Abstract
Purpose
The aim of this study was to investigate the time course of body weight, daytime sleepiness, and functional cardiorespiratory parameters in patients with both chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea syndrome (OSA), after institution of domiciliary nasal continuous positive airway pressure (nCPAP).
Methods
Twelve consecutive obese outpatients (mean age = 61 ± 11 years; four women) were evaluated before (baseline) and after 3, 12, and 24 months of nocturnal nCPAP (4 h per night).
Results
At baseline, all patients were hypercapnic and hypoxemic, suffering from night desaturation (T 90 is the percentage of total recording time (TRT) spent with SaO2 ≤ 90% = 38 ± 2%) and sleepy (Epworth sleepiness scale [ESS] = 16.58 ± 0.86). Three months after the implementation of nCPAP, daytime PaCO2 and PaO2 improved up to 45.1 ± 0.9 and 69.0 ± 1 mmHg, respectively; mean pulmonary artery pressure (MPAP) decreased from 24.7 ± 1.1 to 19.2 ± 04 mmHg. All other variables showed progressive improvements up to 12 months. At 3 and 12 months, mean body mass index was slightly decreased (to 31.6 ± 0.2 and 30.7 ± 0.1 kg/m2, respectively); daytime sleepiness, nocturnal O2 desaturation, and maximal inspiratory pressure were also improved and thereafter remained stable.
Conclusions
In conclusion, in our patients with both severe OSA and mild-to-moderate COPD, arterial blood gasses and MPAP improved and stabilized after 3 months of nCPAP therapy, with the greatest improvements being in ESS score, T 90, and maximal inspiratory force from 3 up to 12 months; these parameters remained stable over the following 12 months. Finally, our data support early treatment with nCPAP in such patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea–hypopnea syndrome (OSA) are both common diseases affecting, respectively, 10% and 5% of the adult population over 40 years of age, and their coexistence, which is defined as overlap syndrome, can be expected to occur in about 0.5% of this population. Moreover, the prevalence of OSA is not higher in COPD than in the general population [1].
Patients with coexisting COPD and sleep apnea typically develop more severe oxygen desaturation during sleep and also are at a higher risk of developing respiratory insufficiency than pure OSA patients [2].
In patients with overlap syndrome, hypoxemia, hypercapnia, and pulmonary hypertension can be observed in the presence of mild to moderate bronchial obstruction, which is different from usual COPD.
OSA shares several important features with COPD, as follows: OSA affects 4–6% of all middle-aged males and 2% of middle-aged females, with percentages similar to COPD [3]; it is now appreciated by several well-controlled epidemiological studies that 20% of patients with OSA will have COPD [4]; moreover, 10% of OSA is disclosed in COPD patients independently of the degree of functional status, and in 63% of OSA patients, a history of smoking is recorded, which is a predisposing factor for both OSA and COPD [5].
Nasal continuous positive airway pressure (nCPAP) is considered the first-choice treatment for patients with OSA, inducing a reduction in nocturnal respiratory events, symptoms, and cardiovascular morbidity [6, 7].
Therapy of the overlap syndrome consists of nCPAP or nocturnal noninvasive ventilation (NIV) with or without associated nocturnal O2 therapy.
COPD is not only an inflammatory chronic disease of the airway and the lungs, but also involves systemic, cellular, and humoral inflammation, and inhaled cigarette smoke is the most important known causative factor [8].
Previous studies have evaluated the role of long-term noninvasive positive pressure ventilation (NPPV) in COPD, particularly during sleep, but have led to conflicting results [9, 10]. Continuous positive airway pressure (CPAP) has been shown to be effective in patients with COPD by decreasing the work of inspiration [11].
The use of nCPAP has also been shown to result in improvements in gas exchange, airflow obstruction, and hospitalization rates in patients with both COPD and sleep-disordered breathing (SDB) [12].
We hypothesized that, by successfully treating patients' severe OSA with nCPAP, their coexistent mild to moderate COPD would consequently improve. We excluded from our study patients with severe COPD requiring long-term oxygen therapy for ≥16/24 h.
The aim of this study was to assess the effect of regular treatment with nCPAP on ventilatory parameters in patients with severe OSA and mild to moderate COPD (overlap syndrome) at basal conditions and after 24 months of treatment.
Patients and methods
Patients
Demographic and clinical data were obtained from the medical chart. These data included: age, smoking status, apnea–hypopnea index (AHI), comorbidities mean and nadir oxygen saturation during the diagnostic sleep study, maximal inspiratory pressure (Pimax), body mass index (BMI), and mean pulmonary artery pressure (MPAP) at the time of the initiation of nCPAP therapy. Pulmonary function tests results and number of COPD exacerbation requiring an emergency room visit, hospitalization, or outpatient visit were obtained.
Inclusion criteria
Consecutive obese (BMI >30 kg/m2) patients suffering from both COPD and OSA were enrolled in the study from January 2005 to January 2007 at the Pneumology Department “A. Galateo” Hospital ASL Lecce (Italy) according to the following criteria: (1) All patients with COPD were diagnosed on the basis of the clinical history, physical examination, chest radiograph, and pulmonary function tests in accordance with the Global Initiative for Chronic Obstructive Lung Disease (GOLD) clinical criteria for the diagnosis and severity of COPD [13]; (2) all subjects were outpatients with stable COPD and with PaO2 >60 mmHg; (3) all patients had been free from acute exacerbations for at least 4 weeks, had stable awake compensated respiratory failure, and reported habitual snoring during the clinical interview; (4) absence of any significant respiratory, neuromuscular, or other disorder that could account for the hypercapnia; (5) AHI >30 events per hour of sleep. OSA was considered mild if AHI was ≥5 per hour but <15 per hour, moderate if ≥15 per hour but <30 per hour, and severe if ≥30 per hour; (6) the excessive daytime sleepiness was measured using the Epworth sleepiness scale (ESS).
Exclusion criteria
The exclusion criteria included: (1) outpatients with stable COPD and with PaO2 <60 mmHg; (2) patients with derangements in gas exchange due to any other causes were excluded, as well as patients with restrictive disease (e.g., kyphoscoliosis, diaphragmatic paralysis and diffuse interstitial fibrosis, bronchiectasis, fibrosis of the pleural space); (3) concurrent treatment with anxiolytics or analeptic drugs, and other associated chronic nonrespiratory diseases; and (4) patients with overlap syndrome who started the treatment with nCPAP, but showed a compliance of <3 h per night.
Patients were requested to give their informed consent for participating in the study and international ethical standards have been respected
Methods and measurements
Static lung volumes were measured by body plethysmographs (6200 Auto Box DL, Sensor Medics, Yorba Linda, CA, USA) and dynamic lung volumes by mass flow sensors with the patient in the seated position according to standard procedure. Normal values were those reported by the GOLD [13]. Arterial blood gasses were measured from the radial artery using microelectrodes (ABL 520-Radiometer, Copenhagen, Denmark) with the patient in the sitting position spontaneously breathing air.
Resting daytime mean MPAP was measured by means of color Doppler echocardiography (DE; GE Vingmend Ultrasound, Horten, Norway) using the subcostal approach [14]. The mean value of three measurements was considered.
Nocturnal desaturation was evaluated using polygraphic recordings (Poly-Mesam, MAP, and Martinsried, Germany) of pulsoximetry, snoring, air flow, thoracic and abdominal respiratory movements, heart rate including electrocardiography in real-time mode, and body position. Polygraphic recordings were performed between 11:00 p.m. and 6:00 a.m. The signals stored in a digital recorder were computer analyzed and then validated by a physician on the morning after the recording.
The definition of apnea and hypopnea was based on standard criteria. An obstructive apnea was defined as a reduction in airflow of >90%, lasting for at least 10 s, with evidence of persistent respiratory effort. A central apnea was defined as a reduction in airflow >90%, lasting for at least 10 s, without any evidence of respiratory effort. A hypopnea was defined as a reduction in airflow by 50%, with duration of at least 10 s [15].
Once the initial tests had been performed, if the patient was considered suitable for inclusion in the study, nCPAP (PV 10 i BREAS Medical AB, Fǒretagsvǎgen 1, SE-435 33 Mǒlnlycke, Sweden) via nasal mask was used. The device was provided by the calendar data analysis program and a storage capacity up to 4 years for patient compliance tracking. A commercially available nasal mask (Respironics Comfort Gel Nasal Mask, Minneapolis, MN, USA) was used in all the patients.
Nocturnal hypoxemia was defined as arterial oxygen saturation (SaO2) below 90% for at least 5 min with nadir saturation (NSaO2) of 85% or lower. Time spent in bed was defined as time from the start to the end of recording. T 90 % was defined as the percentage of total recording time (TRT%) spent in bed with SaO2 <90%. The minimal TRT% required for a satisfactory analysis of nocturnal recordings was 2 h [16].
Maximum inspiratory pressure (Pimax) was assessed with a calibrated manometer (in centimeters of H2O; 163 Sibelmed, Barcelona, Spain) at the functional residual capacity (FRC) level according to the method of Black and Hyatt [17]. For each patient, three to six measures were taken with the goal of obtaining the two measures with the highest values matching within 10%. The value reported are the best values obtained. Moreover, the subjective assessment of daytime sleepiness was carried out using the ESS score of 10 [18].
Treatment with nCPAP
Autotitration of nCPAP was performed by the Autoset® system, the characteristics of which have been previously described [19]. The pressure delivered to the patient was initially set at 4 cm H2O and gradually increased to a maximum of 20 cm H2O in response to detection, by a pneumotachograph, of apneas lasting more than 10 s, snoring, or modifications of the flow curve reflecting increased upper airways resistance. Conversely, the pressure was decreased when no abnormal respiratory event was detected. Automatic titration was performed at home during a second night of polysomnography according to the method described above.
The pneumotachograph was connected to the CPAP mask. The mask was adapted by the technician and repositioned during titration in the case of severe leaks, as detected by the Autoset®. The following morning, analyses of the polysomnography recording and reading of the titration report were used to evaluate the control of respiratory events by Autoset®, the severity of mask leaks, and the determination of pressure at the 95th percentile.
CPAP responders were defined as those patients who achieved a PaCO2 level of 45 mmHg, eliminating obstructive apneas, hypopnea, and flow limitation, with SaO2% persistently >90% during polysomnography, in order to address the variety of respiratory events observed during TRT.
The average number of hours and average pressure value of CPAP use was determined from the meter reading, detailing the hours of use and data setting on the CPAP device.
All subjects were prescribed nasal CPAP by mask by a pneumologist at the time of diagnosis and received an educational session provided by a pulmonary nurse specialist during the afternoon before the overnight polysomnography to familiarize themselves with the equipment and nasal mask [20].
Relative contraindications were: inability to protect airway, excessive airway secretion, need for continuous or nearly continuous ventilatory assistance, anatomic abnormalities that interfere with mask fitting, poorly motivated patient or close family, and inability to cooperate or comprehend.
Study protocol
Demographic and clinical data were obtained from medical charts for the 2 years preceding and the 2 years following the initiation of CPAP therapy. All patients were evaluated before (baseline) and after 3, 12, and 24 months of treatment with nCPAP, which was started in the hospital with a daytime adaptation period of 3 h.
Compliance with nCPAP therapy was defined as four or more hours of use per night. Lack of compliance or noncompliance was defined as an average yearly use of <3.5 h per night. Medical consultations were performed by phone at a frequency that varied according to the patient's clinical conditions. There was no “control” group.
The number of COPD exacerbations (AECOPD) was recorded. According to current definition, an exacerbation of COPD was defined as an event in the natural course of the disease characterized by a change in the patient's baseline dyspnea, cough, and/or sputum that is beyond normal day-to-day variations, is acute in onset, and may warrant a change in regular medication in a patient with underlying COPD [21]. All the patients received a pharmacological treatment according to the standards for the diagnosis and treatment of patients with COPD of the ATS/ERS [22]
The AECOPD requiring an outpatient visit, an emergency room visit, or hospitalization and the total number of days spent in hospital as a result of those exacerbations during the 2 years before and 2 years after starting CPAP therapy were calculated.
Statistical analysis
All statistical analyses were carried out using the Statgraphics© plus version 2.1 software (Statistical Graphics Corporation). Sample size was estimated on the basis of T 90 and ESS as primary endpoints, with a significance level of 5% and a power of 80%. As a first step, seven patients were evaluated at the beginning of the study and after 3 months, in order to calculate the means and standard deviations of T 90 and ESS. Treatment was judged effective if T 90 and ESS improvement was almost 50%. A final sample size of 12 patients was obtained by using the preliminary results of the first seven patients.
A Kolmogorov–Smirnov test was performed before data analysis in order to determine data distribution. This test documented that the entire variable was normally distributed and then we used parametric tests for the management of data. The studied variables were submitted to descriptive statistical analysis to obtain the distribution fitting and to calculate average, variance, standard error, range, standard skewness, and standard kurtosis. A table of the 95% confidence intervals (95%CI) with the mean of each variable was obtained to bind the sampling error in the estimates of such means. Values obtained from overlap syndrome patients at 0, 3, 12, and 24 months were analyzed by the Fisher's least significant difference multiple comparison procedure to determine which means are significantly different from each other.
The relationships of the patient variables were evaluated preliminarily by a table of Pearson product–moment correlations of pairs of variables followed by simple, as well as multiple, linear or nonlinear, regressions. The latter were carried out using the least-squares method in order to obtain the regression equations. Accuracy of the equations referred to bias and precision, with the bias defined as the mean difference between predicted and measured values and precision as the 95%CI for the difference. Values of p < 0.05 were considered as statistically significant.
Results
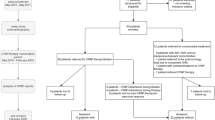
Twelve out of 25 patients met the inclusion criteria, presenting both moderate COPD and severe OSA. The remaining 13 patients were further excluded because of severe emphysema that invalidated echocardiographic estimates of pulmonary artery pressure [23]. The baseline characteristics of enrolled patients are summarized in Table 1.
In four patients, a heated humidifier was prescribed within the first days of treatment owing to nasal congestion and stuffiness secondary to nCPAP use. In these patients, the pressure setting was adjusted so that the mask pressure would match the prescribed value when using the humidifier circuit (Fisher & Paykel HC150, Heater Humidifier, Minneapolis, MN, USA). For all patients, the mean night use of nCPAP was 5.06 ± 0.14 h at 3 months, 5.15 ± 0.05 h at 12 months, and 5.08 ± 0.08 h at 24 months. The nCPAP pressure titration (in centimeters of H2O) was 12.67 ± 0.24 at 3 months, 12.54 ± 0.23 at 12 months, and 12.71 ± 0.22 at 24 months.
At the start of the study, all patients were hypercapnic and hypoxemic and presented severe values of both T 90 and ESS. PaCO2, PaO2, MPAP, and AHI showed improvements at 3 months, while no further changes were detected at 12 or 24 vs 3 months (Table 2).
All other variables showed a progressive improvement up to 12 months, with no further changes being observed from 12 to 24 months. Moreover, BMI slightly decreased at 3 and 12 months, whereas daytime sleepiness (ESS), nocturnal O2 desaturation (T 90), and MIP results greatly improved at 3 months as well as at 12 months, but their values as well as those of all mentioned variables (Table 2) showed no statistically significant changes between 12 and 24 months.
In particular, ESS showed a decrease by 71.35% (p = 0.0001), T 90 a decrease by 63.61% (p = 0.0002), Pimax an increase of 50% (p = 0.0005), PaCO2 a decrease of 29% (p = 0.0002), PaO2 an increase of 13.78% (p = 0.001), MPAP a decrease of 30% (p = 0.0001), FEV1 an increase of 15% (p = 0.0015), BMI a decrease of 11% (p = 0.0001), and FEV1/FVC an increase of 5.55% (p = 0.0012) at 24 months compared to the baseline values. No changes were detected regarding compliance and pressure of nCPAP from 3 to 24 months.
Two years after starting CPAP therapy, the numbers of total COPD exacerbations (per year), of total days in hospital (per year), and of outpatient visits (per year) were reduced (Fig. 1).
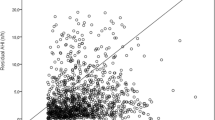
Factors influencing daytime sleepiness
Table 3 shows significant linear correlations identified by the least-squares method. The highest correlation was found between ESS and T 90%, Pimax, and PaCO2; this model explained 96% (R 2) of the ESS variability. Another strong correlation was found between ESS and T 90 alone explaining the 96% of the ESS variability, suggesting that daytime sleepiness may be caused mainly by nocturnal desaturation. Moreover, ESS was correlated with T 90 and PaCO2. Lastly, a significant correlation was found between T 90% and Pimax, the latter explaining the 71% of the T 90% variability.
Discussion
This study does not have a “control group” because all patients received nCPAP as indicated and recommended for the treatment of moderate to severe OSA according to the guideline of the American Academy of Sleep Medicine; moreover, the norms and the ethical principles standard hold the treatment necessary [24]
The standard for measuring pulmonary pressure has been right heart catheterization (RHC). Fisher et al. [23] have demonstrated that, in patients with severe emphysema (FEV1 < 45% and residual volume [RV] >200%), echocardiographic estimates of pulmonary artery pressure had a sensitivity of 60% and specificity of 74%. In this regard, it is important to highlight that the patient population of our study showed a significant lower degree of hyperinflation that has enabled us to get a measurement of MPAP. Transthoracic DE has become a common method to estimate pulmonary artery pressure noninvasively after several investigators showed good correlation with RHC in patient with pulmonary diseases [25].
Static and dynamic functional parameters, together with maximal respiratory pressure, are a measure of the respiratory muscular strength. In fact, in line with observations in COPD patients, we have observed similar decrease in Pimax and increase in FRC with the reduction of FEV1 and FVC. Interestingly, our study has shown that an improvement of functional lung parameters is correlated to an improvement of Pimax and FRC. The regular treatment with nCPAP probably improves the strength of the respiratory muscles, functional parameters, and gas exchange.
Nishimura and colleagues [26] showed a relationship between respiratory muscle force and FEV1 as well as FVC in COPD patients. In this regard, our study has shown that the application of long-term nCPAP increased FEV1/FVC and Pimax and favored an improvement in airflow rate. It is likely that nCPAP merely induces a pneumatic splinting effect, opposing smooth muscle contraction, and therefore, decreasing airway resistance and ventilatory function. This long-term effect of nCPAP can be attributed to the decrease in breathing work of the respiratory muscles. In another study, a significant improvement in gas exchange was obtained by administration of positive pressure ventilation via face mask to patients with acute exacerbation of COPD [27].
The results of our study demonstrate that home nCPAP for a 2-year period is effective in alleviating daytime sleepiness and in reversing cardiorespiratory failure in patients with mild to moderate COPD and coexisting severe OSA. Both nCPAP and bilevel ventilatory support have been used clinically to manage patients with overlap syndrome [28].
In our study, all patients showed good tolerance to nCPAP (nCPAP therapy>4 h of use per night). We expected that, in patients with mild to moderate COPD, an improvement would be seen as a consequence of treating severe OSA with nCPAP therapy.
One study evaluated the long-term effects of treating OSA in patients with coexistent COPD. de Miguel et al. [29] studied the effects of CPAP therapy on lung function in patients with overlap syndrome over an 18-month period. They found improvements in blood gasses and spirometric values after the first 6 months. Response of overlap syndrome patients to CPAP therapy was greater in the hypercapnic group. However, no statistically significant differences were found in any parameters for the comparison between 6 and 18 months. These patients also had significant weight loss during this time, which may explain the benefits observed. Moreover, the degree of obstruction as reflected by the FEV1/FVC ratio did not change. Our data showed a similar trend with weight loss during the nCPAP therapy but, on the contrary, an increased respiratory rate with improved spirometric values. Interestingly, the study of de Miguel et al. [29] showed no improvements in spirometric values from 6 to 18 months, a period in which there was no change in patients' weight. Our data demonstrated improvements in all parameters, cardiac, respiratory, and weight, during CPAP therapy. Mansfield et al. [30] evaluated the effects of CPAP on lung function in patients with COPD and SDB treated for at least 8 months. They found an improvement in patients' arterial blood gasses and FEV1 and a decrease in hospitalizations. Peker et al. [31] also found that treatment of OSA with CPAP may decrease the need for acute hospital admission for cardiovascular and pulmonary disease. An abstract by Young et al. [32] evaluated long-term respiratory function changes in patients with OSA during treatment with CPAP. In this study, patients were followed up for variable periods of time (4 months to 5 years). The authors found no change in FEV1 or FVC; however, there was a decrease in total lung capacity, FRC, and RV. Unfortunately, it is unclear how many patients had COPD or restrictive lung disease. In our study, all respiratory and cardiovascular parameters improved progressively over time.
Sampol et al. [33] demonstrated that CPAP was able to improve overnight oxygenation in patients with overlap syndrome. Sforza et al. [34] also evaluated the long-term effects of CPAP in patients with OSA, of whom a significant percentage also had COPD as judged by their pulmonary function studies. They found an improvement in arterial blood gasses, but not in lung function tests; actually, there was a small but significant decrease in FEV1 and FEV1/FVC ratio. Unlike CPAP, which by definition applies the same pressure throughout the ventilatory cycle, bilevel positive airway pressure (PAP) permits independent adjustment of the pressure applied during inspiration and that applied during expiration. Application of expiratory PAP prevents the static upper airway occlusion (e.g., at end expiration), whereas inspiratory PAP prevents the dynamic upper airway obstruction that is related to inspiratory physiology. There is some evidence from case series studies suggesting that bilevel PAP offers a treatment advantage in subpopulations of patients, for example, those with obesity hypoventilation syndrome and hypercapnic patients with COPD [35, 36]. These studies were neither large nor long-term. Given the potential advantages of bilevel PAP, blind randomized studies with long-term follow-up are needed to elucidate the advantages and disadvantages of this modality as initial treatment of patients with medical comorbidities and as “salvage” therapy in those patients who are unresponsive to, do not accept, are intolerant of, or inadequately adhere to fixed-pressure CPAP. Although research supports a favorable influence of PAP therapy on risk for significant adverse outcomes in patients with severe OSA, well-designed trials are still required to elucidate the effect of PAP on health, quality of life, and economic risks in patients with milder OSA.
In patients with severe hypercapnic COPD without associated OSA, the long-term effects of NIV have not been convincingly demonstrated so far [37, 38]. Further clinical trials of the overlap syndrome are urgently needed.
Besides, our study outlined the association of overlap syndrome with coronary artery disease (CAD) including ischemia for about 58%, with arterial hypertension for about 67%, and with diabetes mellitus for 25% of patients; moreover, all patients were smokers.
In recent years, an incidence of OSA with CAD between 31% and 50%, OSA with arterial hypertension in 25% [39], and OSA with diabetes mellitus in 30.1% [40] have been also outlined.
Conclusions
Our data showed that, in this group of patients affected by mild-to-moderate COPD with mild hypoxemia (PaO2 > 60 mmHg) and severe OSA (AHI > 30 events per hour of sleep), nCPAP therapy improved and stabilized PaCO2, PaO2, MPAP, and AHI, starting from 3 months of treatment with nCPAP. The greater improvement was noted in the ESS score, T 90, and Pimax at 3 months as well as at 12 months, and their values showed no significant changes up to 24 months; the higher CPAP pressure reduced AHI and improved nocturnal hypoxemia. The improvements in symptoms and blood gas levels were directly associated to adherence to nCPAP therapy. ESS variability was highly correlated with T 90, Pimax, FEV1, and PaCO2; moreover, T 90 variability was highly correlated with Pimax. Overall, nCPAP benefits were detectable after 3 months and largely stabilized after the first year.
Finally, our data support the early use of nCPAP in patients with overlap syndrome. Further clinical trials are, therefore, needed to better evaluate CPAP vs NIV.
Abbreviations
- AHI:
-
apnea–hypopnea index
- AECOPD:
-
acute exacerbations of COPD
- BMI (kg/m2):
-
body mass index
- COPD:
-
chronic obstructive pulmonary disease
- DE:
-
Doppler echocardiography
- ESS:
-
Epworth sleepiness scale
- FEV1%:
-
forced expiratory volume in 1 s
- FVC%:
-
forced vital capacity
- FRC%:
-
functional residual capacity
- MPAP (mmHg):
-
mean pulmonary artery pressure
- MSaO2%:
-
mean nocturnal SaO2
- Pimax :
-
maximal inspiratory pressure
- nCPAP:
-
nasal continuous positive airway pressure
- NPPV:
-
noninvasive positive pressure ventilation
- NIV:
-
noninvasive mechanical ventilation
- NSaO2%:
-
nadir nocturnal SaO2
- OSA:
-
obstructive sleep apnea syndrome
- OSA + COPD:
-
overlap syndrome
- PaCO2 (mmHg):
-
arterial carbon dioxide tension
- PaO2 (mmHg):
-
arterial oxygen partial pressure
- RHC:
-
right heart catheterization
- SaO2%:
-
arterial oxygen saturation
- TRT%:
-
total recording time
- T90%:
-
percentage of TRT spent with SaO2 ≤90%
References
Weitzenblum E, Chaouat A, Kessler R, Canuet M (2008) Overlap syndrome: obstructive sleep apnea in patients with chronic obstructive pulmonary disease. Proc Am Thorac Soc 5(2):237–241
Weitzenblum E, Chaouat A (2004) Sleep and chronic obstructive pulmonary disease. Sleep Med Rev 4:281–294
Coughlin S, Calverley P, Wilding J (2001) Sleep disordered breathing—a new component of syndrome x? Obes Rev 2:267–274
Fletcher EC (1990) Chronic lung disease in the sleep apnea syndrome. Lung 168(Suppl):751–761
Alam I, Lewis K, Stephens JW, Baxter JN (2007) Obesity, metabolic syndrome and sleep apnoea: all pro-inflammatory states. Obes Rev 8:119–127
Sullivan CE, Berthon-Jones M, Issa FG (1983) Nocturnal nasal airway pressure for sleep apnea. N Engl J Med 309:112 (letter)
Doherty LS, Kiely JL, Swan V et al (2005) Long-term effects of nasal continuous positive airway pressure therapy on cardiovascular outcomes in sleep apnea syndrome. Chest 127:2076–2084
Pauwels RA, Rabe KF (2004) Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet 364:613–620
Wijkstra PJ, Lacasse Y, Guyatt GH, Casanova C, Gay PC, Meecham Jones J, Goldstein RS (2003) A meta-analysis of nocturnal noninvasive positive pressure ventilation in patients with stable COPD. Chest 124(1):337–343
Krachman SL, Quaranta AJ, Berger TJ, Criner GJ (1997) Effects of noninvasive positive pressure ventilation on gas exchange and sleep in COPD patients. Chest 112:623–628
Petrof BJ, Kimoff RJ, Cosio LRD, MC GSB (1991) Nasal continuous positive airway pressure facilitates respiratory muscle function during sleep in severe COPD. Am Rev Respir Dis 143:928–935
Mansfield D, Naughton MT (1999) Effects of continuous positive airway pressure on lung function in patients with chronic obstructive pulmonary disease and sleep disordered breathing. Respirology 4(4):365–370
Rabe KF, Hurd S, Anzueto A, Barnes PJ, Buist SA, Calverley P, Fukuchi Y, Jenkins C, Rodriguez-Roisin R, van Weel C, Zielinski J, Global Initiative for Chronic Obstructive Lung Disease (2007) Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176(6):532–555
Abramson SV, Burke JB, Pauletto FJ, Kelly JJ Jr (1995) Use of multiple views in the echocardiographic assessment of pulmonary artery systolic pressure. J Am Soc Echocardiogr 8(1):55–60
Anonymous (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The report of an American Academy of Sleep Medicine Task Force. Sleep 22(5):667–689
Levi-Valensi P, Weitzenblum E, Rida Z, Aubry P, Braghiroli A, Donner C, Aprill M, Zielinski J, Wurtemberger G (1992) Sleep-related oxygen desaturation and daytime pulmonary haemodynamics in COPD patients. Eur Respir J 5:301–307
Black LF, Hyatt RE (1969) Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 99:696–702
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Teschler H, Berthon-Jones M, Thompson AB, Henkel A, Henry J, Konietzko N (1996) Automated continuous positive airway pressure titration for obstructive sleep apnea syndrome. Am J Respir Crit Care Med 154:734–740
Reeves-Hoche MK, Meck R, Zwillich CW (1994) Nasal CPAP: an objective evaluation of patient's compliance. Am J Respir Crit Care Med 149:149–154
Madison JM, Irwin RS (1998) Chronic obstructive pulmonary disease. Lancet 352:467–473
Celli BR, MacNee W, committee members (2004) Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 23:932–946
Fisher MR, Criner GJ, Fishman AP, Hassoun PM, Minai OA, Scharf SM, Fessler AH, NETT Research Group (2007) Estimating pulmonary artery pressures by echocardiography in patients with emphysema. Eur Respir J 30:914–921
Kushida CA, Littner MR, Hirshkowitz M et al (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29:375–380
Stephen B, Dalal P, Berger M, Schweitzer P, Hecht S (1999) Noninvasive estimation of pulmonary artery diastolic pressure in patients with tricuspid regurgitation by Doppler echocardiography. Chest 116:73–77
Nishimura Y, Tsutsumi M, Nakata H, Tsunenari T, Maeda H, Yokoyama M (1995) Relationship between respiratory muscle strength and lean body mass in men with COPD. Chest 107:1232–1236
Brochard L, Isabey D, Piquet J, Amaro P, Mancebo J, Messadi AA, Brun-Buisson C, Rauss A, Lemaire F, Harf A (1990) Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. N Engl J Med 323:1523–1530
Robert D, Argaud L (2007) Clinical review: long-term non-invasive ventilation. Crit Care 11:210
de Miguel J, Cabello J, Sanchez-Alarcos JM et al (2002) Long term effects of treatment with nasal continuous positive airway pressure on lung function in patients with overlap syndrome. Sleep Breath 6:3–10
Mansfield D, Naughton MT (1999) Effects of continuous positive airway pressure on lung function in patients with chronic obstructive pulmonary disease and sleep disordered breathing. Respirology 4:365–370
Peker Y, Hedner J, Johansson A, Bende M (1997) Reduced hospitalization with cardiovascular and pulmonary disease in OSA patients on nasal CPAP treatment. Sleep 20:645–653
Young IH, Milhalyka M, Costas L, Sullivan CE (1987) Long term lung function changes in patients with obstructive sleep apnoea during treatment with nasal continuous positive airway pressure. Thorax 42:722
Sampol G, Sagalés MT, Roca A, de la Calzada MD, Bofill JM, Morell F (1996) Nasal continuous positive airway pressure with supplemental oxygen in coexistent sleep apnoea–hypopnoea syndrome and severe chronic obstructive pulmonary disease. Eur Respir J 9:111–116
Sforza E, Krieger J, Weitzenblum E, Aprill M, Lampert E, Ratamaharo J (1990) Long-term effects of treatment with nasal continuous positive airway pressure on daytime lung function and pulmonary haemodynamics in patients with obstructive sleep apnea. Am Rev Respir Dis 141:866–870
Resta O, Guido P, Picca V, Sabato R, Rizzi M, Scarpelli F, Sergi M (1998) Prescription of nCPAP and nBiPAP in obstructive sleep apnoea syndrome: Italian experience in 105 subjects. A prospective two centre study. Respir Med 92:820–827
Schafer H, Ewig S, Hasper E, Luderitz B (1998) Failure of CPAP therapy in obstructive sleep apnoea syndrome: predictive factors and treatment with bi-level-positive airway pressure. Respir Med 92:208–215
Strumpf DA, Millman RP, Carlisle CC, Grattan LM, Ryan SM, Erickson AD, Hill NS (1991) Nocturnal positive-pressure ventilation via nasal mask in patients with severe chronic obstructive pulmonary disease. Am Rev Respir Dis 144:1234–1239
Gay PC, Hubmayr RD, Stroetz RW (1996) Efficacy of nocturnal nasal ventilation in stable, severe chronic obstructive pulmonary disease during a 3-month controlled trial. Mayo Clin Proc 71:533–542
Lüthje L, Andreas S (2008) Obstructive sleep apnea and coronary artery disease. Sleep Med Rev 12:19–31
Tasali E, Mokhlesi B, Van Cauter E (2008) Obstructive sleep apnea and type 2 diabetes: interacting epidemics. Chest 133:496–506
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Toraldo, D.M., De Nuccio, F. & Nicolardi, G. Fixed-pressure nCPAP in patients with obstructive sleep apnea (OSA) syndrome and chronic obstructive pulmonary disease (COPD): a 24-month follow-up study. Sleep Breath 14, 115–123 (2010). https://doi.org/10.1007/s11325-009-0291-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-009-0291-1