as an independent factor for less daytime sleepiness. This may though be due to the fact that retired people are less restricted in their daily routine and that they can more easily choose rest periods when they are tired than full-time workers can.
The consumption of alcohol and nicotine also seemed to be associated with excessive daytime sleepiness in the univariate analyses. The effect sizes were similar to that of gender effect. After controlling for age and gender, the influence remained statistically significant, but the odds ratios were not high in magnitude (OR = 1.14 and 1.21, respectively). Similar results were obtained in a French study [32]. These findings underline that it is necessary to take age and gender into account when assessing associations. Obesity proved to be an independent risk factor for excessive daytime sleepiness in this study. As in the Chinese study [21], there were only small differences between normal weight (BMI < 25) and overweight (BMI < 30), but significant differences (OR = 1.39; CI = [1.22–1.58]) between normal weight and obesity (BMI ≥ 30).
Some limitations of this study should be mentioned. The low response rate (33 %) limits the generalizability of the results. Though there were no great differences between the participants and those who refused participation in terms of age and gender [26], we cannot conclude that there was no bias concerning sleepiness. Due to the cross-sectional character of this study, we cannot draw causal conclusions for the relationship between daytime sleepiness and associated factors such as tobacco consumption or obesity. Further limitations are the lack of information on shift work status and the problem that we cannot clearly distinguish between the factors age and retirement. The low level of sleepiness in the old age group and especially in the group of retired people may be a hint that the frames of reference can change over time. Elderly people generally experience higher degrees of physical complaints and fatigue. One reason for the high levels of sleepiness reported by full-time workers could be that they feel less tolerant of episodes of daytime sleepiness because these episodes hinder them in fulfilling their work obligations. Part-time workers or retired people however are not faced with bad consequences if they have a sleepy spell and are therefore less likely to perceive these as being problematic. Such problems can be solved when objective measures are used, but these are not applicable in large epidemiologic studies.
Conclusion
Age and gender differences have to be taken into account when sociodemographic or behavioral factors are analyzed as putative prognostic factors for daytime sleepiness. The normative scores provide a suitable data basis for the comparison between groups of patients differing in age and gender distributions.
References
American Academy of Sleep Medicine (2014) International classification of sleep disorders: diagnostic and coding manual, third edition (ICSD-3)
Ruggles K, Hausman N (2003) Evaluation of excessive daytime sleepiness. WMJ 102:21–24
Newman AB, Spiekerman CF, Enright P, Lefkowitz D, Manolio T, Reynolds CF, Robbins J (2000) Daytime sleepiness predicts mortality and cardiovascular disease in older adults. The Cardiovascular Health Study Research Group. J Am Geriatr Soc 48:115–123
Slater G, Steier J (2012) Excessive daytime sleepiness in sleep disorders. J Thorac Dis 4:608–616
Leger D, Bayon V, Ohayon MM, Philip P, Ement P, Metlaine A, Chennaoui M, Faraut B (2014) Insomnia and accidents: cross-sectional study (EQUINOX) on sleep-related home, work and car accidents in 5293 subjects with insomnia from 10 countries. J Sleep Res 23:143–152
Arita A (2015) Risk factors for automobile accidents caused by falling asleep while driving in obstructive sleep apnea syndrome. Sleep Breath 19:1229–1234
Curcio G, Ferrara M, De Gennaro L (2006) Sleep loss, learning capacity and academic performance. Sleep Med Rev 10:323–337
Jaussent I, Bouyer J, Ancelin ML, Akbaraly T, Peres K, Ritchie K, Besset A, Dauvilliers Y (2011) Insomnia and daytime sleepiness are risk factors for depressive symptoms in the elderly. Sleep 34:1103–1110
Jaussent I, Bouyer J, Ancelin ML, Berr C, Foubert-Samier A, Ritchie K, Ohayon MM, Besset A, Dauvilliers Y (2012) Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep 35:1201–1207
Jaussent I, Empana JP, Ancelin ML, Besset A, Helmer C, Tzourio C, Ritchie K, Bouyer J, Dauvilliers Y (2014) Insomnia, daytime sleepiness and cardio-cerebrovascular diseases in the elderly: a 6-year prospective study. Plos One 8, e56048
Johns MW (1991) A new method for measuring daytime sleepiness - the Epworth Sleepiness Scale. Sleep 14:540–545
Olaithe M, Skinner TC, Clarke J, Eastwood P, Bucks RS (2013) Can we get more from the Epworth Sleepiness Scale (ESS) than just a single score? Sleep Breath 17:763–769
Sargento P, Perea V, Ladera V, Lopes P, Oliveira J (2015) The Epworth Sleepiness Scale in Portuguese adults: from classical measurement theory to Rasch model analysis. Sleep Breath 19:693–701
Ulander M, Arestedt K, Svanborg E, Johansson P, Brostrom A (2013) The fairness of the Epworth Sleepiness Scale: two approaches to differential item functioning. Sleep Breath 17:157–165
Kendzerska TB, Smith PM, Brignardello-Petersen R, Leung RS, Tomlinson GA (2014) Evaluation of the measurement properties of the Epworth sleepiness scale: a systematic review. Sleep Med Rev 18:321–331
Pallesen S, Nordhus IH, Omvik S, Sivertsen B, Tell GS, Bjorvatn B (2007) Prevalence and risk factors of subjective sleepiness in the general adult population. Sleep 30:619–624
Beaudreau SA, Spira AP, Stewart A, Kezirian EJ, Lui LY, Ensrud K, Redline S, Ancoli-Israel S, Stone KL (2012) Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med 13:36–42
Spira AP, Beaudreau SA, Stone KL, Kezirian EJ, Lui LY, Redline S, Ancoli-Israel S, Ensrud K, Stewart A (2012) Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol Ser A-Biol Sci Med Sci 67:433–439
Gander PH, Marshall NS, Harris R, Reid P (2005) The Epworth Sleepiness Scale: influence of age, ethnicity, and socioeconomic deprivation. Epworth sleepiness scores of adults in New Zealand. Sleep 28:249–253
Joo SJ, Baik I, Yi H, Jung K, Kim J, Shin C (2009) Prevalence of excessive daytime sleepiness and associated factors in the adult population of Korea. Sleep Med 10:182–188
Wu S, Wang R, Ma X, Zhao Y, Yan X, He J (2012) Excessive daytime sleepiness assessed by the Epworth Sleepiness Scale and its association with health related quality of life: a population-based study in China. BMC Public Health 12:849
Joo S, Shin C, Kim J, Yi HY, Ahn Y, Park M, Kim J, Lee S (2005) Prevalence and correlates of excessive daytime sleepiness in high school students in Korea. Psychiatry Clin Neurosci 59:433–440
Sauter C, Popp R, Danker-Hopfe H, Büttner A, Wilhelm B, Binder R, Böhning W, Weess H-H (2007) Normative values of the German Epworth Sleepiness Scale. Somnologie 11:272–278
Ng TP, Tan WC (2005) Prevalence and determinants of excessive daytime sleepiness in an Asian multi-ethnic population. Sleep Med 6:523–529
Slater G, Pengo MF, Kosky C, Steier J (2013) Obesity as an independent predictor of subjective excessive daytime sleepiness. Respir Med 107:305–309
Loeffler M, Engel C, Ahnert P, Alfermann D, Arelin K, Baber R, Beutner F, Binder H et al (2015) The LIFE-Adult-Study: objectives and design of a population-based cohort study with 10,000 deeply phenotyped adults in Germany. BMC Public Health 15:691
Scalarum CIP (ed) (2005) Internationale Skalen für Psychiatrie, 5th edn. Beltz, Göttingen
Deutsche Gesellschaft für Schlafforschung und Schlafmedizin (DGSM) http://www.dgsm.de/fachinformationen_frageboegen_epworth.php?language=german Accessed 20 Apr 2016
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index—a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Ware JE, Kosinski M, Dewey JE, Gandek B (2001) How to score and interpret single-item health status measures: a manual for users of the SF-8TM Health Survey. Lincoln (RI), QualityMetric Incorporated
Kroenke K, Spitzer RL, Williams JBW (2002) The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 64:258–266
Bloch KE, Schoch OD, Zhang JNN, Russi EW (1999) German version of the Epworth Sleepiness Scale. Respiration 66:440–447
Tsuno N, Jaussent I, Dauvilliers Y, Touchon J, Ritchie K, Besset A (2007) Determinants of excessive daytime sleepiness in a French community-dwelling elderly population. J Sleep Res 16:364–371
Sauter C, Asenbaum S, Popovic R, Bauer H, Lamm C, Klosch G, Zeitlhofer J (2000) Excessive daytime sleepiness in patients suffering from different levels of obstructive sleep apnoea syndrome. J Sleep Res 9:293–301
Acknowledgments
This paper is supported by LIFE, Leipzig Research Centre for Civilization Diseases, an organizational unit affiliated to the Medical faculty of the University of Leipzig. LIFE is funded by means of the European Union, by the European Regional Development Fund (ERDF), and by funds of the Free State of Saxony within the excellence initiative (project numbers 713–241202, 14505/2470, 14575/2470).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the European Regional Development Fund (ERDF) and by funds of the Free State of Saxony within the excellence initiative (project numbers 713–241202, 14505/2470, 14575/2470). The sponsors had no role in the design or conduct of this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Sander, C., Hegerl, U., Wirkner, K. et al. Normative values of the Epworth Sleepiness Scale (ESS), derived from a large German sample. Sleep Breath 20, 1337–1345 (2016). https://doi.org/10.1007/s11325-016-1363-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1363-7