Abstract
Objective
Obstructive sleep apnea (OSA) and obesity are increasingly prevalent worldwide. Both promote endothelial dysfunction contributing to systemic and pulmonary hypertension over time. Endothelin-1 (ET-1) plays a pivotal role in the development of pulmonary hypertension (PH). The aim of the present study was to assess the association between plasma ET-1 and echocardiographic findings in obese individuals with and without OSA, as well as in non-obese patients with OSA.
Methods
Ninety-seven subjects (56 males) were enrolled in the study. All subjects underwent the following tests: venous endothelin-1 levels, pulmonary function testing, and arterial blood gas analysis. All patients except controls underwent transthoracic echocardiography and portable testing for sleep-disordered breathing.
Results
Plasma ET-1 levels were significantly higher in obese patients, both with and without OSA (respectively, n = 30 (mean value, 268.06 ± 49.56 pg/ml) and n = 32 (mean value, 263.12 ± 65.26 pg/ml)), compared with non-obese patients with OSA or to healthy controls (respectively, n = 20 (mean value, 149.8 ± 23.09 pg/ml) and n = 15 (mean value, 152.3 ± 27.64 pg/ml); p < 0.0001). Pulmonary artery pressure (PAPs) in obese patients with OSA were significantly higher than in obese patients without OSA (p < 0.0001), while there was no statistical difference between PAPs of obese patients without OSA, compared with the group of non-obese OSA patients. Plasma ET-1 levels significantly correlated with systolic PAPs in obese patients both with and without OSA (respectively, n = 30, r = 0.385, p = 0.03567; n = 32, r = 0.3497, p = 0.0497).
Conclusions
Our study suggests that endothelin levels are more strongly associated with weight than the presence of sleep-disordered breathing, but pulmonary artery hypertension is associated with both weight and OSA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is increasing in prevalence globally, in large part due to the increasing prevalence of overweight and obesity, which are common hallmarks of the disorder [1]. OSA is accompanied by local and systemic inflammation [2, 3]. Indeed, there is evidence that oxidative stress [2] as well as circulating inflammatory factors [3] are elevated in OSA patients. In addition, recent studies have demonstrated a strongly positive correlation between C-reactive protein and severity of OSA [4]. Increased inflammation in OSA is likely due to the activation of nuclear factor-κB by increased circulating adipokines and free fatty acids and/or by stress hypoxia. The release of adipokines and free fatty acids by excess adipose tissue links obesity, OSA, and the metabolic syndrome, both individually and synergistically [5]. In addition, intermittent hypoxia plays an important role not only by stimulating the release of pro-inflammatory cytokines, thus accelerating the course of the disease [6], but also by contributing to hypoxic vasoconstriction by the release of several vascular mediators. One such mediator is endothelin-1 (ET-1) [7], which actively participates in the development of endothelial dysfunction with irreversible vascular remodeling and effects on the systemic and pulmonary circulations [8, 9]. It has been recently documented that pulmonary hypertension (PH) affects 20 to 40 % of those with OSA, in the absence of other known cardiopulmonary disorders, and that these disorders have important interacting clinical effects in patients affected [10].
The prevalence of obesity is increasing globally, now affecting 10 to 25 % of the world population. Obesity is associated with a wide range of pathophysiological alterations, including elevated systemic and pulmonary artery pressures [11] and is sustained by systemic inflammation [12]. Further, obesity is characterized by increased production and secretion of a wide range of inflammatory molecules, including TNF-alpha and interleukin-6, which have both local effects on adipose tissue physiology and systemic effects on other organs [12, 13]. Among a wide spectrum of pro-inflammatory and growth factor mediators, Endothelin-1 plays a crucial role in obese individuals, not only by contributing to the link between obesity, inflammation and endothelial dysfunction [14], but also by actively participating in vascular remodeling with subsequent pulmonary hypertension. Plasma ET-1 concentrations are increased in human obesity, independent of the arterial pressure [15]. These findings aside, there is limited data on the prevalence of PH in obese people. A retrospective single center study reported that 5 % of otherwise healthy individuals with a body mass index (BMI) >30 kg/m2 had moderate or severe pulmonary hypertension (estimated pulmonary artery systolic pressure (PAPs) greater than 50 mm/Hg on echocardiogram) [16]. Although measurable changes in the structure and function of the right ventricle have been reported in association with OSA and obesity [17], the clinical significance of these changes is uncertain.
The aim of the present study was to assess the association between plasma levels of endothelin-1 and echocardiographic findings of PH in obese patients with and without OSA, as well as in OSA patients with normal BMI.
Methods
Patient population
Ninety-seven subjects (56 males) being followed in the outpatient clinic of Institutes of Pulmonary Disease and Cardiovascular Disease, University of Bari, and in the outpatient clinic of Santa Maria della Pietà, from March 2011 to July 2014, were enrolled into the study. Thirty-two (14 males) obese subjects without OSA were included in group 1, 30 obese individuals (19 males) with polysomnographic signs of OSA were enrolled in group 2, 20 OSA patients (15 males) with normal BMI comprised group 3, and 15 healthy subjects (8 males) with normal BMIs participated as the control group. Patients with respiratory, cardiovascular, or other organ failure, cancer, or inability to cooperate were excluded from the study. At the time of inclusion into the study, all the patients were non-smokers or ex-smokers, in stable condition, and free from respiratory tract infections. No patients were receiving steroids. No change in medical therapy was made in the week prior to the study. The study was approved by the Institutional Review Board of Bari University General Hospital and carried out in accordance with the principles of the Helsinki Declaration. All patients gave prior written informed consent to take part in the study. The IRB approval number was ST 3389, 15 Aug 2009.
All subjects underwent the following tests: venous endothelin-1 levels, pulmonary function testing, and arterial blood gas analysis. All patients except controls underwent transthoracic echocardiography and polysomnographic evaluation for sleep-disordered breathing. The anthropometric characteristics of the patients recruited are shown in Table 1.
Measurement of ET-1
Peripheral venous blood samples were obtained in all subjects from an antecubital vein after at least 30 min, seated at rest. Venous blood samples were collected in plastic tubes containing EDTA centrifuged at 5000×g for 10 min, and plasma was frozen and stored at −80 °C until assay. A specific enzyme immunoassay (EIA) kit (Cayman Chemical, Ann Arbor, Michigan, USA) was used to measure ET-1 concentrations in the blood samples. The evaluation was conducted at Clinic of Internal Medicine, University of Bari.
Pulmonary function testing and arterial blood gas analysis
Pulmonary function tests were performed in the pulmonary function laboratory of our Institutes using a spirometer (PK Morgan Ltd; Gillingham, UK). The equipment was calibrated daily using a 3-l syringe, and the analysis was performed in accordance to the guidelines of the American Thoracic Society [18]. The best of three reproducible values was expressed as a percentage of the predicted normal value.
Echo-Doppler assessment
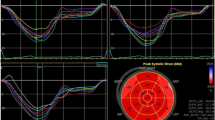
All patients except controls were investigated using real-time, phased array, two-dimensional Doppler (2-D) echocardiography (CFM 750 CV 2.5 or 3.25 MHz transducer; GE Vingmed, Milan, Italy). The examinations were performed at the Division of Cardiovascular Disease, University of Bari, with the patients in the semi-recumbent left lateral position, and images were taken from sub-xiphoid, parasternal, and apical views. The mean value of three measurements was included in analysis. Tricuspid valve regurgitation pressure was identified by color flow mapping, then maximal pressure gradient between right ventricular and right atrial was obtained using continuous wave Doppler on the guidance of the color Doppler signal of the tricuspid regurgitation. Peak pressure gradient measurement was estimated by means of a simplified Bernoulli equation [19]. PAP was calculated by adding the Bernoulli derived pressure gradient to an assumed right atrial pressure of 10 mmHg. Tricuspid annular plane systolic excursion (TAPSE) was measured from the tricuspid lateral annulus. A TAPSE <16 mm indicates right ventricular systolic dysfunction.
Sleep study
All patients in groups 1, 2, and 3 were evaluated in the sleep laboratory of the Institutes of Respiratory Diseases of the University of Bari for one night. They were monitored continuously for about 8 h using a portable cardiorespiratory monitoring (POLYMESAM®, MAP, Martinsried, Germany). The POLYMESAM® (PM) device consists of a recorder, to which multiple sensors are linked for the detection of the following signals: oxy-hemoglobin saturation (by a finger sensor), heart rate (derived from three electrocardiogram (ECG) electrodes placed on the chest), snoring sound (by a microphone placed on the thyroid cartilage), body posture, oro-nasal airflow (by a threefold thermocouple sensor for both nostrils and mouth), and thoracic and abdominal movements (by stretch belts). Apnea was identified if the airflow was absent or nearly absent for at least 10 s. Hypopnea was defined as at least a 30 % reduction in airflow or thoraco-abdominal movement below baseline values for at least 10 s, accompanied by a decrease in oxyhemoglobin saturation of ≥4 %. Table 1 shows the polysomnographic analysis of the groups 1, 2, and 3.
Statistical analysis
Distributions were defined by the Kolmogorov-Smirnov test. As all data were parametrically distributed, they are expressed as mean ± SD. Comparisons between continuous variables were obtained with ANOVA and Student’s t test for unpaired data. The Pearson’s correlation coefficient was used to analyze correlations between variables. The level of significance was set at p < 0.05 in all analyses. Statistical analyses were performed using GraphPAD Prism, version 4 (GraphPAD Inc, San Diego, CA, USA).
Results
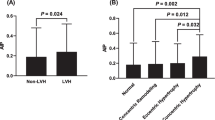
Demographic and clinical characteristics of 97 subjects are presented in Table 1. Endothelin-1 was detectable in the blood of all subjects. Plasma ET-1 levels were significantly higher in obese patients, both with or without OSA (respectively, n = 30 (268.06 ± 49.56 pg/ml) and n = 32 (263.12 ± 65.26 pg/ml)), as compared with patients with OSA with a normal BMI, or to healthy controls (respectively, 149.8 ± 23.09 pg/ml and 152.3 ± 27.64 pg/ml; (p < 0.0001) (Fig. 1).
Endothelin-1 (pg/ml) concentration in the venous blood of the four groups: Obese without OSA [32], obese with OSA [30], OSA without obesity [20], and healthy subjects (HS) [15]. Significance was established at a p value <0.05. The horizontal lines represent median value. ET-1 in venous sample was increased in all obese patients as compared with OSA non obese (p < 0.0001) and to control group (p < 0.0001)
PAPs in obese patients with OSA were significantly higher than in obese patients without OSA (p < 0.0001), while there was no statistical difference between PAPs of obese patients without OSA, compared with the group of non-obese OSA patients (p = 0.07) (Table 1).
There was a significant positive correlation between plasma ET-1 levels and PAPs in obese patients with or without OSA (respectively, n = 30, r = 0.385, p = 0.03567; n = 32, r = 0.3497, p = 0.0497) (Fig. 2). No such relationship existed in OSA patients with normal BMI (n = 20, r = −0.11, p = 0.5) (Fig. 2).
Significant positive correlation between plasma ET-1 levels and systolic pulmonary artery pressure (PAPs) in obese patients with OSA (n = 30, r = 0.385, p = 0.03567). Significant positive relationship between plasma ET-1 levels and PAPs in obese patients without OSA (n = 32, r = 0.3497, p = 0.0497). No significant relationship between plasma ET-1 levels and PAPs in OSA patients without signs of obesity (n = 20, r = −0.11, p = 0.5)
TAPSE in obese patients with OSA was significantly lower than in obese patients without OSA (p < 0.001), while there was no statistical difference between TAPSE of obese patients without OSA and TAPSE of non-obese OSA patients (p = 0.25) (Table 1).
A significant positive correlation was found between plasma ET-1 levels and PAPs in all patients (n = 97, r = 0.39, p = 0.0003) (Fig. 3), while a statistical negative correlation was observed between plasma ET-1 levels and TAPSE in all patients (n = 97, r = −0.34, p = 0.002) (Fig. 4).
Discussion
The present study demonstrated increased plasma ET-1 levels in obese patients with or without OSA, as compared with patients affected by OSA with a normal BMI. Indeed, ET-1 levels in non-obese patients with OSA were not significantly elevated and were very similar to those observed in normal subjects. In addition, there was a positive correlation between PAPs and ET-1 levels in all obese subjects (62) but an inversely significant relationship between echocardiographic TAPSE values and plasma ET-1 levels in the entire study group. On the other hand, PAPs were higher in obese patients with OSA than in obese patients without OSA, suggesting that the effects of OSA and obesity on PH are additive.
Obstructive sleep apnea and obesity are both recognized as important risk factors for PH. More than 20 years ago, the prevalence of OSA was reported to be 40 % of obese men with PH [22]. OSA has been formally recognized as a cause of PH since 2009, and classified in the third group of the recent classification [23]. The pathogenic mechanisms leading to PH in OSA include by repetitive nocturnal hypoxemia, diurnal hypercapnia, blood acidosis, and increased sympathetic tone, which induce pulmonary artery hypoxic vasoconstriction with subsequent pulmonary arteriolar remodeling. In isolation, OSA typically causes only mild PH, which generally does not require treatment [24]. However, OSA patients often present with more severe degrees of PH when they have comorbid conditions contributing to hypoxemia, such as obesity hypoventilation syndrome (OHS) [25]. In addition, cardiomyopathy characterized by eccentric ventricular hypertrophy and diastolic heart failure is a well-recognized condition in severely obese patients [26]. The chronically elevated left ventricular filling pressure is transmitted into the pulmonary venous system, leading to elevated pulmonary venous pressures, arteriolar remodeling, and ultimately to persistent elevated pulmonary vascular resistance [27]. The interplay between OSA, insulin resistance [28], and elevated left ventricular filling is likely responsible for endothelial dysfunction, with consequent PH in obesity individuals. Further support for this concept is a recent study that showing that the majority of patients with OSA and PH had elevated left ventricular filling pressures [29].
The relationship between plasma ET-1 levels and echocardiographic findings has previously been reported in COPD patients with pulmonary hypertension [30], but this association has not been previously demonstrated in obese patients with or without OSA. In the present study, we found a positive correlation between estimated systolic pulmonary artery pressure and plasma ET-1 levels only in obese subjects, both with and without OSA, while in normal weight patients with OSA, ET-1 levels did not correlate to PAPs. These data confirm previous observations in patients with OSA, in which ET-1 plasma levels were not elevated as compared with the control group. Furthermore, these concentrations did not significantly change during sleep or after continuous positive airway pressure (cPAP) therapy [31]. Conversely, a more recent study of OSA patients showed increased circulating ET-1 levels which did not decrease after 1 year of cPAP [21]. However, both of these observational studies were performed in a small number of patients.
With regard to obesity, plasma ET-1 levels have been previously found to be significantly higher in obese patients than in controls [32]. In addition, increased plasma ET-1 levels have been observed in obese normotensive and hypertensive subjects [15]. Whether ET-1 plays a pathogenic role in obesity is not clear; however, increased vascular ET-1 mRNA and protein levels have been disclosed in experimental obesity [20]. The presence of higher circulating levels of ET-1 in obese patients in the present study which correlate with echocardiographic assessment suggests an important role of obesity in determining increased concentrations of some crucial vasoconstrictor and remodeling mediators, such as Endothelin-1. Interestingly, ET-1 plasma concentrations were similar in all obese patients, while the value of PAPs was significantly higher only in obese patients with OSA. Thus, obesity may promote endothelial pulmonary dysfunction, while the coexistence with OSA might accelerate the evolution toward PH. These data are confirmed by another study, which disclosed obesity as an important risk factor for developing PH; in particular, OHS patients were significantly more likely to suffer “cor pulmonale” compared with patients with OSA only [33]. However, the role of obesity induced endothelial dysfunction in pulmonary hypertension is still under active investigation. In addition, despite the prevalence of sleep-disordered breathing and central sleep apnea appears to be much higher in PH patients than controls [34], our findings did not confirm this previous observation, thus the number of central apneas of the patients recruited was very low.
There are several limitations to this study. One is the lack of observation of follow-up plasma ET-1 levels and PAPs in OSA patients after cPAP treatment. It would be interesting to observe whether this relationship still persists after cPAP therapy, in order to determine whether these relationships are modifiable. Furthermore, a better characterization of the comparison cohorts would have been ideal, but that data was not available to us. The golden standard for the diagnosis of PH is not echocardiography but right heart catheterization (RHC). A recent systematic literature review revealed that the correlations between estimated pulmonary artery systolic pressure on echocardiography and PAPs measured by RHC differed dependent on the etiologies of PH [35]; however, we used other echocardiographic parameters to reinforce the diagnosis of PH, such as increased size of the right heart chambers, right heart dysfunction (assessed by TAPSE), and abnormal movement of the interventricular septum. Finally, the number of patients evaluated is too small to make definitive statements, however the results are significant and we believe that they demonstrate that obesity plays a more significant role than OSA in predisposing patients toward to PH.
In conclusion, we found a positive relationship between echocardiographic assessment and plasma endothelin-1 levels in obese patients with and without obstructive sleep apnea. We suggest that pulmonary hypertension should be early considered in patients with obesity and exertional dyspnea. If elevated pulmonary pressures are documented by echocardiography, further investigations are needed to define the diagnosis and eventually establish an accurate therapy.
Abbreviations
- AHI:
-
Apnea hypopnea index
- BMI:
-
Body mass index
- cPAP:
-
Continuous positive airway pressure
- ET-1:
-
Endothelin-1
- OSA:
-
Obstructive sleep apnea
- PAPs:
-
Systolic pulmonary artery pressure
- PH:
-
Pulmonary hypertension
- TAPSE:
-
Tricuspid annular plane systolic excursion
References
Strobel RJ, Rosen RC (1996) Obesity and weight loss in obstructive sleep apnea: a critical review. Sleep 19(2):104–115
Lavie L (2003) Obstructive sleep apnoea syndrome—an oxidative stress disorder. Sleep Med Rev 7(1):35–51, Review
Testelmans D, Tamisier R, Barone-Rochette G et al (2013) Profile of circulating cytokines: impact of OSA, obesity and acute cardiovascular events. Cytokine 62(2):210–216
Chung S, Yoon IY, Shin YK et al (2007) Endothelial dysfunction and C-reactive protein in relation with the severity of obstructive sleep apnea syndrome. Sleep 30:997–1001
Htoo AK, Greenberg H, Tongia S et al (2006) Activation of nuclear factor κB in obstructive sleep apnea: a pathway leading to systemic inflammation. Sleep Breath 2006(10):43–50
He Q, Yang QC, Zhou Q, Zhu H et al (2014) Effects of varying degrees of intermittent hypoxia on proinflammatory cytokines and adipokines in rats and 3T3-L1 adipocytes. PLoS One 9(1), e86326
Ferri C, Bellini C, De Angelis C et al (1995) Circulating endothelin-1 concentrations in patients with chronic hypoxia. J Clin Pathol 48(6):519–524
Friedman JK, Nitta CH, Henderson KM et al (2014) Intermittent hypoxia-induced increases in reactive oxygen species activate NFATc3 increasing endothelin-1 vasoconstrictor reactivity. Vascul Pharmacol 60(1):17–24
Dempsey JA, Veasey SC, Morgan BJ, O’Donnell CP (2010) Pathophysiology of sleep apnea. Physiol Rev 90(1):47–112
Sajkov D, McEvoy RD (2009) Obstructive sleep apnea and pulmonary hypertension. Prog Cardiovasc Dis 51(5):363–370, Review
Friedman SE, Andrus BW (2012) Obesity and pulmonary hypertension: a review of pathophysiologic mechanisms. J Obes 50(5):274
Bastard JP, Maachi M, Lagathu C et al (2006) Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw 17(1):4–12
Prieto D, Contreras C, Sánchez A (2014) Endothelial dysfunction, obesity and insulin resistance. Curr Vasc Pharmacol 12(3):412–426
Mauricio MD, Aldasoro M, Ortega J, Vila JM (2013) Endothelial dysfunction in morbid obesity. Curr Pharm Des 19(32):5718–5729, Review
Ferri C, Bellini C, Desideri G et al (1995) Plasma endothelin-1 levels in hypertensive and normotensive men. Diabetes 44:431–436
McQuillan BM, Picard MH, Leavitt M, Weyman AE (2001) Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 104(23):2797–2802
Cuspidi C, Sala C, Rescaldani M, Tadic M, Grassi G (2014) Effects of bariatric surgery on right ventricular structure and function. J Cardiovasc Med (Hagerstown) 15(10):731–737
American Thoracic Society (1995) Standardization of spirometry, 1994 update. Am J Respir Crit Care Med 152:1107–1136
Berger M, Haimowitz A, Van Tosh A, Berdoff RL, Goldberg E (1985) Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol 6:359–365
Traupe T, D’Uscio LV, Muenter K, Morawietz H, Vetter W, Barton M (2002) Effects of obesity on endothelium-dependent reactivity during acute nitric oxide synthase inhibition: modulatory role of endothelin. Clin Sci (Lond) 103:13S–15S
Zamarrón C, Riveiro A, Gude F (2011) Circulating levels of vascular endothelial markers in obstructive sleep apnoea syndrome. Effects of nasal continuous positive airway pressure. Arch Med Sci 7(6):1023–1028
Vgontzas AN, Tan TL, Bixler EO, Martin LF, Shubert D, Kales A (1994) Sleep apnea and sleep disruption in obese patients. Arch Intern Med 154(15):1705–1711
Simonneau G, Robbins IM, Beghetti M et al (2009) Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 54(1 Suppl):S43–S54
Minai OA, Ricaurte B, Kaw R et al (2009) Frequency and impact of pulmonary hypertension in patients with obstructive sleep apnea syndrome. Am J Cardiol 104(9):1300–1306
Mokhlesi B (2010) Obesity hypoventilation syndrome: a state-of-the-art review. Respir Care 55(10):1347–1362, discussion 1363-5. Review
Wong CY, O’Moore-Sullivan T, Leano R, Byrne N, Beller E, Marwick TH (2004) Alterations of left ventricular myocardial characteristics associated with obesity. Circulation 110(19):3081–3087
Segers VF, Brutsaert DL, De Keulenaer GW (2012) Pulmonary hypertension and right heart failure in heart failure with preserved left ventricular ejection fraction: pathophysiology and natural history. Curr Opin Cardiol 27(3):273–280
Zamanian RT, Hansmann G, Snook S et al (2009) Insulin resistance in pulmonary arterial hypertension. Eur Respir J 33(2):318–324
Leung CC, Moondra V, Catherwood E, Andrus BW (2010) Prevalence and risk factors of pulmonary hypertension in patients with elevated pulmonary venous pressure and preserved ejection fraction. Am J Cardiol 106(2):284–286
Carratu P, Scoditti C, Maniscalco M et al (2008) Exhaled and arterial levels of endothelin-1 are increased and correlate with pulmonary systolic pressure in COPD with pulmonary hypertension. BMC Pulm Med 26(8):20
Grimpen F, Kanne P, Schulz E, Hagenah G, Hasenfuss G, Andreas S (2000) Endothelin-1 plasma levels are not elevated in patients with obstructive sleep apnoea. Eur Respir J 15(2):320–325
Ferri C, Bellini C, Desideri G et al (1997) Circulating endothelin-1 levels in obese patients with the metabolic syndrome. Exp Clin Endocrinol Diabetes 105:38–40
Berg G, Delaive K, Manfreda J, Walld R, Kryger MH (2001) The use of health-care resources in obesity-hypoventilation syndrome. Chest 120(2):377–383
Javaheri S, Javaheri S, Javaheri A (2013) Sleep apnea, heart failure, and pulmonary hypertension. Curr Heart Fail Rep 10(4):315–320
Finkelhor RS, Lewis SA, Pillai D (2015) Limitations and strengths of doppler/echo pulmonary artery systolic pressure-right heart catheterization correlations: a systematic literature review. Echocardiography 32(1):10–18
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Author contributions
PC conceived the study, designed the study, analyzed data, and wrote the manuscript. VAV designed the study, carried out and analyzed data, and revised the manuscript. MM analyzed data and critically revised the manuscript. SD contributed to data collection, preparation of the manuscript, and approval of the final version of the manuscript. SB contributed to data collection, analysis of data, and preparation of the manuscript. RR contributed to preparation of the manuscript and revision and approval of the final version of the manuscript. VNQ contributed to data collection, preparation of the manuscript, and approval of the final version of the manuscript. AV analyzed data and critically revised the manuscript. FD performed echocardiography, analyzed data, and revised the manuscript in the final version. MMC designed the study, analyzed data, and revised the manuscript. BAP edited the manuscript, critically revised the manuscript, and approved the final version of the manuscript. OR contributed to the study design, review and interpretation of data, revised the manuscript, and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carratù, P., Ventura, V.A., Maniscalco, M. et al. Echocardiographic findings and plasma endothelin-1 levels in obese patients with and without obstructive sleep apnea. Sleep Breath 20, 613–619 (2016). https://doi.org/10.1007/s11325-015-1260-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-015-1260-5