Abstract
Objective
The aim of this study was to evaluate the risk of obstructive sleep apnea (OSA) to preterm delivery (PTD), using the Berlin Questionnaire (BQ).
Methods
This was a large, prospective cohort study among pregnant Thai women. The BQ was employed for symptom-based OSA screening during the second trimester, and PTD was recorded in 1345 pregnant women. Multivariate models were applied in controlling for potential confounders.
Results
The overall prevalence of the high risk of OSA was 10.1 %, and it was significantly associated with pre-pregnancy body mass index and score on the Perceived Stress Scale. An adjusted odds ratio for PTD in women with a high risk of OSA was 2.00 (95 % confidence intervals (CIs) = 1.20, 3.34). Stratified analyses, after adjusting for confounding factors, indicated that a high risk of OSA was associated with an increased risk of spontaneous preterm delivery (odds ratio (OR) = 2.45, 95 % CI = 1.20, 5.02), but not with preterm premature rupture of membranes (OR = 1.61, 95 % CI = 0.61, 4.26), and medically indicated preterm delivery (OR = 1.83, 95 % CI = 0.72, 4.64).
Conclusion
Pregnant women with a high risk of OSA are at an increased risk of having PTD, compared with pregnant women with a low risk of OSA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Preterm delivery (PTD), defined by the World Health Organization as birth before the completion of 37 weeks of gestation, is the leading cause of perinatal mortality and long-term morbidity and is an important public health concern [1]. It has been estimated that 9.6 % of all births are preterm, accounting for 12.9 million babies per year worldwide. Approximately 85 % of this burden has been concentrated in Africa and Asia, where 10.9 million births have been preterm [2]. Many maternal risk factors have been associated with PTD, including maternal demographic characteristics, nutritional status, pregnancy history, present pregnancy characteristics, psychological characteristics, and adverse health behavior [3]. Preventing PTD remains one of the great challenges in modern obstetrics [4]; therefore, factors associated with preterm birth, but not obviously in the causal pathway, have been sought to explain PTD [4]. One area of increased investigation relates to obstructive sleep apnea (OSA).
OSA consists of decreased airflow due to repetitive complete or partial obstruction of the upper airway associated with progressive respiratory effort to overcome the obstruction. OSA is more common among pregnant women than non-pregnant women [5]. Several prior studies have provided information regarding the association between OSA and pregnancy outcomes [6–10]. Despite the potential adverse effects of OSA on maternal and fetal outcomes [11, 12], little research has been conducted in Asia (including Thailand) on the effects of OSA on pregnancy outcomes. OSA and its risk among pregnant Thai women, however, have not been widely evaluated, partly because of the lack of awareness of the impact of OSA in pregnancy and the limited availability of polysomnography (PSG).
Comparing data from those studies, differences should be noted among methodologies, definitions, and diagnostic criteria used. Many studies have used questionnaires to determine sleep apnea or its risk, whereas many have relied on overnight PSG studies, which are generally considered the gold standard diagnostic tool for evaluating OSA. Because PSG is expensive and time consuming, questionnaires have been developed to identify persons with OSA. However, the Berlin Questionnaire (BQ) is one screening tool widely used to identify patients with OSA, including pregnant women [13]. It is a useful and practical method of screening for OSA and can easily be incorporated into routine prenatal care. In addition to this, prior studies have suggested that the BQ has different predictive values, depending on the trimester of pregnancy when it is administered [14]. During the first trimester, the amount of sleep increases, coinciding with the subjective worsening of sleep quality. General sleep disturbance and fatigue are more common with advancing gestation, particularly during the third trimester [15–17], whereas during the second trimester, normal characteristics of sleep, such as sleep duration or sleep quality, prevail [18, 19]. Therefore, we sought to examine the independent effects of OSA screening by BQ during the second trimester of pregnancy on PTD among pregnant Thai women.
Methods
A prospective cohort study was conducted among women presenting to five prenatal care clinics affiliated with Maharat Nakhon Ratchasima Hospital, a large tertiary hospital in Nakhon Ratchasima Province, Thailand, between July 2013 and December 2014. Women in the second trimester of singleton pregnancy who initiated antenatal care prior to 20 weeks and planned to carry the pregnancy to term and to deliver at the study hospitals were recruited and followed up until delivery. Participants with asthma and chronic renal disease were excluded from the study. Because pregnancies complicated by chronic hypertension are at increased risk of several adverse pregnancy and perinatal outcomes, including PTD [20, 21], we also excluded participants with chronic hypertension. As this study examined pregnancy outcomes, enrolled subjects who had miscarriages or were lost on follow-up (delivery outcome unknown or medical record not found) were not included for outcomes analysis.
The plan was to enroll 1500 women. Assuming a 90 % completion rate, a 5 % PTD rate among the low-risk group for OSA, and a 10 % high risk for the OSA rate, 1350 women would complete the study, of whom approximately 135 would be PTD. With these sample size numbers for the current study, using an α error of 0.05 and a power of 0.80, the lowest detectable risk ratio was 2.3 for PTD, with a prevalence of 5 % in the low-risk group for OSA.
Data collection
This study was conducted by means of a self-administered, close-ended questionnaire distributed by research personnel at the five prenatal care clinics. Study participants, i.e., pregnant women between 14 and 27 weeks of gestation, were asked to complete a questionnaire that ascertained demographic information, including maternal age at the expected delivery date, marital status, and education level. Questions were also related to behavioral risk factors such as smoking and alcohol consumption. Consenting subjects were also administered a BQ to evaluate the risk of OSA in addition to the Perceived Stress Scale-10 (PSS-10) questionnaire to assess stress [22, 23]. Following delivery, participants’ medical records were reviewed by well-trained research personnel who used a standardized abstraction form. Information abstracted from medical records included a total amount of weight gain, gravidity, parity, number of previous abortions, gestational age at delivery, pregestational diabetes mellitus, and prior history of PTD.
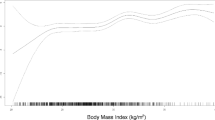
Pre-pregnancy body mass index (BMI) was calculated from maternal self-report of height and weight just prior to conception and cross-checked with documented BMI from the initial obstetric visit in the first trimester. Serial weights throughout the pregnancy were obtained from clinical visits, and following delivery, the total amount of weight gain was calculated.
Pre-pregnancy BMI categories were defined according to he World Health Organization: underweight <18.5, normal weight 18.5 to 24.9, overweight 25 to 29.9, and obese >30 kg/m2. BMI was calculated using height and weight data (kg/m2) [24].
Preterm delivery
The diagnosis of PTD was made using the American College of Obstetricians and Gynecologists (ACOG) guidelines [25]. Gestational age was based on the last menstrual period or ultrasound examination. Ultrasound-established dates should take preference over menstrual dates when the discrepancy is greater than 7 days during the first trimester or greater than 10–14 days during the second trimester [25, 26]. The ultrasonography was available for 96.4 % (54.3 % during the first trimester and 42.1 % during the second trimester) of all participants in this study. We also categorized PTD cases suggested from prior studies [3, 27, 28], by etiologic heterogeneity as well as heterogeneity in its underlying clinical presentations: spontaneous onset of labor, preterm premature rupture of membranes, and medically indicated PTD.
The Berlin Questionnaire
The BQ, developed in 1996 [13], includes a series of questions about risk factors for sleep apnea, including snoring behavior, wake-time sleepiness, or fatigue, and obesity or hypertension. The BQ contains five questions concerning snoring, three questions addressing daytime sleepiness, and one question concerning obesity or history of high blood pressure. Predetermination of high risk and lower risk for sleep apnea was based on responses in three symptom categories. In category 1, in two or more questions about participants’ snoring, high risk was defined as persistent symptoms (more than three to four times per week). In category 2, high risk was defined as persistent (more than three to four times per week) wake-time sleepiness, drowsy driving, or both. In category 3, high risk was defined as a history of high blood pressure and/or a BMI of more than 30 kg/m2. Because we excluded all participants with known chronic hypertension at the time of screening, a positive response in category 3 was based on the presence of a BMI of more than 30 kg/m2. As per the questionnaire guidelines, for a person to be considered at high risk of OSA, she had to qualify as high risk for at least two symptom categories. Those with symptoms in at least two categories which were not persistent or those who were qualified in only one symptom category were considered to be at low risk of OSA [13].
Statistical analysis
All data were analyzed with Stata software, version 11.0 (Stata Corp., College Station, TX, USA). Histograms, boxplots, and descriptive methods were used to examine data for errors, outliers, and missing values. Between-group comparisons of continuous variables (perceived stress score and total amount of weight gain) were conducted with t tests (low risk of OSA vs. high risk of OSA). Dichotomized variables were compared with Fisher’s exact test. Logistic regression was used to determine associations between the risk of OSA and PTD after adjusting for potential covariates, where appropriate. We considered the following covariates as possible confounders: maternal age, marital status, maternal educational attainment, pre-pregnancy BMI, alcohol consumption, smoking status during pregnancy, parity, previous abortion, pregestational diabetes mellitus, prior history of PTD, and score on PSS. Confounders were defined as those factors that altered unadjusted odds ratios by at least 10 %. Statistical hypotheses were tested using two-tailed odds ratios (OR), 95 % confidence intervals (CIs), and p < 0.05 was considered statistically significant.
Results
During the study period, 1568 eligible women were approached and 1500 (95.7 %) agreed to participate. One hundred and fifty-three women who were lost to follow-up (delivery outcome unknown or medical records not found) were excluded from this analysis. Also excluded were women who experienced an abortion or fetal demise prior to 28 weeks of gestation (n = 2). A cohort of 1345 women remained for analysis.
Of the 1345 respondents who completed screening questionnaires for symptoms of OSA at a mean gestational age of 18.1 (SD 3.29) weeks, 10.1 % (n = 136) met the criteria for a high risk of OSA, while the remainder of the participants were classified as low risk. Table 1 provides the maternal sociodemographic factors stratified by the risk group for OSA. Overall, women at high or low risk of OSA were similar with regard to maternal age, educational attainment, marital status, smoking, and alcohol consumption status. As seen in Table 2, no clinically meaningful differences were observed between women at high risk and low risk of OSA with regard to parity, prior history of PTD, previous abortion, pregestational diabetes mellitus, and total gestational weight gain. The women in the high-risk group for OSA, however, were more likely to be overweight or obese pre-pregnancy and were reported to be more likely to have an average score on PSS than the low-risk group was.
As seen in Table 3, women in the group at high risk of OSA were at higher risk of PTD than those in the group at low risk (unadjusted OR = 2.10, 95 % CI = 1.32, 3.36). Adjustment for possible confounding by maternal age, pre-pregnancy BMI, parity, smoking during pregnancy, previous preterm delivery, and number of previous abortions did not result in a material difference in the association (adjusted OR = 2.00, 95 % CI = 1.20, 3.34).
Additionally, analyses were also performed stratified by the PTD subtype described previously (i.e., spontaneous preterm delivery, preterm premature rupture of membranes, and medically indicated preterm delivery). As seen in Table 4, the risk of OSA was associated with an increased risk of spontaneous preterm delivery after adjusting for potential confounders (OR = 2.45, 95 % CI = 1.20, 5.02). For preterm premature rupture of membranes or medically indicated preterm delivery, there was no clear evidence of a positive association with the risk group for OSA. The high-risk group for OSA was associated with an increased risk of preterm premature rupture of membranes (OR = 1.61, 95 % CI = 0.61, 4.26) and medically induced preterm delivery (OR = 1.83, 95 % CI = 0.72, 4.64), though these latter associations were not statistically significant.
Discussion
To the best of our knowledge, this is the first prospective cohort study comparing PTD between high risk and low risk of OSA among pregnant Thai women. In this study, using both adjusted and unadjusted analyses, we found that screening positive for OSA on BQ was associated with PTD. Also notable was the risk of spontaneous preterm delivery among those screening positive on the BQ, demonstrating that the risk of spontaneous preterm delivery increases with screening positive on BQ.
Our findings confirm those of prior studies [10, 12]. For example, Louis et al. reported that women with OSA were more likely to have PTD than obese controls and normal-weight controls (30 % vs. 10 % and 12 %, respectively; p < 0.01) [10]. Another study by Chen et al. also found that after adjusting for mother’s education, marital status, gestational diabetes mellitus, gestational hypertension, anemia, coronary heart disease, hyperlipidemia, obesity, geographic region, paternal age, infant’s sex, and parity, pregnant women with OSA were at an increased risk of preterm delivery 2.31 (95 % CI = 1.77, 3.01) [12]. Moreover, our findings are similar to those that used more invasive, though objective, measures of sleep traits (e.g., polysomnography) [10].
The association between OSA and PTD has biological plausibility. For example, some research suggests that inflammatory cytokines may play a major role in the initiation of PTD [29–32]. The meta-analysis study has identified that levels of systemic inflammatory markers were found to be higher in OSA patients than in the control subjects [33]. The associations between OSA and increased inflammatory cytokine concentrations and between inflammatory cytokines and PTD demonstrate a plausible mechanism for the observed associations. However, no prior research has directly examined the relationship between OSA, levels of pro-inflammatory markers, and risk of PTD. More research is needed to enhance our understanding of the effect of OSA on PTD and the physiological mechanisms underlying this relationship.
When interpreting our data, there are several points to consider. First, the screening of participants by BQ in this study had no confirmation with the PSG. However, the BQ is widely used in pregnancy [14, 34–36], and a prior study confirms that the predictive values are acceptable, particularly in the second trimester [34]. Second, although we adjusted for many potential confounders, we cannot exclude the possibility that some residual confounding factors not measured in our study (e.g., urinary tract infection, bacterial vaginosis, chorioamnionitis, and pre-existing OSA) may have influenced the reported risk estimates.
Despite the abovementioned limitations, our large datasets, examined for integrity and validity as described in the previous text, provided sufficient statistical power to detect differences. The prospective study design and very high successful follow-up rate (89.7 %) of the enrolled subjects and the fact that less than 5 % of the cases in this study had missing values represent important strengths in our study. We also compared the baseline characteristics of enrollees lost to follow-up to those who completed the study and noted that all the variables were comparable, suggesting that the few women lost to follow-up would not have affected the outcomes disproportionately. We worked toward identifying the etiologically homogenous grouping of PTD by a subgroup analysis of spontaneous preterm delivery, preterm premature rupture of membranes, and medically indicated preterm delivery. This study also suggests that the BQ, administered in the second trimester of pregnancy, may be capable of screening for OSA, as the potential for earlier screening tools will hopefully allow earlier detection of OSA and more time for effective intervention and potentially improved pregnancy outcomes including PTD.
Conclusion
The results of this study indicate that pregnant women with a high risk of OSA detected by BQ had a high risk of PTD. Our result, given the local relevance of OSA, suggests that it is important to increase awareness not only among pregnant women but also, more importantly, among physicians. OSA symptoms should be assessed in all pregnant women. Early diagnosis and management may decrease the adverse outcomes associated with OSA during pregnancy. Close monitoring of pregnant women with a high risk of OSA is essential. Moreover, our study illustrates the need for further studies to assess the mechanisms for the association between OSA and PTD.
References
Behrman RE, Butler AS (Eds). (2007) In: Preterm birth: causes, consequences, and prevention. The National Academies Collection: reports funded by National Institutes of Health. Washington (DC).
Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, Rubens C, Menon R, Van Look PF (2010) The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ 88(1):31–38. doi:10.2471/BLT.08.062554
Ip M, Peyman E, Lohsoonthorn V, Williams MA (2010) A case-control study of preterm delivery risk factors according to clinical subtypes and severity. J Obstet Gynaecol Res 36(1):34–44. doi:10.1111/j.1447-0756.2009.01087.x
Iams JD, Romero R, Culhane JF, Goldenberg RL (2008) Primary, secondary, and tertiary interventions to reduce the morbidity and mortality of preterm birth. Lancet 371(9607):164–175. doi:10.1016/S0140-6736(08)60108-7
Sahota PK, Jain SS, Dhand R (2003) Sleep disorders in pregnancy. Curr Opin Pulm Med 9(6):477–483
Champagne K, Schwartzman K, Opatrny L, Barriga P, Morin L, Mallozzi A, Benjamin A, Kimoff RJ (2009) Obstructive sleep apnoea and its association with gestational hypertension. Eur Respir J 33(3):559–565. doi:10.1183/09031936.00122607
Sahin FK, Koken G, Cosar E, Saylan F, Fidan F, Yilmazer M, Unlu M (2008) Obstructive sleep apnea in pregnancy and fetal outcome. Int J Gynaecol Obstet 100(2):141–146. doi:10.1016/j.ijgo.2007.08.012
Ayrim A, Keskin EA, Ozol D, Onaran Y, Yiidirim Z, Kafali H (2011) Influence of self-reported snoring and witnessed sleep apnea on gestational hypertension and fetal outcome in pregnancy. Arch Gynecol Obstet 283(2):195–199. doi:10.1007/s00404-009-1327-2
Ko H, Kim M, Kim Y, Lee J, Park Y-G, Moon H, Kil K, Lee G, Kim S, Shin J (2012) Obstructive sleep apnea screening and perinatal outcomes in Korean pregnant women. Arch Gynecol Obstet:1–5. doi:10.1007/s00404-012-2602-1
Louis JM, Auckley D, Sokol RJ, Mercer BM (2010) Maternal and neonatal morbidities associated with obstructive sleep apnea complicating pregnancy. Am J Obstet Gynecol 202(3):261 . doi:10.1016/j.ajog.2009.10.867e261–265
Louis JM, Mogos MF, Salemi JL, Redline S, Salihu HM (2014) Obstructive sleep apnea and severe maternal-infant morbidity/mortality in the United States, 1998-2009. Sleep 37(5):843–849. doi:10.5665/sleep.3644
Chen YH, Kang JH, Lin CC, Wang IT, Keller JJ, Lin HC (2012) Obstructive sleep apnea and the risk of adverse pregnancy outcomes. Am J Obstet Gynecol 206(2):136 . doi:10.1016/j.ajog.2011.09.006e131–135
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP (1999) Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131(7):485–491
Tantrakul V, Sirijanchune P, Panburana P, Pengjam J, Suwansathit W, Boonsarngsuk V, Guilleminault C (2015) Screening of obstructive sleep apnea during pregnancy: differences in predictive values of questionnaires across trimesters. J Clin Sleep Med JCSM: Off Publ Am Acad Sleep Med 11(2):157–163. doi:10.5664/jcsm.4464
Wilson DL, Barnes M, Ellett L, Permezel M, Jackson M, Crowe SF (2011) Decreased sleep efficiency, increased wake after sleep onset and increased cortical arousals in late pregnancy. Aust N Z J Obstet Gynaecol 51(1):38–46. doi:10.1111/j.1479-828X.2010.01252.x
Facco FL, Kramer J, Ho KH, Zee PC, Grobman WA (2010) Sleep disturbances in pregnancy. Obstet Gynecol 115(1):77–83. doi:10.1097/AOG.0b013e3181c4f8ec
Parry BL, Martinez LF, Maurer EL, Lopez AM, Sorenson D, Meliska CJ (2006) Sleep, rhythms and women’s mood. Part I. Menstrual cycle, pregnancy and postpartum. Sleep Med Rev 10(2):129–144. doi:10.1016/j.smrv.2005.09.003
Hedman C, Pohjasvaara T, Tolonen U, Suhonen-Malm AS, Myllyla VV (2002) Effects of pregnancy on mothers’ sleep. Sleep Med 3(1):37–42
Lee KA, Zaffke ME, McEnany G (2000) Parity and sleep patterns during and after pregnancy. Obstet Gynecol 95(1):14–18
Sibai BM, Koch MA, Freire S, Pinto e Silva JL, Rudge MV, Martins-Costa S, Moore J, Santos Cde B, JG C, Costa R, JG R, Moss N, Spinnato JA 2nd (2011) The impact of prior preeclampsia on the risk of superimposed preeclampsia and other adverse pregnancy outcomes in patients with chronic hypertension. Am J Obstet Gynecol 204(4):345 . doi:10.1016/j.ajog.2010.11.027e341–346
Chappell LC, Enye S, Seed P, Briley AL, Poston L, Shennan AH (2008) Adverse perinatal outcomes and risk factors for preeclampsia in women with chronic hypertension: a prospective study. Hypertension 51(4):1002–1009. doi:10.1161/HYPERTENSIONAHA.107.107565
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24(4):385–396
Wongpakaran N, Wongpakaran T (2010) The Thai version of the PSS-10: an investigation of its psychometric properties. Biopsychosoc Med 4:6. doi:10.1186/1751-0759-4-6
(2009). In: Rasmussen KM, Yaktine AL (eds) Weight gain during pregnancy: reexamining the guidelines. The National Academies Collection: Reports funded by National Institutes of Health. Washington (DC)
ACOG Practice Bulletin (2001) Assessment of risk factors for preterm birth. Clinical management guidelines for obstetrician-gynecologists. Number 31, October 2001. (Replaces Technical Bulletin number 206, June 1995; Committee Opinion number 172, May 1996; Committee Opinion number 187, September 1997; Committee Opinion number 198, February 1998; and Committee Opinion number 251, January 2001). Obstet Gynecol 98(4):709–716
Berghella V (2012) Obstetric evidence based guidelines. Series in maternal-fetal medicine, 2nd edn. Informa Healthcare, New York
Savitz DA, Blackmore CA, Thorp JM (1991) Epidemiologic characteristics of preterm delivery: etiologic heterogeneity. Am J Obstet Gynecol 164(2):467–471
Ananth CV, Vintzileos AM (2006) Epidemiology of preterm birth and its clinical subtypes. J Matern Fetal Neonatal Med 19(12):773–782. doi:10.1080/14767050600965882
Gargano JW, Holzman C, Senagore P, Thorsen P, Skogstrand K, Hougaard DM, Rahbar MH, Chung H (2008) Mid-pregnancy circulating cytokine levels, histologic chorioamnionitis and spontaneous preterm birth. J Reprod Immunol 79(1):100–110. doi:10.1016/j.jri.2008.08.006
Simhan HN, Krohn MA (2009) First-trimester cervical inflammatory milieu and subsequent early preterm birth. Am J Obstet Gynecol 200(4):377 . doi:10.1016/j.ajog.2008.10.038e371–374
Chang JJ, Pien GW, Duntley SP, Macones GA (2010) Sleep deprivation during pregnancy and maternal and fetal outcomes: is there a relationship? Sleep Med Rev 14(2):107–114. doi:10.1016/j.smrv.2009.05.001
Taylor BD, Holzman CB, Fichorova RN, Tian Y, Jones NM, Fu W, Senagore PK (2013) Inflammation biomarkers in vaginal fluid and preterm delivery. Hum Reprod 28(4):942–952. doi:10.1093/humrep/det019
Nadeem R, Molnar J, Madbouly EM, Nida M, Aggarwal S, Sajid H, Naseem J, Loomba R (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med 9(10):1003–1012. doi:10.5664/jcsm.3070
Wilson DL, Walker SP, Fung AM, O’Donoghue F, Barnes M, Howard M (2013) Can we predict sleep-disordered breathing in pregnancy? The clinical utility of symptoms. J Sleep Res 22(6):670–678. doi:10.1111/jsr.12063
Olivarez SA, Ferres M, Antony K, Mattewal A, Maheshwari B, Sangi-Haghpeykar H, Aagaard-Tillery K (2011) Obstructive sleep apnea screening in pregnancy, perinatal outcomes, and impact of maternal obesity. Am J Perinatol 28(8):651–658. doi:10.1055/s-0031-1276740
Mindell JA, Cook RA, Nikolovski J (2015) Sleep patterns and sleep disturbances across pregnancy. Sleep Med 16(4):483–488. doi:10.1016/j.sleep.2014.12.006
Acknowledgments
The authors would like to thank all the staff of the Research Center of Maharat Nakhon Ratchasima Hospital for their assistance in data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Funding
This study was supported by grants from the 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund) and Ratchadaphiseksomphot Fund (RA 57/001), Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand. The funders had no role in the design or conduct of this research.
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Na-rungsri, K., Lertmaharit, S., Lohsoonthorn, V. et al. Obstructive sleep apnea and the risk of preterm delivery. Sleep Breath 20, 1111–1117 (2016). https://doi.org/10.1007/s11325-016-1339-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1339-7