Abstract
Background
Congenital central hypoventilation syndrome (CCHS) is a rare condition that usually presents soon after birth and is potentially life-shortening if not treated. The defining abnormality is hypoventilation during sleep which requires life-long treatment with artificial ventilation. This syndrome may also be associated with generalised dysfunction of the autonomic nervous system and a sub-group with associated Hirschsprung’s disease. The genetic basis of CCHS has been identified as mutations in the PHOX2B gene.
Methods
We present four families, three with autosomal dominant inheritance and familial clustering, and one with a de novo mutation resulting in CCHS.
Conclusions
We demonstrate that nasal mask ventilation from birth can provide adequate treatment and improved quality of life for these children. Phenotypic variability in expression of disease is seen in families with the same mutations in PHOX2B gene. The psychosocial costs of the disease and the unrecognised ‘morbidity barter’ that is part of current management needs to be factored into in all stages of management from childhood to adolescence to adulthood.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
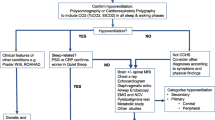
Congenital central hypoventilation syndrome (CCHS), previously known as “Ondine’s curse”, is characterised by marked reduction in ventilatory sensitivity to hypercapnia and hypoxemia, which can be demonstrated during both sleep and wakefulness. This lack of automatic ventilatory control also means that CCHS manifests during non-REM and particularly slow wave sleep when breathing is driven by automatic responses. CCHS is traditionally diagnosed by presence of marked hypoventilation during sleep after exclusion of primary neuromuscular, cardiac, respiratory or brainstem pathologies. It usually presents soon after birth. Anomalies of the autonomic nervous system (ANS; Hirschsprung’s disease, cardiac arrhythmias, pupillary abnormalities, sweating and tumours of neural crest derivatives) are expressed with lower penetrance [1, 2].
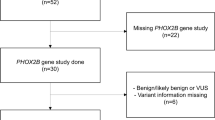
The recent characterisation of the genetic basis of this condition now allows genetic testing [2, 3] Poly-alanine repeat expansion mutations in the paired-like homeobox PHOX2B gene were noted in more than 90% of cases and alternative nonpolyalanine repeat expansions in the rest [4]. The mutations can occur as a heterozygous de novo mutation and are passed on in an autosomal dominant (AD) manner [5–7]. With improvement in genetic diagnosis of CCHS, phenotype descriptions and importance of different domains of PHOX2B protein are likely to emerge.
From a clinical perspective, CCHS presents a significant financial and psychosocial burden to the families of affected children [1]. A range of neuropsychological abnormalities have been reported in children with CCHS [8]. Adequate care requires a multidisciplinary approach that is flexible enough to accommodate changes in the patient’s health and psychosocial states. Management strategies are limited and ongoing review is required to improve quality of life and outcomes.
We present four families and review aspects of the management that these cases have highlighted, with the aim of illustrating emerging strategies for the clinical management of this disorder.
Family 1
The proband was a baby girl who presented with multiple episodes of apnoea and oxygen desaturation shortly after birth requiring invasive mechanical ventilation (IMV). Her father had a known diagnosis of CCHS but was not, himself, aware of the genetic nature of the disorder. Her father had been one of the early survivors of CCHS in our clinical service who required management as a hospital in-patient until around the age of 5 years. As an adult, he had clinical evidence of memory and social dysfunction.
In this girl, magnetic resonance imaging (MRI) of the brain and electroencephalogram (EEG) were normal. Elevated lactate levels within the basal ganglia identified by magnetic resonance spectroscopy were consistent with the occurrence of hypoxic events. Polysomnography showed significant oxygen and carbon dioxide abnormalities occurring after sleep onset. The diagnosis of CCHS was made on the basis of these results in conjunction with the family history of an affected father. Genetic sequencing on the patient, her father and paternal grandmother showed a heterozygous in-frame duplication resulting in a five alanine expansion of the PHOX2B gene. The paternal grandmother, although relatively asymptomatic in the past, will now be managed with pressure support during sleep.
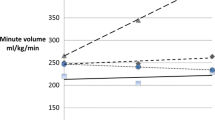
Non-invasive mask ventilation (NIV) with portable, bi-level pressure support ventilation (BiPAP synchrony Respironics, ST mode) was commenced at 3 weeks of age. Horizontal and vertical tilt tests (available at that time on an experimental basis), performed to evaluate ANS, were abnormal.
The infant was discharged at 3 months of age with a plan to remain on BiPAP support during all sleep periods. Bi-level titration studies were performed every 2 months during the first year 2 years of life, then every 6 months to review ventilation needs, with concurrent machine and mask-fitting sessions to ensure that the equipment was altered to appropriately follow her growth. At the time of this report, she is 7 years old, on nocturnal BiPAP, at pressure settings of 18/5 and rate of 22/min and cared for primarily by her paternal grandparents. She participates in normal school and family activities. Prolonged use of a nasal mask for ventilation has led to mild mid-face hypoplasia. Cardiac screening has demonstrated no evidence of pulmonary hypertension. Formal neuro-developmental assessment performed prior to school commencement was normal.
Family 2
The proband was baby girl presented with apnoea with respiratory acidoses shortly after birth requiring IMV. There was no family history of CCHS.
MRI of brain was normal. Seizure activity on EEG and slightly elevated lactate level in the cerebrospinal fluid were considered to be consistent with the occurrence of hypoxic events. Rectal biopsy, performed in view of delayed passage of meconium, ruled out aganglionosis. Attempts to extubate were unsuccessful due to recurrence of hypoventilation and respiratory acidosis. The infant was diagnosed with CCHS on clinical grounds with inadequate ventilatory efforts during both wakefulness and sleep. Genetic sequencing showed a seven alanine expansion of the PHOX2B gene that was concluded to be the result of a de novo mutation. Sequencing studies on her parents were negative.
In view of her continuous ventilation requirements, a tracheostomy was performed. The clinical course in early infancy was complicated by intermittent episodes of hypoglycaemia necessitating treatment with oral diazoxide. The aetiology for hypoglycaemia could not be identified. The levels of insulin and other counter-regulatory hormones and a meta-ido-benzyl-guanidine scan (to detect a neuro-endocrine tumour secreting insulin) were normal. At the age of 11 months, she was home 4 days per week and otherwise managed within the paediatric intensive care unit. She was discharged to full-time home care at the age of 15 months (delayed because of the need to access home carers). Continuous mechanical ventilation (Tag Medical LPV1000 pressure ventilation volume cycled) is provided via a tracheostomy. At 3 years and 10 months of age, she continues to require full-time ventilation. Formal assessment of her developmental skills showed a cognitive equivalent to 17 months of age, fine motor skills 2 years and gross motor skills equivalent to 18–21 months with her major delay in social interaction, communication (limited vocalisation) and play skills.
Family 3
The proband in this family was an infant girl, who was considered at risk of congenital central hypoventilation syndrome at birth. Her mother was diagnosed with CCHS by polysomnography and genetic testing. The maternal history was of breathing difficulties soon after birth and nocturnal ventilation was commenced at the age of 4 years via a tracheostomy. The mother has had intermittent episodes of cardiac failure attributed to inadequate nocturnal ventilation; the mother has cognitive deficits, although these have not been formally tested. Her older brother had undergone polysomnography as an infant which was reported to be normal. His history included long-term association with paediatric and behavioural services in the community because of poor daytime behaviour.
This girl was admitted to the newborn intensive care unit after birth in view of her maternal history. Intermittent episodes of oxygen desaturation were noted. She underwent a sleep study which was deemed negative and was transferred to a peripheral hospital close to home for observation, on continuous oximetry, without respiratory support. Worsening episodes of oxygen desaturation occurred which led to review at 1 month of age and the commencement of BiLevel pressure support ventilation. She was positive for PHOX2B gene mutation with five alanine repeats which is the same mutation as her mother and older brother who was tested at the age 8 years, following her birth and positive diagnosis. The sleep study at the age of 8 years in her older brother was abnormal and he was commenced on BiLevel pressure support ventilation during sleep periods at that time, but has ongoing behavioural issues which have interfered with his compliance with his nocturnal ventilation.
At the age of 13 months, she is growing and developing well. She is managed on BiLevel pressure support ventilation (Weinmann Bi-level ST22 Spontaneous time mode) during all sleep periods with settings of 18/5 and rate of 22/min. She was discharged from our tertiary centre to a peripheral hospital close to home at the age of 4 months and discharged to full-time care in the home at the age of 6 months.
Family 4
This index case in this family was a girl who presented at 20 days of age with history of apnoea and cyanosis and was managed with IMV. Her father reported that he was diagnosed with “Ondine’s Curse” as a child and had now outgrown the disease. Attempts to initiate non-invasive ventilation on him had failed. Subsequently, he was lost to medical follow-up. Reported that he had attention deficit and hyperactivity disorder and limited school performance.
In this girl, MRI of brain revealed bilateral grade III intraventricular haemorrhages and thrombosis in the right transverse and sigmoid sinus. After extubation a drop in respiratory rate to <5/min whilst asleep, associated with oxygen desaturation was noted. Polysomnography revealed hypoventilation in all stages of sleep with marked oxygen desaturation and hypercarbia noted especially in NREM sleep. The infant had tracheostomy placed 2 weeks later and is managed by pressure support ventilation while sleep. The infant spent a considerable period in the hospital while arrangements were made for home care. Due to difficult social circumstances the child was under care of the state and placed in foster care. The child is now 35 months of age and ventilated through tracheostomy during sleep. She has normal developmental milestones with no neurological deficit.
Fifteen months after the daughter’s presentation, a male sibling was born who also demonstrated signs of hypoventilation. This infant demonstrated more marked hypoventilation during sleep than his sister, despite having the same mutation. In his case, early elective tracheostomy and ventilatory support was commenced. He was also placed in foster care, with the same carers as his sister, and discharged home on a government-funded package for home ventilation support.
Another 15 months later, a third (female) sibling was born at 33 weeks gestation who demonstrated signs of hypoventilation soon after birth. This female infant has a milder phenotype on polysomnography. The infant was invasively ventilated until she achieved weight gain suitable for tracheostomy and is now also ventilated via tracheostomy. This infant remains resident in the paediatric intensive care unit and is awaiting foster family placement. Blood samples for genetic testing could only be obtained after the birth of his third affected child. The father and all three affected children had positive PHOX2B gene mutation analysis with five additional alanine repeats
Discussion
We present three families of second generation inheritance of CCHS. In each of these families, all of the affected members have same poly-alanine expansion of the PHOX2B gene. Longer length of the polyalanine expansion in the PHOX2B gene region and non-poly-alanine repeat mutations are reported to produce more severe disruption of PHOX2B function [9, 10]. The affected families in our series show considerable variability in phenotype with neither consistency of expression within families, nor any association between the number of alanine repeats and severity of hypoventilation. In family 2, a relatively short mutation presented with a severe respiratory control defect. In family 1, the same mutation was noted on three generations but the phenotypic expression was different and again in family 3 the same mutation led to different expression of the disease. The same genotype in the family of case 4 has had four different degrees of severity. These observations suggest that more research is required to fully elucidate issues such as penetrance and associations between genotype and phenotype. It is imperative for clinicians to ensure that information regarding mode of transmission and genetic counselling is provided to the patients with CCHS at an appropriate age. Pre-implantation genetic diagnosis or chorionic villous sampling to detect PHOX2B mutations is possible but we are not aware of any reports of this being performed.
NIV is an accepted, less expensive and easier-to-use mode of ventilation for management of CCHS [11, 12]. NIV from birth can be considered in patients with CCHS and was reported as effective and preferred by both patients and carers [13]. In two infants (family 1 and 3), NIV was used as effective treatment for CCHS from birth and therefore precluded any need for tracheostomy. Infant one leads a relatively normal life style at home and at school. No obvious neurological deficits were noted in either of these infants. Also, they spent lesser duration of time in hospital as compared to the two probands who required invasive ventilation. NIV seemed to offer a higher level of consideration to the quality of life for both the patient and carers. Portability of the mask ventilation equipment makes it relatively easy for carers to mobilise. Prolonged mask ventilation can interfere with mid-face growth [14]. Mild mid-hypoplasia was noted in one of the reported cases. The impact of this clinical complication of NIV especially when facial phenotype can be different in PHOX2B mutations is not clear [15]. Hypothetically, inadequate pressure from mask ventilation due to lower achieved pressure can lead to pulmonary hypertension. This concern was addressed in our series by bi-level titration studies to determine a higher set pressure to compensate for the leakage and technical support. Mask ventilation can irritate face and the hypothetical risk of asphyxiation in the case of emesis has not been yet reported. Mask ventilation may replace tracheostomy ventilation later in life. The less severely affected family members of the reported cases, were commenced on ventilation using a non-invasive interface. Finally, the father in the first family was successfully transitioned from tracheostomy to mask ventilation in adolescence.
Full-time ventilation via a tracheostomy in family 2 significantly delayed home management and delayed the first overnight home visit to the age of 9 months. Invasive ventilation requires frequent reviews for progress of mechanical ventilation and the maintenance of tracheostomy. It also incurs a major financial burden on the carers, mainly arising from the need to continuous supervision, either opting out of employment or employing medically trained carers.
All affected parents in our series have suffered significant psychosocial difficulties that have increased the difficulties in managing care of their children. The father of the first infant died in sleep when not using his NIV support (something he frequently allowed). The extreme manifestation of this has been family 4 where the children are cared for by the state in foster care. Every stage of management has to be carefully planned in advance with adequate resources. Given the limited resources that is available in the state health budgets these children have spent longer periods in hospital awaiting care packages. The third infant in this family is still in the hospital awaiting placement. Medical management in controlling and treating the hypoventilation appear to be the easiest of the management steps in these children. The psychosocial costs that patients and families pay is difficult to quantify and there is no qualitative rubric available to measure them. The holistic management of these children entail a form of ‘morbidity barter’ where tracheostomy optimises ventilation but extracts a heavier psychosocial and financial price. Mask ventilation obviates many of the problems listed with tracheostomy ventilation but adequate ventilation at a crucial period of neuronal growth in childhood has to be paramount and no compromises made to achieve optimal gas exchange. Mask ventilation may compound the blunted perception of disease severity in these cases because the child appears and behaves normally when awake and does not suffer any symptoms during sleep. Presence of neuro-cognitive deficits in parent with CCHS may be due to lack of compliance with ventilatory strategies. Now that the adults with CCHS are having children of their own; addressing issue of compliance with the therapy at an appropriate age cannot be understated.
Autonomic dysfunction has been associated with this disorder with relatively low penetrance. Mild dysautonomia was noted on formal testing in first family and hypoglycaemia requiring active management in the second. Subtle autonomic abnormalities may be present in an infant with a mild phenotypic expression of the disorder suggesting that generalised autonomic dysfunction is likely to be closely associated with this disorder. The hypoglycaemia in family 2 might have resulted from generalised autonomic dysfunction. Hyperinsulinism leading to hypoglycaemia has been reported in association with CCHS [16]. The presence of severe hypoglycaemia in second infant has no cause identified other than a potential relationship to her CCHS. The subtle dysautonomia which may go unnoticed on clinical examination can be identified by formal testing. The relevance and functional implications of testing for ANS dysfunction is not clear. Formal testing of ANS can aid in management and diagnose milder variant of CCHS. The disadvantages of such testing are need for the equipment and expertise required to undertake and interpret the test which would be required infrequently. Asymptomatic autonomic dysfunction could suggest that the low penetrance for autonomic abnormalities may relate to the level of dysfunction rather than the presence or absence of the abnormalities.
Conclusion
A population of patients affected by CCHS are reaching adulthood and are having children of their own. Cognitive deficits in the current generation of CCHS-affected parents added significant difficulties to their understanding and ability to manage the condition in them and in their children. The AD mode of inheritance has significant implications for patients who were diagnosed before the underlying cause was known. Also, the clinical expression of the disease is variable in families with the same PHOX2B mutation. Nasal mask ventilation can be used from birth and to avoid tracheostomy, although it is not suitable for treating all affected infants. Despite significant advances in the management of children with CCHS, the requirement for full-time ventilation via tracheostomy continues to impose significant social and financial burdens to their family and community.
References
Vanderlaan M, Holbrok CR, Wang M, Tuell A, Gozal D (2004) Epidemiologic survey of 196 patients with congenital central hypoventilation syndrome. Pediatr Pulmonol 37:217–229
Autonomic control, congenital failure of. MIM#209880. http://www.ncbi.nlm.nih.gov/omim/209880, accessed on 08/05/2010
Gaultier C, Amiel J, Dauger S, Trang H, Lyonnet S, Gallego J, Simonneau M (2004) Genetics and early disturbances of breathing control. Pediatr Res 55:729–733
Berry-Kravis EM, Zhou L, Rand CM, Weese-Mayer DE (2006) Congenital central hypoventilation syndrome: PHOX2B mutations and phenotype. Am J Respir Crit Care Med 74:1139–1144
Hamilton J, Bodurtha JN (1989) Congenital central hypoventilation syndrome and Hirschsprung's disease in half sibs. J Med Genet 26:272–274
Weese-Mayer DE, Berry-Kravis EM (2004) Genetics of congenital central hypoventilation syndrome: lessons from a seemingly orphan disease. Am J Respir Crit Care Med 170:16–21
Antic NA, Malow BA, Lange N, McEvoy RD, Olson AL, Turkington P, Windisch W, Samuels M, Stevens CA, Berry-Kravis EM, Weese-Mayer DE (2006) PHOX2B mutation—confirmed congenital central hypoventilation syndrome presentation in adulthood. Am J Respir Crit Care Med 174:923–927
Silvestri JM, Weese-Mayer DE, Nelson MN (1992) Neuropsychologic abnormalities in children with congenital central hypoventilation syndrome. J Pediatr 120:388–393
Bachetti T, Matera I, Borghini S, Di Duca M, Ravazzolo R, Ceccherini I (2005) Distinct pathogenic mechanisms for PHOX2B associated polyalanine expansions and frameshift mutations in congenital central hypoventilation syndrome. Hum Mol Genet 14:1815–1824
Matera I, Bachetti T, Puppo F, Di Duca M, Morandi F, Casiraghi GM, Cilio MR, Hennekam R, Hofstra R, Schober JG, Ravazzolo R, Ottonello G, Ceccherini I (2004) PHOX2B mutations and polyalanine expansions correlate with the severity of the respiratory phenotype and associated symptoms in both congenital and late onset central hypoventilation syndrome. J Med Genet 41:373–380
Chen ML, Keens TG (2004) Congenital central hypoventilation syndrome: not just another rare disorder. Paediatr Respir Rev 5:182–189
Villa MP, Dotta A, Castello D, Piro S, Pagani J, Palamides S, Ronchetti R (1997) Bi-level positive airway pressure (BiPAP) ventilation in an infant with central hypoventilation syndrome. Pediatr Pulmonol 24:66–69
Ramesh P, Boit P, Samuels M (2008) Mask ventilation in the early management of congenital central hypoventilation syndrome. Arch Dis Child Fetal Neonatal Ed 3:F400–F403
Li KK, Riley RW, Guilleminault C (2000) An unreported risk in the use of home nasal continuous positive airway pressure and home nasal ventilation in children. Chest 117:916–918
Todd ES, Weinberg SM, Berry-Kravis EM, Silvestri JM, Kenny AS, Rand CM, Zhou L, Maher BS, Marazita ML, Weese-Mayer DE (2006) Facial phenotype in children and young adults with PHOX2B-determined congenital central hypoventilation syndrome: quantitative pattern of dysmorphology. Pediatr Res 59:39–45
Hennewig U, Hadzik B, Vogel M, Meissner T, Goecke T, Peters H, Selzer G, Mayatepek E, Hoehn T (2008) Congenital central hypoventilation syndrome with hyperinsulinism in a preterm infant. J Hum Genet 53:573–577
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trivedi, A., Waters, K., Suresh, S. et al. Congenital central hypoventilation syndrome: four families. Sleep Breath 15, 785–789 (2011). https://doi.org/10.1007/s11325-010-0439-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0439-z