Abstract
Purpose
To determine the effects of spousal involvement on continuous positive airway pressure (CPAP) adherence and response to CPAP problems in male patients with obstructive sleep apnea (OSA).
Methods
Wives’ involvement (pressure, support, and collaboration), CPAP adherence and CPAP problems (e.g., mask leaks) were assessed for 10 days in 31 male OSA patients. Disease severity and pre-treatment ratings of relationship quality were tested as moderators of daily associations in multilevel models. Effects of wives’ involvement were tested as predictors of day-to-day adherence and average nightly adherence at 3 months.
Results
Perception of wives’ support predicted increased adherence only in patients with high disease severity. Collaboration increased following nights with lower adherence and greater CPAP problems. Patients with lower conflict in the relationship reported a greater increase in collaboration associated with CPAP problems. Patients with lower support in the relationship reported increased next-day support following nights with CPAP problems. Perceived pressure from the wife was not associated with increased adherence in day-to-day analyses and associated with poorer adherence at 3 months.
Conclusions
The relationship between wives’ involvement and adherence was bidirectional and influenced by disease and relationship context. The majority of findings demonstrated increased positive wife involvement as a reaction to adherence and problems with CPAP. Supportive and collaborative interventions have the potential to improve CPAP adherence and response to CPAP-related problems, particularly in patients with high disease severity. Pressure to use CPAP from the wife was not beneficial for adherence that day and predicted poorer adherence at 3 months. Further research is needed to test supportive spousal involvement as an adherence intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Obstructive sleep apnea (OSA) is a condition characterized by repeated pauses or reductions in breathing and excessive daytime sleepiness. Treatment of this disorder is important due to the association between OSA and coronary heart disease [1], hypertension [2], insulin resistance [3], depression [4, 5], and poor quality of life [6]. The characteristic symptoms of OSA (i.e., snoring, sleepiness, irritability, and depressive symptoms) are often problematic for relationship and family functioning [7]. Continuous positive airway pressure (CPAP) improves daytime sleepiness [8], mood [9], and reduces risk for coronary events [10, 11]. Patients and partners report decreased sleepiness and improved psychosocial, relationship quality [12–14], and objective sleep quality [15, 16] when treated with CPAP. However, despite the benefits of CPAP, 46-83% of patients is non-adherent [17, 18].
Little is known regarding the role of marital and family factors in CPAP use. One study reported that patients who slept with a bed partner had higher adherence during the first week of CPAP treatment than patients without a bed partner [19]. However, two studies suggest that spousal influence may not always improve CPAP use. In a study of male OSA patients over the first 3 months of CPAP treatment, marital conflict predicted poorer adherence [20]. Another study found that patients who reported seeking treatment due to their spouse, versus being self-referred, demonstrated lower CPAP adherence over the first 3 months of treatment [21]. These studies suggest there may be both positive and negative aspects of relationships for CPAP adherence.
There is a large literature that demonstrates that support, particularly from a marital partner is associated with better health and health behavior [22–26]. Married individuals have healthier behaviors [27–30] and higher healthcare utilization [31] compared with unmarried and never-married individuals. For patients coping with a chronic health problem, spouses are frequently described as the greatest source of social support for both the physical and emotional aspects of the illness [32–35]. Marital quality and family support have been associated with adherence to medical treatments for a wide variety of conditions including post-surgical recommendations in cardiac patients [36, 37], hemodialysis in end-stage renal disease [38, 39], medication adherence [40], and self-care behaviors in type II diabetes [41, 42].
Much of the benefits of marriage have been attributed to support, but interpersonal dynamics of marriage also include pressure and control, which also may also promote health behaviors [29]. The term health-related social control refers to pressure from the social network, such as a spouse, to have better health behavior [27, 43]. This pressure may be applied directly, through words and action, or indirectly, through the individual’s desire to fulfill role obligations. Control or pressure tactics, when viewed as positive and collaborative, have been related to better health behaviors or desire to improve health behaviors [30, 43–46]. On the other hand, pressure may lead to negative effects such as increased distress and loss of autonomy when viewed as nagging or critical [27, 45, 47–49].
In addition to the type of involvement (support or control), another important area to consider in studying spousal involvement is context, including relationship and severity of disease. Pressure from the partner may not have the same impact in the context of a discordant relationship. In a study of patients recovering from total knee replacement, positive social control tactics (e.g., encouragement to engage in post-surgical recommendations) only predicted improved health behavior in couples with low levels of dismissive behavior [50]. Disease severity has not been extensively studied but it is possible that spousal involvement may operate differently when the patient has greater symptoms or disability.
In summary, despite the benefits of CPAP to patient and spouse, little is known about how spouses are involved in this treatment or the impact of spousal involvement on adherence. To date, no study has examined spousal involvement in CPAP beyond patient perceptions of pressure to seek treatment. The purpose of this study was to evaluate the effects of wives’ support and control on CPAP adherence in patients with OSA. Pressure from the wife was conceptualized as direct actions by the wife aimed at influencing behavior (e.g., asking, providing reminders, persuasion to use CPAP). Two types of supportive behavior were evaluated: support (e.g., feeling supported for using CPAP) and collaboration (e.g., helping solve problems with CPAP, helping with the CPAP machine). We hypothesized that positive wife involvement (support and collaboration) would be associated with higher adherence but negative wife involvement (e.g., pressure) would be unrelated to adherence or associated with poorer adherence. We also predicted that lower adherence and greater problems with CPAP would precipitate an increase in wife involvement. We tested pre-treatment ratings of relationship quality (i.e., support and conflict) and the Apnea-Hypopnea Index (AHI), the standard objective measure of OSA severity, as moderators of the effects of wife involvement on adherence and affect. Relationship quality was chosen because wife influence may be more effective in the context of a high support and low-conflict relationship. AHI was chosen as a moderator because it is related to severity of symptoms [51, 52].
Methods
Participants
Participants included male patients 65 years of age or younger who were married or cohabiting for ≥1 year, newly diagnosed with OSA, and had never used CPAP. Participants were recruited consecutively from August 2005 to April 2006. We limited our sample to male participants due to significant gender differences in spousal involvement [30, 53]. Exclusionary criteria included the following conditions that may affect the treatment of sleep apnea: chronic obstructive pulmonary disease, supplemental oxygen therapy, congestive heart failure, cardiomyopathy, and psychosis. This study was approved by the University of Utah IRB and participants provided written informed consent.
Procedure
Participants completed baseline questionnaires after OSA diagnosis prior to undergoing CPAP titration. Research assistants discussed study procedures and provided study materials at the sleep laboratory. This study utilized a daily questionnaire to test the association between three types of wife involvement (pressure, emotional support, and collaboration) on adherence. This methodology allowed measurement of wife involvement closer to the event and the outcome, thereby reducing recall bias and allowing some ability to test the directionality of the relationship from day to night [54, 55]. Participants were instructed to complete daily questionnaires at bedtime, without the help of their wife and place them in the mail the next day in pre-stamped, pre-addressed envelopes. We chose to administer the daily questionnaire once per day in order to minimize participant burden and thus increase adherence to the questionnaire. The time of administration (evening) was chosen to allow participants to complete questionnaires closer to occurrences of wife involvement in treatment (which are more likely during the day and at bedtime, such as setting up the CPAP for the night). Participants began completing daily questionnaires within 1 week of receiving the CPAP machine in their home (M = 4.45, SD = 6.06 days). Research assistants called participants every other day to prompt completion of diaries and answer questions. Daily questionnaires were verified by postmark and in situations when participants returned diaries late, researcher assistants called to assess when they were completed.
Measures
Sample characteristics
Demographics
Participants completed a demographic questionnaire that included age, race/ethnicity, marital status, income, and employment status.
Medical history
Weight, height, and medications, and medical co-morbidities were obtained through review of medical records. Body mass index (BMI) was calculated as kg/m2. Records from follow-up visits were examined to determine if problems with CPAP or poor adherence were identified at follow-up visits. BMI, medical history, and information regarding mask changes and pressure changes were available for all 31 participants. Reports of treatment side effects (e.g., mask leaks and awakenings) were available for 24 participants.
Daily measures
Spousal involvement
Eight items were administered to measure wife involvement in CPAP. Items were drawn from a validated measure based on frequency of use in other health behaviors and applicability to CPAP, and item content was adapted to focus on CPAP use [56]. Participants rated the extent to which their wife engaged in the behaviors during the past day on a scale from 1 (not at all) to 5 (extreme). The three subscales were derived from these items using principle components analysis with Varimax rotation based on items from the first questionnaire day: pressure (asked about using CPAP, tried to persuade you to use CPAP, dropped hints about using CPAP), collaboration (helped solve a problem with CPAP, helped with the CPAP machine), and support (felt supported for using CPAP). Two items were excluded from the subscales: felt criticized about CPAP, which was excluded due to low frequency, and made jokes to get you to use CPAP, which loaded on more than one factor. Internal consistency was adequate for pressure (0.811) and collaboration (0.867). Support for CPAP was only measured by one item; therefore, internal consistency was not calculated.
Problems with CPAP were assessed by one item, “Last night, to what extent did you have problems with CPAP (e.g., mask leaks, stuffy nose, awakenings)?” This item was rated from 1 (none) to 5 (severe).
Contextual variables
Disease severity
Disease severity was measured by AHI which is calculated by dividing the number of apneas and hypopneas by the total hours of sleep during the diagnostic PSG.
Relationship quality
General ratings of relationship quality were measured by the Quality of Relationship Inventory [57] support and conflict subscales. The seven-item support subscale contained items related to emotional support in the marriage, such as “To what extent could you count on your spouse for advice about a problem?” The 12-item conflict subscale contained items related to the frequency and extent of marital conflict, such as, “How angry does your spouse make you feel?” The QRI demonstrated good internal consistency for both subscales in this study (Cronbach’s alpha = 0.85 for the support subscale, Cronbach’s alpha = 0.89 for the conflict subscale).
Adherence
Adherence was measured as hours of self-reported adherence per night. Average self-report adherence over the 10-day questionnaire period was excellent (M = 5.96; SD = 1.51 h/night). Participants were notified in the informed consent procedures that objective adherence data would be collected to allow for comparison of self-report and objective data. A memory card located in the CPAP apparatus recorded the number of minutes per night CPAP machine was turned on at the appropriate pressure with the mask in place for 16 participants, as not all machines were capable of collecting this information. There was a moderate to high correlation between self report and objective adherence reports (r(14) = 0.64, p < 0.001 comparing each night of self-report and objective adherence, r(14) = 0.79, p < 0.001 comparing the average of the 10-day period for self-report and objective adherence).
Data analysis
Descriptive analyses of daily tactic use and correlations were conducted using SPSS v15.0 (SPSS Inc., Chicago, IL, USA). Data from the daily questionnaires were analyzed using Hierarchical Linear Modeling [58] with ten observations nested within each individual. This program interpolates missing data under the assumption that it is missing at random [59]. The majority of the 31 participants completed all ten daily questionnaires (71%). All participants completed at least two diaries. Only six diaries (2%) were excluded due to late return or illegibility. There were no missing data for moderator (level 2) variables. Statistical significance was defined as p < 0.05 using two-tailed tests.
Statistical model
The hierarchical structure of the data allowed tests of both within (level 1) and between (level 2) subject effects. In the models, questionnaire day was entered as an uncentered variable, with day 1 scaled as zero. All other level 1 independent variables were centered around each individual patient’s mean (group mean or person centering) and level 2 variables were centered around the grand mean [60]. This method of centering tested the question “Do participants report higher than their own average levels of adherence on days when they report higher than their own average levels of wife involvement?” At level 2, we asked the question “Do individuals with a high AHI report a stronger relationship between wife involvement and adherence the following night?” We tested three sets of models: (1) wife involvement as a predictor of change in adherence that night, (2) daily adherence as a predictor of next-day wife involvement, and (3) daily problems with CPAP as a predictor of next-day wife involvement. Day (1-10) and prior day adherence or wife involvement were included as covariates in all models.
In models with significant variability in the day-to-day within-person effects (level 1), the moderators, relationship quality (support and conflict) and AHI, were entered in level 2. Both positive (support) and negative (conflict) aspects of relationship quality were tested in separate level 2 because support and conflict are important but separate predictors of marital satisfaction, health, and health behavior [57, 61]. Estimates reported are unstandardized coefficients and can be interpreted similar to B coefficients in multiple regression analyses.
Results
Participant characteristics
Forty-two participants initially enrolled in the study and 31 participants completed the daily questionnaire. Participant characteristics are listed in Table 1. On average, participants were middle-aged, married, and identified their race/ethnicity as Caucasian. Average length of marriage was 20.1 (SD = 11.3) years. Ratings of relationship quality were comparable to other reported means from men in romantic relationships [62]. Average AHI was severe. Reasons for dropout after initial questionnaires were unknown but participants who initially enrolled but did not complete the daily diaries were slightly younger (M = 39.8, SD = 12.4 years, p < 0.05) and were less likely to have mask problems reported in medical records. Participants who completed daily diaries did not differ based on disease severity, BMI, adherence, or other aspects of treatment or side effects.
Frequency and amount of spousal involvement
Descriptive statistics for spousal involvement is listed in Table 2. The most frequent and highest rating of wife involvement was support, with 94% reported feeling supported by their wife to use CPAP on at least 1 day of the 10-day period. Collaboration and pressure were less common. Only 13% of participants did not report any wife involvement.
Correlations between spousal involvement, relationship quality, and adherence
Table 3 contains correlations between daily ratings of wife involvement, general ratings of relationship quality, disease severity, and adherence (self-report at day 10 and objective adherence at 3 months). Support for CPAP was positively associated with collaboration, general levels of support in the relationship, and negatively associated with general levels of conflict in the relationship. Collaboration and pressure were not associated with general ratings of support or conflict in the relationship. Pressure from the wife to use CPAP was negatively correlated with objective adherence at 3 months.
Predictors of daily CPAP adherence
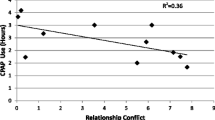
There was a trend toward increased adherence on nights following days that participants reported higher collaboration (β = 0.19, SE = 0.10, p = 0.06). Daily pressure and support did not predict CPAP adherence but variance components were significant for these models. In level 2 analyses, AHI moderated the relationship between support and adherence (γ = 0.02, SE = 0.01, p < 0.05) which indicated a CPAP use increased following days with higher support only among participants with higher AHI (Fig. 1). Level 2 variables were not significant for models of pressure and adherence.
Predictors of next-day wife involvement
Collaboration increased following nights with lower adherence (β = −0.12, SE = 0.05, p < 0.05). The variance component for this model was significant, but no variables were significant at level 2. Adherence did not predict next-day wife pressure or support. The variance component was significant for the model of next-day support but there were no significant variables at level 2.
CPAP problems and change in next-day wife involvement
CPAP problems were associated with higher next-day collaboration (β = 0.18, SE = 0.07, p < 0.05). The variance component was significant for this model. There was a significant level 2 effect for relationship conflict (β = 0.20, SE = 0.07, p < 0.05), indicating that participants with lower relationship conflict demonstrated a greater increase in next-day collaboration following nights with CPAP problems (Fig. 2). Daily support was not associated with CPAP problems but the variance component was significant for this model. Relationship support moderated the relationship between CPAP problems and next-day support for CPAP (γ = −0.04, SE = 0.02, p < 0.05). Participants with lower ratings of overall ratings of support in the relationship reported an increase in daily support for CPAP following nights with higher CPAP problems whereas participants with high relationship support did not report an increase in support.
Discussion
This study is the first investigation of the role of wife support and pressure in CPAP treatment. We utilized a daily questionnaire to study the bi-directional relationships between involvement from the wife (pressure, support, and collaboration) and nightly CPAP adherence. This study also provided descriptive information about wives’ involvement with CPAP in patients beginning CPAP treatment. We found that nearly all participants in our study reported wife involvement on at least one of the 10 days early in treatment. Even for the least common type of wife involvement, pressure, 63% of participants reported experiencing this on at least 1 day. However, the mean levels of wife involvement were fairly low. This suggests that wife involvement is common but not high in intensity.
A summary of our findings from the daily analyses is presented in Fig. 3. We hypothesized that wife involvement would be associated with higher adherence and that contextual factors (AHI, relationship support, and relationship conflict) would be important to understanding these associations. Overall, we found a small amount of evidence that wife involvement measured in this study was associated with increased adherence that night. There was greater evidence pointing in the opposite direction, that changes in wife involvement were a response to adherence and problems with adherence.
The finding that support was associated with higher adherence in participants with high AHI was consistent with our prediction that wife involvement would be beneficial to adherence. A wide variety of studies in many health conditions have found social support (emotional, instrumental) to be associated with better adherence [63]. In this study, it is possible that participants with lower AHI had lower levels of daytime sleepiness and daytime functional impairment, and thus were less likely to report subjective benefits from treatment [64, 65]. Therefore, it is possible that providing support, even if meant to be helpful, may have been viewed as unhelpful and lead to ignoring the request [66, 67].
In analyses of changes in wife involvement in response to adherence, we found that patients reported increased collaboration from their wives following nights with lower adherence. This may be due to the wives’ sleep disruption due to the non-adherent patient. In addition, participants experience an increase in daytime sleepiness and decrease in cognitive function after even 1 night without CPAP, which may increase the involvement of the wife if they notice a change in patient behavior [68, 69].
We also found interesting results regarding wives’ next-day response to problems with CPAP. Our finding that participants with low relationship conflict reported a greater increase in next-day collaboration (such as helping with the CPAP machine) following nights with CPAP problems suggests patients in low conflict marriages may have wives who are more involved with ironing out initial issues with treatment. One of our prior studies demonstrated lower adherence in patients with higher relationship conflict [20]. This may point to a mechanism by which marital conflict interferes with adherence. Responses to CPAP problems are important because the majority of patients report having initial problems with CPAP in the beginning that need to be worked through (e.g., mask fit) [70]. Many of the early problems can be remedied with technical changes (e.g., mask adjustment and pressure changes). It should also be noted that relationship quality impacts recall and interpretation of marital interactions [71, 72]. Patients in higher conflict relationships may have viewed this behavior as “miscarried helping” or “overprotectiveness”, and therefore not reported increased collaboration [73, 74].
It is also interesting that participants with low support in the relationship reported increased support for CPAP associated with CPAP problems. This increase in support may be beneficial for some patients, as we found that support increased adherence in patients with high AHI. In addition, it is possible that there was a ceiling effect for wives’ support for CPAP in participants who already had high support in the relationship.
We did not find that pressure from the wife to use CPAP increased adherence, and it is possible that it may have even interfered with adherence. In correlations between spousal involvement and adherence at 3 months, higher daily pressure early in CPAP treatment was associated with lower adherence at 3 months. This type of pressure may not impact proximal reactions to adherence but if high levels continue, it may contribute to decreased adherence over time due to reactance [75]. In one prior study, patients who reported seeking treatment due to their spouse versus being self-referred demonstrated lower CPAP adherence over the first 3 months of treatment [21].
Findings from our study are limited by aspects of our sample and methodology. The greatest limitation is the use of self-report rather than objective adherence. Future studies should confirm these results with objective findings. In addition, the measures of wives’ involvement used in this study were adapted from a questionnaire for general health behaviors, and may not have been the most relevant types of involvement for CPAP use. Qualitative research may be helpful in future studies to determine the most relevant types of involvement. In addition, future research should aim to include reports from both patient and spouse, as there have been differences demonstrated based on surveys of the target vs. provider of support and pressure. For example, Lewis and colleagues [56] found that wives’ but not husbands’ perceptions of spousal involvement were related to husbands’ reports of health behavior. Furthermore, future research should also include greater gender and ethnic diversity. OSA is present in approximately 2% of the middle-age female population; due to the presence of significant gender differences in spousal involvement, it should not be assumed that results from male patients can be generalized to female patients [53, 56, 67, 76]. There is also a need to explore these processes in more diverse race/ethnic samples as OSA prevalence is up to three times higher in middle-aged African Americans [77, 78].
In conclusion, this study demonstrates that the majority of patients beginning CPAP report wife involvement in CPAP treatment but daily levels are generally low. There was some evidence that support from the wife was associated with increased CPAP adherence, but this was only true for patients with high AHI. There was greater support for changes in wife involvement as a reaction to adherence and problems with CPAP. These results demonstrate enhancing spousal involvement in treatment in a way that increases patient perceptions of support for CPAP may aid in adherence and response to treatment-related problems, particularly for patients with greater disease severity. However, high levels of relationship conflict may interfere with collaboration in response to treatment problems. It may be helpful to reduce pressure from the spouse, as this was associated with poorer adherence at 3 months. Future research is warranted to determine if increasing spousal support and collaboration can be an effective intervention to improve CPAP adherence.
References
Malhotra A, White DP (2002) Obstructive sleep apnoea. Lancet 360(9328):237–245
Logan AG, Tkacova R, Perlikowski SM, Leung RS, Tisler A, Floras JS et al (2003) Refractory hypertension and sleep apnoea: effect of CPAP on blood pressure and baroreflex. Eur Respir J 21(2):241–247
Punjabi NM, Sorkin JD, Katzel LI, Goldberg AP, Schwartz AR, Smith PL (2002) Sleep-disordered breathing and insulin resistance in middle-aged and overweight men. Am J Respir Crit Care Med 165(5):677–682
Bardwell WA, Berry CC, Ancoli-Israel S, Dimsdale JE (1999) Psychological correlates of sleep apnea. J Psychosom Res 47(6):583–596
Vandeputte M, de Weerd A (2003) Sleep disorders and depressive feelings: a global survey with the Beck depression scale. Sleep Med 4(4):343–345
Goncalves MA, Paiva T, Ramos E, Guilleminault C (2004) Obstructive sleep apnea syndrome, sleepiness, and quality of life. Chest 125(6):2091–2096
Reishtein JL, Pack AI, Maislin G, Dinges DF, Bloxham TJ, George CF et al (2006) Sleepiness and relationships in obstructive sleep apnea. Issues Ment Health Nurs 27(3):319–330
Patel SR, White DP, Malhotra A, Stanchina ML, Ayas NT (2003) Continuous positive airway pressure therapy for treating sleepiness in a diverse population with obstructive sleep apnea: results of a meta-analysis. Arch Intern Med 163(5):565–571
Means MK, Lichstein KL, Edinger JD, Taylor DJ, Durrence HH, Husain AM et al (2003) Changes in depressive symptoms after continuous positive airway pressure treatment for obstructive sleep apnea. Sleep Breath 7(1):31–42
Marin JM, Carrizo SJ, Vicente E, Agusti AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365(9464):1046–1053
Doherty LS, Kiely JL, Swan V, McNicholas WT (2005) Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest 127(6):2076–2084
Doherty LS, Kiely JL, Lawless G, McNicholas WT (2003) Impact of nasal continuous positive airway pressure therapy on the quality of life of bed partners of patients with obstructive sleep apnea syndrome. Chest 124(6):2209–2214
McFadyen TA, Espie CA, McArdle N, Douglas NJ, Engleman HM (2001) Controlled, prospective trial of psychosocial function before and after continuous positive airway pressure therapy. Eur Respir J 18(6):996–1002
Parish JM, Lyng PJ (2003) Quality of life in bed partners of patients with obstructive sleep apnea or hypopnea after treatment with continuous positive airway pressure. Chest 124(3):942–947
Beninati W, Harris CD, Herold DL, Shepard JW Jr (1999) The effect of snoring and obstructive sleep apnea on the sleep quality of bed partners. Mayo Clin Proc 74(10):955–958
Cartwright RD (2008) Sleeping together: a pilot study of the effects of shared sleeping on adherence to CPAP treatment in obstructive sleep apnea. J Clin Sleep Med 4(2):123–127
Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: the challenge to effective treatment. Proc Am Thorac Soc 5(2):173–178
Engleman HM, Wild MR, Weaver TE, Maislin G, Dinges DF, Younger J et al (2003) Improving CPAP use by patients with the sleep apnoea/hypopnoea syndrome (SAHS). Sleep Med Rev 7(1):81–99
Lewis KE, Seale L, Bartle IE, Watkins AJ, Ebden P (2004) Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep 27(1):134–138
Baron KG, Smith TW, Czajkowski LA, Gunn HE, Jones CR (2009) Relationship quality and CPAP adherence in patients with obstructive sleep apnea. Behav Sleep Med 7(1):22–36
Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ (1999) Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med 159(4 Pt 1):1096–1100
Kiecolt-Glaser JK, Newton TL (2001) Marriage and health: his and hers. Psychol Bull 127(4):472–503
Uchino BN (2006) Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med 29(4):377–387
Berkman LF, Syme SL (1979) Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol 109(2):186–204
Berkman LF, Glass T, Brissette I, Seeman TE (2000) From social integration to health: Durkheim in the new millennium. Soc Sci Med 51(6):843–857
House JS, Landis KR, Umberson D (1988) Social relationships and health. Science 241(4865):540–545
Hughes M, Gove WR (1981) Living alone, social integration, and mental health. Am J Sociol 87(1):48–74
Wickrama K, Conger RD, Lorenz FO (1995) Work, marriage, lifestyle, and changes in men's physical health. J Behav Med 18(2):97–111
Umberson D (1987) Family status and health behaviors: social control as a dimension of social integration. J Health Soc Behav 28(3):306–319
Umberson D (1992) Gender, marital status and the social control of health behavior. Soc Sci Med 34(8):907–917
Kaplan RM, Kronick RG (2006) Marital status and longevity in the United States population. J Epidemiol Community Health 60(9):760–765
Revenson TA, Kayser K, Bodenmann G (2005) Couples coping with stress: emerging perspectives on dyadic coping. American Psychological Association, Washington
Lyons RF, Mickelson KD, Sullivan MJ, Coyne JC (1998) Coping as a communal process. J Epidemiol Community Health 15(5):579–605
Manne S (1994) Couples coping with cancer: research issues and recent findings. J Clin Psychol Med Settings 1(4):317–330
Berg CA, Upchurch R (2007) A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol Bull 133(6):920–954
Kulik JA, Mahler HI (2006) Marital quality predicts hospital stay following coronary artery bypass surgery for women but not men. Soc Sci Med 63(8):2031–2040
Bastone EC, Kerns RD (1995) Effects of self-efficacy and perceived social support on recovery-related behaviors after coronary artery bypass graft surgery. Ann Behav Med 17(4):324–330
Christensen AJ, Smith TW, Turner CW, Holman JM et al (1992) Family support, physical impairment, and adherence in hemodialysis: an investigation of main and buffering effects. J Behav Med 15(4):313–325
Christensen AJ, Ehlers SL (2002) Psychological factors in end-stage renal disease: an emerging context for behavioral medicine research. J Consult Clin Psychol 70(3):712–724
Doherty WJ, Schrott HG, Metcalf L, Iasiello-Vailas L (1983) Effect of spouse support and health beliefs on medication adherence. J Fam Pract 17(5):837–841
Trief PM, Morin PC, Izquierdo R, Teresi J, Starren J, Shea S et al (2006) Marital quality and diabetes outcomes: the IDEATel project. Fam Syst Health 24(3):318–331
Trief PM, Ploutz-Snyder R, Britton KD, Weinstock RS (2004) The relationship between marital quality and adherence to the diabetes care regimen. Ann Behav Med 27(3):148–154
Rook KS, Thuras PD, Lewis MA (1990) Social control, health risk taking, and psychological distress among the elderly. Psychol Aging 5(3):327–334
Lewis MA, Butterfield RM (2005) Antecedents and reactions to health-related social control. Pers Soc Psychol Bull 13(3):416–427
Lewis MA, Rook KS (1999) Social control in personal relationships: impact on health behaviors and psychological distress. Health Psychol 18(1):63–71
Tucker JS, Anders SL (2001) Social control of health behaviors in marriage. Am J Respir Crit Care Med 31(3):467–485
Krause N, Goldenhar L, Liang J, Jay GM et al (1993) Stress and exercise among the Japanese elderly. Soc Sci Med 36(11):1429–1441
Thorpe CT, Lewis MA, Sterba KR (2008) Reactions to health-related social control in young adults with type 1 diabetes. J Behav Med 31:93–103
Stephens MAP, Fekete EM, Franks MM, Rook KS, Druley JA, Greene K (2009) Spouses' use of pressure and persuasion to promote osteoarthritis patients' medical adherence after orthopedic surgery. Health Psychol 28(1):48–55
Fekete EM, Stephens MA, Druley JA, Greene KA (2006) Effects of spousal control and support on older adults' recovery from knee surgery. J Fam Psychol 20(2):302–310
Gay P, Weaver T, Loube D, Iber C, Positive Airway Pressure Task F, Standards of Practice C et al (2006) Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep 29(3):381–401
Gottlieb DJ, Whitney CW, Bonekat WH, Iber C, James GD, Lebowitz M et al (1999) Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Respir Crit Care Med 159(2):502–507
Westmaas JL, Wild TC, Ferrence R (2002) Effects of gender in social control of smoking cessation. Health Psychol 21(4):368–376
Bolger N, Davis A, Rafaeli E (2003) Diary methods: capturing life as it is lived. Annu Rev Psychol 2003(54):579–616
West SG, Hepworth JT (1991) Statistical issues in the study of temporal data: daily experiences. J Pers 59(3):609–662
Lewis MA, Butterfield RM, Darbes LA, Johnston-Brooks C (2004) The conceptualization and assessment of health-related social control. J Soc Pers Relatsh 21(5):669–687
Pierce GR, Sarason IG, Sarason BR (1991) General and relationship-based perceptions of social support: are two constructs better than one? J Pers Soc Psychol 61(6):1028–1039
Raudenbush SW, Bryk AS, Congdon R (2007) Hierarchical linear modeling 6.04 ed. Scientific software international, Lincolnwood, IL
Bryk AS, Raudenbush SW (1992) Hierarchical linear models: applications and data analysis methods. Sage, Newbury Park
Kreft IGG, de Leeuw J, Aiken LS (1995) The effect of different forms of centering in hierarchical linear models. Multivariate Behav Res 30(1):1–21
Mattson RE (2006) The longitudinal course of positive and negative relationship quality. Dissertation Abstracts International: Section B: The Sciences and Engineering, 67
Verhofstadt LL, Buysse A, Rosseel Y, Peene OJ (2006) Confirming the three-factor structure of the quality of relationships inventory within couples. Psychol Assess 18(1):15–21
DiMatteo MR (2004) Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol 23(2):207–218
Marshall NS, Neill AM, Campbell AJ, Sheppard DS (2005) Randomised controlled crossover trial of humidified continuous positive airway pressure in mild obstructive sleep apnoea. Thorax 60(5):427–432
Lindberg E, Berne C, Elmasry A, Hedner J, Janson C (2006) CPAP treatment of a population-based sample—what are the benefits and the treatment compliance? Sleep Med 7(7):553–560
Tucker JS, Mueller JS (2000) Spouses' social control of health behaviors: use and effectiveness of specific strategies. Pers Soc Psychol Bull 26(9):1120–1130
Tucker JS, Orlando M, Elliott MN, Klein DJ (2006) Affective and behavioral responses to health-related social control. Health Psychol 25(6):715–722
Kribbs NB, Pack AI, Kline LR, Getsy JE, Schuett JS, Henry JN et al (1993) Effects of one night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnea. Am Rev Respir Dis 147(5):1162–1168
Yang Q, Phillips CL, Melehan KL, Rogers NL, Seale JP, Grunstein RR (2006) Effects of short-term CPAP withdrawal on neurobehavioral performance in patients with obstructive sleep apnea. Sleep 29(4):545–552
Engleman HM, Asgari-Jirhandeh N, McLeod AL, Ramsay CF, Deary IJ, Douglas NJ (1996) Self-reported use of CPAP and benefits of CPAP therapy: a patient survey. Chest 109(6):1470–1476
Hawkins MW, Carrere S, Gottman JM (2002) Marital sentiment override: does it influence couples' perceptions? J Marriage Fam 64(1):193–201
Notarius CI, Benson PR, Sloane D, Vanzetti NA (1989) Exploring the interface between perception and behavior: an analysis of marital interaction in distressed and nondistressed couples. Behav Assess 11(1):39–64
Coyne JC, Wortman CB, Lehman DR (1988) Marshaling social support. In: Gottlieb BH (ed) Formats, processes, and effects., p 337
Kuijer RG, Ybema JF, Buunk BP, De Jong GM, Thijs-Boer F, Sanderman R (2000) Active engagement, protective buffering, and overprotection: three ways of giving support by intimate partners of patients with cancer. J Soc Clin Psychol 19(2):256–275
Brehm JW (1966) A theory of psychological reactance. Academic Press, New York
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235
O'Connor GT, Lind BK, Lee ET, Nieto FJ, Redline S, Samet JM et al (2003) Variation in symptoms of sleep-disordered breathing with race and ethnicity: the sleep heart health study. Sleep 26(1):74–79
Kripke DF, Ancoli-Israel S, Klauber MR, Wingard DL, Mason WJ, Mullaney DJ (1997) Prevalence of sleep-disordered breathing in ages 40–64 years: a population-based survey. Sleep 20(1):65–76
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors note
This study was funded in part by an APA Division 38 Health Psychology graduate student research award and by the University of Utah Sleep Wake Center. The authors thank the physicians and staff at the University of Utah Sleep Wake Center for their assistance in data collection, including Dr. Robert Simpson, Rick Pointer, and Thi-ly Downing.
Rights and permissions
About this article
Cite this article
Baron, K.G., Smith, T.W., Berg, C.A. et al. Spousal involvement in CPAP adherence among patients with obstructive sleep apnea. Sleep Breath 15, 525–534 (2011). https://doi.org/10.1007/s11325-010-0374-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0374-z