Abstract
Study objectives
It has been shown that volume exhaled in the first 0.5 s after application at the mouth of 5 cmH2O negative pressure (V,NEP0.5) during wakefulness strongly reflects critical pressure (Pcrit) during sleep but only in males with neck circumference (NC) >37 cm. The aim of this study was to establish the relationship between upper airway (UA) size and V,NEP0.5, to obtain V,NEP0.5 values as percent predicted and then correlate them with Pcrit obtained in the same subjects.
Patients and measurements
In 20 (8 women) normal subjects (age, 39 ± 16 years; BMI, 22.5 ± 3.0 kg/m2; AHI, 0.8 ± 1.0), NC, mean pharyngeal cross-sectional area (APmean) by acoustic pharyngometry and V,NEP0.5 in the supine position were measured. Correlations between APmean, NC and V,NEP0.5 were performed. A strong relationship was found between APmean and NC, and the predicted V,NEP0.5 values were obtained using the equation derived from the relationship between V,NEP0.5 and NC.
Subsequently, nine normal subjects (age, 26.3 ± 2.5 yrs, BMI 23.9 ± 3.2 kg/m2, AHI 2.3 ± 0.5), ten snorers (age, 68 ± 11 years; BMI, 26.6 ± 4.6 kg/m2; AHI, 3.5 ± 0.8) and ten OSAH patients (age, 64 ± 9 years; BMI, 32 ± 4.9 kg/m2; AHI, 43.8 ± 24.4) underwent measurement of V,NEP0.5 in the supine position while awake and Pcrit during sleep. Correlations between Pcrit and both V,NEP0.5 and V,NEP0.5 expressed as percent predicted were performed in all subjects.
Results
Controls had V,NEP0.5 of 387 ± 103 mL (100.1 ± 13% predicted) and Pcrit of −3.7 ± 2.0 cmH2O, snorers had V,NEP0.5 of 320 ± 33 mL (62 ± 12% predicted) and Pcrit of −0.6 ± 0.3 cmH2O while OSAH patients had V,NEP0.5 of 295 ± 67 mL (48 ± 12% predicted) and Pcrit of 1.0 ± 1.0 cmH2O. The linear regression analysis showed a close and highly significant correlation between V,NEP0.5 percent predicted and Pcrit (r 2 = 0.79, p < 0.001).
Conclusions
V,NEP0.5 expressed as percent predicted according to NC strongly reflects Pcrit in a wide range of values and can be used as a surrogate of Pcrit to assess UA collapsibility independently from UA size and sex.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea–hypopnea (OSAH) is a condition characterized by the pharynx being more collapsible than normal. It has been repeatedly shown that critical pressure (Pcrit), defined as the nasal pressure at which upper airways (UA) are completely closed and airflow ceases during sleep, is higher in OSAH patients compared to normals [1–3].
Although it has been shown that the severity of OSAH is not related to the degree of UA collapsibility, an elevated Pcrit can be considered as a predisposing factor that, in association with a disrupted or ineffective response of dilator muscles of the pharynx, determines the occurrence of OSAH [4]. Therefore, UA critical pressure could be an interesting clinical parameter, but it is usually limited solely to a research consideration because of its difficult assessment.
Recently, a new method to assess UA collapsibility based on the application of a negative expiratory pressure (NEP) at the mouth of the subjects while awake has been introduced and validated as surrogate of passive Pcrit [5–7]. As UA dilator muscles exhibit a reflex activation only after 0.5 s following the application of a small negative pressure at the onset of quiet tidal expiration [8], the volume expired in the first 0.5 s after applying NEP of 5 cmH2O at the mouth (V,NEP0.5) has been proposed as an alternative measure of the UA passive properties.
In a recent work, it has been assumed that a value higher than 400–500 mL of V,NEP0.5 could reasonably exclude OSAH, but only in subjects with neck circumference >37 cm. Indeed, we found mean values lower than 300 mL in healthy subjects (mainly in women) with lower neck circumferences [6].
Actually, if we consider the pharynx in hypotonic conditions as a collapsible tube in which pressure changes applied to the upstream segment (mouth) are transmitted to the flow-limited segment (oropharynx), maximum flow (\( {\dot V_{\max }} \)) is determined by tube cross-sectional area (XSA), tube compliance (∆XSA/∆P), and gas density (ρ) as expressed in the tube law [9, 10].
So, it is reasonable to suppose that V,NEP0.5 could be affected by UA cross-sectional area, particularly in children, women, and men with small upper airways.
The aim of this study was to evaluate the relationship between UA size and V,NEP0.5 in order to normalize V,NEP0.5 values for UA dimensions and then correlate them with Pcrit values obtained in the same subjects. UA dimensions have been assessed by acoustic reflection technique and afterwards by NC measure which is more easily obtainable in all clinical settings.
Patients and methods
Patients
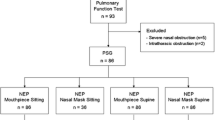
The subjects were recruited in our Sleep Laboratory from November 2008 to January 2010. Ten patients with a sleep study showing moderate or severe OSAH (AHI > 15/h), 10 snorers (snoring time ≥30% of sleep time) without OSAH (AHI ≤5), and 29 subjects without OSAH (AHI < 5/h) and snoring were studied. We excluded those with anatomical defects such as craniofacial and/or severe otorinolaryngoiatric abnormalities, or with neurological and endocrine diseases. Patients were not treated with drugs active on the central nervous system or who suffered from chronic alcoholism. All patients, before being enrolled, underwent arterial blood gas analysis and spirometry in order to exclude the presence of resting hypercapnia (PaCO2 ≥ 45 mmHg) and/or ventilatory dysfunction. The study was approved by our local Ethics Committee, and all patients gave written informed consent.
Study protocol
After the baseline sleep study, all the enrolled subjects underwent evaluation of UA collapsibility by the NEP technique in the supine position while awake in the afternoon. Healthy subjects also underwent assessment of UA XSA by the acoustic pharyngometer technique in the sitting position. Pcrit was assessed during supine sleep the following night in ten OSAH patients, ten snorers, and nine healthy subjects.
NEP test
UA collapsibility was assessed by computing the volume exhaled at the mouth during the first 0.5 s after the application of −5 cmH2O NEP (V,NEP0.5). This technique is fully described elsewhere [5]. Briefly, NEP was applied 10 min after the subjects assumed the supine position. In this position, at least six NEP breath tests were performed at intervals of five to ten respiratory cycles, always when the patient had resumed regular breathing as determined by a computer-generated spirogram. In this respect, great care was placed to check the level of the end-expiratory lung volume. Acceptable manoeuvres had to be without drift between the curves on the spirogram, without any cough or glottis closure, and with the application of the negative pressure within the first 200 ms or 0.10 L/s flow after the start of the expiratory phase. Intra-thoracic tidal expiratory flow limitation was excluded by the NEP technique, checking that the flow during NEP was never superimposed on the flow during the previous control tidal expiration. Then, the expiratory flow under each NEP application was recorded in order to compute, by time integration, the volume exhaled in the first 0.5 s after the start of NEP, henceforth labelled V,NEP0.5. V,NEP0.5 was calculated, after discarding the highest and the lowest values of the six, by averaging those obtained during at least four acceptable NEP manoeuvres.
Acoustic pharyngometry and neck circumference
UA anatomy was evaluated in the seated position by means of acoustic pharyngometry (‘Eccovision’ Hood Laboratories, Pembroke, MA, USA). It uses acoustic reflection technology to assess cross-sectional areas from the oral cavity to the hypopharynx by calculating changes in acoustic impedance that occur along these UAs with variable calibre. This technique is fully described elsewhere [11, 12]. We obtained traces that represent UA cross-sectional area versus distance down the airway. Four technically acceptable traces (variability ≤10%) were taken at the end of resting expiration. We examined the UA XSA for the presence of a standard mouth peak, oropharyngeal junction (OPJ) valley, pharyngeal peak (APmax) and glottic valley. The mean pharyngeal area (APmean) represents the mean area from the OPJ to the glottis and can be used for evaluation of mean pharyngeal calibre. After the execution of acoustic pharyngometry, we measured the circumference of the neck in the seated position at the superior border of the cricothyroid cartilage with a tape measure.
Assessment of passive Pcrit
Passive Pcrit, which reflects the mechanical properties of the UA without taking into account the neuromuscular response to UA obstruction, was determined during NREM sleep as previously described elsewhere [13]. Briefly, a nasal mask was applied to the subject, connected to a CPAP machine (HC221LE, Fisher and Paykell), and a pressure that eliminated any obstructive events (including snoring and flow limitation), so-called ‘holding pressure’, was set. Nasal pressure was assessed continuously at the mask, and airflow was measured through a pneumotachograph (Hans-Rudolph, Kansas City, MO) positioned between the mask and the CPAP device. Subjects slept in the supine position with one pillow under their heads during the measurement period. The nasal pressure was abruptly lowered for five breaths and brought up to the holding pressure. Nasal pressure was reduced again to increasingly lower values after re-establishing at least 1 min of sleep at the holding pressure. A minimum of two runs of stepwise reductions in nasal pressure by 1–2 cmH2O that eventually encompassed zero airflow (Pcrit) was performed.
In snorers and healthy subjects, Pcrit resulted subatmospheric, and a negative pressure was applied to measure it in order to obtain a stepwise reduction in pressure and flow. In these subjects, CPAP was substituted with a portable negative pressure circuit connected to the mask via a pneumotachograph. Pcrit of the upper airway was determined by plotting the peak inspiratory airflow (\( {\dot V_{{\text{i}},\max }} \)) against nasal pressure under the hypotonic conditions occurring during sleep. Linear regression was applied to the obtained values, and Pcrit was identified as the intercept in the pressure axis when flow was zero.
Data analysis
Linear regressions were performed between different variables of interest, and the determination coefficients were established. Analysis of variance was performed by the Kruskall–Wallis test among the three groups of subjects for BMI, neck circumference, AHI, Pcrit and V,NEP0.5. If the p value was significant, multiple comparisons were made using the Mann–Whitney test. Statistical significance was assumed for p < 0.05. Data are presented as means ± SD. All statistical analyses were made using Graph Pad Prism 4.02 (MacKiev Software, Boston, MA, USA) version for Windows software.
Results
Thirteen women and 36 men, all Caucasian, were enrolled in the study protocol. Initially, we evaluated 20 healthy subjects (age, 39 ± 16 years; BMI, 22.5 ± 3 kg/m2; AHI, 0.8 ± 1) as reference population, and we measured neck circumference, APmean and absolute V,NEP0.5 values (Table 1). A close correlation was observed between APmean and V,NEP0.5 (p < 0.0001, r 2 = 0.79), NC and APmean (p < 0.0001, r 2 = 0.72), NC and V,NEP0.5 (p < 0.0001, r 2 = 0.74). From this latest correlation, we derived the following equation (Fig. 1):
which allowed us to calculate the predicted V,NEP0.5 values based on neck circumference. Afterwards, to validate such a prediction equation, we assessed as a study population three groups composed of nine other healthy subjects (5 female; age, 26.3 ± 2.5 years; BMI, 23.9 ± 3.2 kg/m2; AHI, 2.3 ± 0.5) and ten snorers (age, 68 ± 11 years; BMI, 26.6 ± 4.6 kg/m2; AHI, 3.5 ± 0.8) and ten OSAH (age, 64 ± 9 years; BMI, 32 ± 4.9 kg/m2; AHI, 43.8 ± 24.4), the V,NEP0.5 and Pcrit of whom have previously been measured in our lab [7].
a Relationship between mean pharyngeal area (APmean) obtained with acoustic pharyngometry and volume exhaled in the first 0.5 s after application of −5 cmH2O at the mouth (V,NEP0.5) in 20 normals. Black points represent men; white points, women. b Relationship between neck circumference and APmean in the same population of 20 normals as in a. c Relationship between neck circumference and V,NEP0.5 in the same population of 20 normals as in a and b
There was a significant difference in age between healthy subjects and snorers and between healthy subjects and OSAH patients (p < 0.05). Patients with OSAH had higher BMI, neck circumference and AHI (p < 0.05) as compared to snorers and healthy subjects. Snorers had higher neck circumference and BMI as compared to healthy subjects (p < 0.05) (Table 2).
In Table 2, Pcrit, V,NEP0.5 in absolute values, neck circumference, V,NEP0.5 predicted values and V,NEP0.5 as percent predicted are shown for nine normal subjects, ten snorers and ten OSAH patients. Normal subjects had higher V,NEP0.5 compared to OSAH patients and snorers (p < 0.001), and OSAH patients had higher Pcrit compared to snorers (p < 0.05) and normals (p < 0.001). A significant tight correlation was found in the three groups between Pcrit and V,NEP0.5 percent predicted (p < 0.001, r 2 = 0.79) (Fig. 2).which was much better than the correlation between Pcrit and absolute V,NEP0.5 (p < 0.001, r2 = 0.53).
Discussion
This study shows that in normal subjects, V,NEP0.5 is directly related to the UA size, as reflected by both APmean and NC. More important is the finding that V,NEP0.5, expressed as percent predicted, is more closely related to Pcrit than is absolute V,NEP0.5 in healthy subjects and patients with SDB.
At the beginning of the quiet tidal expiration, the application of a small negative pressure (NEP) at the mouth for 500 ms does not elicit any appreciable reflex activity of the genioglossus in awake supine subjects. Under these circumstances, assessment of expiratory flow change, as related to a corresponding change in upper airway calibre, should likely reflect passive upper airway collapsibility. Absolute V,NEP0.5 values have been previously shown to correlate to Pcrit in male subjects with NC greater than 37 cm, either healthy or suffering from SDB [7]. However, in subjects with a small neck circumference and presumably small UA size such as women and children, absolute V,NEP0.5 values may be heavily influenced by the UA dimension beside UA collapsibility. V,NEP0.5 is the integral of the expiratory flow in the first 0.5 s of NEP application and can be influenced by both anatomical size and the degree of collapse of upper airways. Taking into account the upper airway size, high percent predicted values of this parameter reflect little upper airway collapsibility and vice versa.
To challenge this hypothesis, we tried to establish the relationship between V,NEP0.5 and neck circumference and UA size (i.e. APmean) in normal adults with a wide range of neck dimension in order to calculate the V,NEP0.5 predicted values using the corresponding reference equations.
In normal subjects, absolute V,NEP0.5 values were lower for smaller neck dimensions and UA size, as assessed by NC or APmean, in all instances showing a linear correlation good enough to derive simple reference equations for computing predicted values. Considering the close relationship between APmean and NC, we chose to refer to the predicted values of V,NEP0.5 based on the NC relationship, since NC is much easier to measure than APmean.
By using this equation, the V,NEP0.5 predicted values were obtained in a group of 29 individuals without and with SDB, with the purpose of comparing the relationship between absolute and percent predicted V,NEP0.5 values with Pcrit measured in the same subjects. The correlation with Pcrit was better for V,NEP0.5 expressed as percent predicted instead of absolute values, suggesting a greater utility for V,NEP0.5 percent predicted for assessing UA collapsibility, especially when NC is less than 38 cm, as often is the case in women and children.
The main limitation of the study is the lack of women in the OSA and snorer groups; moreover, we limited our assessment to passive Pcrit as we consider minimal the contribution of UA neuromuscular reflex in determining the volume exhaled in the first 0.5 s after application of NEP while awake. However, further studies are needed to investigate if a relationship between V,NEP and active Pcrit also exists.
Although it has been shown that Pcrit is not related to the severity of sleep apnea [4, 7], assessment of collapsibility could be a useful tool to determine the risk of obstructive sleep apnea for screening purposes. A V,NEP0.5 value <500 mL or a V,NEP0.5 percent predicted value <80% could be associated with a higher risk of having sleep apnea.
Hence, it would be helpful to validate this method in a cohort of children where Pcrit measurements are very difficult and V,NEP0.5 (percent predicted) might be adequate and useful to evaluate the UA collapsibility and the risk of OSAH (and the need of polysomnographic studies) in such a population. In conclusion, V,NEP0.5, expressed as percent predicted, strongly reflects Pcrit in a wide range of values and can be used as a surrogate of Pcrit to assess UA collapsibility for clinical and research purposes independently from UA size and sex.
References
Gleadhill IC, Schwartz AR, Schubert N, Wise RA, Permutt S, Smith PL (1991) Upper airway collapsibility in snorers and in patients with obstructive hypopnea and apnea. Am Rev Respir Dis 143:1300–1303
Smith PL, Wise RA, Permutt S (1988) Upper airway pressure-flow relationships in patients with obstructive sleep apnea. J Appl Physiol 64:789–795
Owens RL, Malhotra A, Eckert DJ, White DP, Jordan AS (2010) The influence of end-expiratory lung volume on measurements of pharyngeal collapsibility. J Appl Physiol 108(2):445–451
Younes M (2003) Contributions of upper airway mechanics and control mechanisms to severity of obstructive apnea. Am J Respir Crit Care Med 168:645–658
Ferretti A, Giampiccolo P, Redolfi S, Mondini S, Cirignotta F, Cavalli A, Tantucci C (2006) Upper airway dynamics during negative expiratory pressure in apneic and non-apneic awake snorers. Respir Res 30:47–54
Corda L, Redolfi S, Taranto Montemurro L, La Piana GE, Bertella E, Tantucci C (2009) Short- and long-term effects of CPAP on upper airway anatomy and collapsibility in OSAH. Sleep Breath 13:187–193
Taranto Montemurro L, Bettinzoli M, Corda L, Braghini A, Tantucci C (2010) Relationship between critical pressure and volume exhaled under negative pressure awake subjects with sleep disordered breathing. Chest 137(6):1304–1309
Tantucci C, Mehiri S, Duguet A, Similowski T, Arnulf I, Zelter M, Derenne JP, Milic-Emili J (1998) Application of negative respiratory pressure during expiration and activity of genioglossus in humans. J Appl Physiol 84:1076–1082
Dawson SV, Elliott EA (1977) Wave-speed limitation on expiratory flow—a unifying concept. J Appl Physiol 43:498–515
Younes M (2008) Role of respiratory control mechanisms in the pathogenesis of obstructive sleep disorders. J Appl Physiol 105:1389–1405
Marshall I, Maran NJ, Martin S, Jan MA, Rimmington JE, Best JJ, Drummond GB, Douglas NJ (1993) Acoustic reflectometry for airway measurements in man: implementation and validation. Physiol Meas 14:157–169
Fredberg JJ, Wohl ME, Glass GM, Dorkin HL (1980) Airway area by acoustic reflections measured at the mouth. J Appl Physiol 48:749–758
Patil SP, Punjabi NM, Schneider H, O'Donnell CP, Smith PL, Schwartz AR (2004) A simplified method for measuring critical pressures during sleep in the clinical setting. Am J Respir Crit Care Med 170:86–93
Acknowledgements
The authors acknowledge Mr. Michele Guerini and Mr. Joseph S. Gabriel for their invaluable technical and editorial assistance.
Conflict of interest
Luigi Taranto Montemurro, Michela Bettinzoli, Luciano Corda, Stefania Redolfi, Mauro Novali, Alessia Braghini and Claudio Tantucci have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Taranto Montemurro, L., Bettinzoli, M., Corda, L. et al. Influence of upper airway size on volume exhaled under negative pressure during evaluation of upper airway collapsibility. Sleep Breath 16, 399–404 (2012). https://doi.org/10.1007/s11325-011-0511-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-011-0511-3