Abstract
Objectives
The exact pathophysiology leading to pharyngeal collapse in obstructive sleep apnea syndrome (OSAS) remains incompletely understood. Prior research has shown that normal men have a longer pharyngeal airway than women, and it has been hypothesized that this difference may play a role in the gender-related differences in OSAS. In the current study, we sought to study the potential relationship between the length of the collapsible pharyngeal segment, the upper airway length (UAL), and the severity of OSAS.
Study design
The hospital records were searched for all patients who had had polysomnography and also had had a computed tomography of the neck. A total of 24 such patients were identified who participated (15 men and nine women).
Measurements and results
The UAL, the distance between the lower posterior part of the hard palate bone to the upper posterior part of the hyoid bone, was measured for all participants in the midsagittal plane. A correlation coefficient (Pearson r) of 0.406 was found between Respiratory Disturbance Index (RDI) and UAL (p = 0.049). When UAL was normalized to body height, a correlation coefficient (r) of 0.423 was found (p = 0.039). A gender-related difference in UAL was also found. Men with OSAS were found to have longer UAL even when normalized to body height (p = 0.003, unpaired t test) as compared with OSAS women.
Conclusion
This study provides potential clinical relevance to prior studies in normal subjects, by demonstrating that men with OSAS have longer UAL than women with OSAS, independent of body size. In addition, the significant correlation between UAL and OSAS severity suggests that UAL may play a role in the pathophysiology of OSAS. These findings are consistent with our predictions from computational modeling studies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea syndrome (OSAS) is a common disorder characterized by repetitive pharyngeal collapse during sleep. OSAS has gained increasing attention in the literature because of convincing data showing important neurocognitive and cardiovascular sequelae [1–3], as well as increased health care utilization and costs [4].
The pathophysiology leading to pharyngeal collapse and apnea is incompletely understood. Current theories on OSAS pathogenesis involve a combination of abnormalities in the following: the anatomy of the pharynx, the physiology of the upper airway dilator muscles, and the stability of ventilatory control [5]. Anatomical studies based upon various imaging techniques have focused mainly on the width of the pharynx; these include anteroposterior, lateral, and cross-sectional measurements at different pharyngeal levels [6–9]. According to Bernoulli’s principle, a fluid (much like air stream) flowing through a tube is susceptible to increase in velocity and decrease in pressure in a narrow segment. In the case of OSAS, a decline in pressure may lead to collapse, especially if the airway is narrow or the surrounding tissue pressures are high. Indeed, several anatomical parameters have been associated with apnea. These include larger lateral pharyngeal walls [7], thicker soft palate [9], and wider retropharyngeal tissue [10].
The length of the pharyngeal airway, however, has received only minimal attention so far. We have previously reported that upper airway length (UAL) was greater in normal men compared to women, suggesting that it may play a role in the male predisposition to pharyngeal collapse [11]. Further, using computational modeling, we have reported a major impact of UAL on pharyngeal mechanics [11]. In another study of 69 healthy boys and girls who had undergone computed tomography (CT) scans of the neck, we have found prepubertal children UAL to be equal between genders. However, following puberty, males were found to have longer upper airways than females (independent of systemic growth), thus potentially explaining why pharyngeal collapse has a strong male predominance in adults but not in children [12]. In addition, we have reported a longer pharyngeal airway in normal women following the menopause as compared with premenopausal women [13]. Thus, the existing data would suggest that upper airway length may at least partially explain the male predisposition to airway collapse that occurs at puberty and the female predisposition which occurs at menopause. However, all of these prior studies have included only healthy control males and females and have not investigated patients with OSAS. Thus, the clinical relevance of our prior research has been questioned.
In the present study, the UAL is evaluated in patients with OSAS. Based on prior studies and underlying pathophysiology, we hypothesized that a longer pharyngeal airway would be an important predictor of sleep apnea severity and that gender differences would be present in UAL of OSAS patients. Such findings could help to prove or refute the potential clinical relevance of our prior studies on UAL in normal subjects.
Materials and methods
To identify potential participants, we searched for all individuals who had undergone both polysomnography (PSG) and CT of the neck for clinical purposes in the Rambam hospital archives in the prior 4 years (i.e., both tests between January 2002 and March 2006). The reason for the PSG was in most cases snoring and suspected OSAS. The reasons for the neck CT included mostly elective orthopedic scans, trauma, and suspected neck mass (which was subsequently excluded). We found a total of 29 matching patients who had undergone both tests within the study period. The average time between the CT and the PSG was 14 months (range between less than a month and 49 months).
All CT scans were done while the patient was awake and in the supine position. We routinely perform CT scanning with the patient in a standard position (Frankfort plane) unless otherwise specified by the ordering clinician.
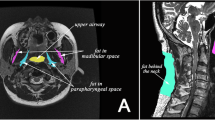
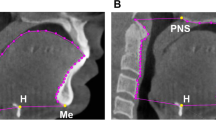
By using sagittal reconstruction, the distance between the lower posterior part of the hard palate bone to the upper posterior part of the hyoid bone was measured digitally in the midsagittal plane (Fig. 1). This distance refers to UAL [11, 12] and can be easily and accurately measured on a CT scan [11]. While reviewing the CT scans, we did not recognize any problematic images, e.g., not in the neutral anatomical position.
All polysomnographies were performed for a full night using a computerized PSG system (Embla Flaga hf, Iceland), with the following channels: electroencephalography (C3-A2 and O2-A1), electrooculography (Rt. And Lt.), chin electromyography (EMG), arterial oxygen saturation, nasal airflow (pressure canula), electrocardiogram, chest and abdominal wall motion (piezo electrodes), bilateral tibialis EMG, and body position. The PSG recordings were scored manually for sleep stages and respiratory events according to the American Academy of Sleep Medicine Criteria, 1999. A hypopnea event was defined as an airflow amplitude reduction of more than 50% from the baseline lasting at least 10 s or having a less significant reduction in the airflow amplitude but with the presence of arousal or oxygen desaturation of at least 3%. The RDI was calculated as the number of apnea–hypopnea events per hour of sleep. The scoring technician was unaware of the CT scan results.
Patient’s medical history, demographic and physical measures, as well as PSG report were taken as documented in the medical charts. Polysomnography for all patients included an overnight study in a sleep laboratory. Age, height, and weight were taken from the date of PSG.
After reviewing a senior radiologist's interpretations of all CT scans and patients’ charts, five patients were excluded from participation. These consisted of one patient who had had an upper cervical orthopedic surgery within days prior to the CT scan, two patients who had undergone surgical intervention that could have distorted the outcome variable (uvulopalatopharyngoplasty (UPPP) surgery and maxillomandibular advancement surgery for severe micrognathia), and one patient who suffered from severe insomnia with only 43 min of total sleep time in the polysomnography test, and one outlier patient was omitted (he had UAL more than 3 SD different from all the others). In all other CT scans, no abnormalities that could have potentially distorted UAL were found, and in all other PSGs the total sleep time was at least 3 h. The assessment of the UAL was performed by one investigator who was blinded to the PSG results and was not involved in the sleep study interpretations.
Thus, a total of 24 patients were included in the study, 21 of whom were referred with suspected OSA.
The study was approved by Rambam’s Medical Center Institutional Review Board.
Statistical analysis
Descriptive results are expressed as mean ± SD
Association between RDI and UAL was analyzed by using Pearson Product–Moment Correlation Coefficient r, with the level of significance (p value) tested based on the degree of freedom. UAL is represented not only in millimeters but also as a normalized measure with body height (UAL / height, millimeter per centimeter).
For the gender comparisons, unpaired t tests were performed for normally distributed data. The sample size was underpowered for within gender correlation calculations, and therefore these and other subgroup analyses are not reported. For all measures, p < 0.05 was defined as the threshold for statistical significance.
Results
Fifteen men and nine women with an age range of 33–80 years at the time of PSG were included in the study (Table 1). All were classified as suffering from OSAS, defined by a complaint of excessive daytime somnolence and RDI of over five events per hour, although three had a major complaint of insomnia.
A correlation coefficient (r) of 0.406 was found between RDI and UAL (p = 0.049). When UAL was normalized to body height, a correlation coefficient (r) of 0.423 was found (p = 0.039). Results are shown in Fig. 2.
When patients with RDI ≤ 10 per hour (n = 6) were compared with those with RDI > 10 per hour (n = 18), there was a significant longer airway to the RDI > 10 subgroup (64.3 mm vs 56.1 mm, p < 0.05).
A gender-related difference in UAL was also found. Men had longer UAL compared to women, 67.07 ± 6.72 vs. 54.24 ± 3.70 mm (p = 0.00003). When normalized to body height, the results were 0.387 ± 0.042 vs. 0.334 ± 0.023 mm/cm (p = 0.003). No statistically significant difference in RDI between men and women was observed (p = 0.18, two-tailed unpaired t test). Figure 3 summarizes these results. There were no significant correlations between UAL and age or BMI.
Discussion
This study reports significant correlation between upper airway length and respiratory disturbance index in a cohort of OSAS patients. It also demonstrates longer airway in patients with RDI > 10 per hour than in those with RDI up to ten per hour. Acknowledging potential limitations, these results demonstrate a potential role for airway length in OSAS pathogenesis and suggest (in the context of the existing literature) that assessment of airway length may be useful clinically in predicting response to certain therapies in OSAS patients.
It is well established that pharyngeal collapse during sleep leads to OSAS. The pharyngeal site of obstruction occurs in segments with lack of rigid bony support [5], predominantly the oropharynx and the hypopharynx [14]. The measure of UAL represents the length of these anatomical segments (Fig. 1). Since these measures use bony structures as references, it can easily and accurately be identified on a CT scan (or potentially cephalometries) and it represents the vertical distance of air streaming along the collapsible segment of the pharynx during basal breathing. The pathophysiology of pharyngeal collapse during sleep is, however, much more complex. One cannot expect a single anatomical measure to explain all of the variance in sleep apnea. Anatomy, pharyngeal dilator muscle function during sleep, and ventilatory control instability are all factors contributing to OSAS pathogenesis, and each mechanism (or group of mechanisms) likely has variable importance in predisposing to (or protecting from) development of OSAS [15]. Yet, our results suggest that UAL may be one of the factors contributing to collapse in patients with OSAS and may even predict its severity. It is indeed logical and likely that the length of the collapsible segment of the pharyngeal airway predicts the susceptibility to its collapse. Based on the rules of buckling of cylindrical shells [16], and since as nonrigid tubes become longer they are increasingly prone to collapse, we believe that airway length is a possible mechanism playing a role in increased upper airway collapsibility in patients with OSAS. Obviously, this statement assumes that the airway is tethered at its two edges to a rigid noncollapsible stable structure, and it depends on the tissues’ Young's modulus [17]. In these conditions, according to Bernoulli's law, a fluid (much like an air stream) flowing through a tube is susceptible to an increase in velocity and decrease in pressure within a narrow segment.
Since UAL is a constant factor that cannot be simply corrected surgically, we speculate that determining it prior to other surgical intervention may have important clinical value. Indeed, by using cephalometric measures, Woodson et al. [18, 19] have found that nonresponders to UPPP had longer airways compared to responders; thus, airway length can potentially help to predict surgical response. Thus, we believe that research into factors that predispose to airway collapsibility (e.g., airway length) would be helpful in explaining the limited success of surgical interventions such as UPPP in unselected patients [20]. On the other hand, surgical success rates could potentially be improved if patients were appropriately stratified preoperatively. Thus, further research assessing this hypothesis would be of major interest and clinical importance.
The comparison between men and women suggests longer UAL in men compared to women even when data are normalized for body height. These findings are consistent with previous studies in normal subjects [11, 12] but are assessed here for the first time in OSAS patients, to our knowledge. We speculate that pharyngeal airway length may be an important determining factor in the increased collapsibility we have previously reported in normal men vs. women, despite similar upper airway dilator muscle (genioglossus and tensor palatini) activation [21]. However, another explanation for longer airway and worse OSAS in men is that male gender causes through independent mechanisms an elongated UAL and a greater RDI. To clarify this option, a larger scale study is required.
As mentioned, patients with OSAS have a reduced pharyngeal lumen size when compared with normal subjects, but women have smaller pharyngeal lumen size than men [22, 23]. Thus, anatomical pharyngeal cross-sectional area alone is unlikely to explain the pathophysiology of apnea. These findings of shorter UAL in women that correspond to lower RDI and the correlation between UAL and RDI for the whole group support a potential role for UAL in the pathophysiology of pharyngeal collapse and in the male predominance of OSAS. Because men are generally larger than women, some have advocated normalizing gender-related data of upper airway anatomical findings for body size. However, others have argued that deleterious upper airway characteristics would predispose to apnea regardless of systemic measurements. Thus, we present the data in both forms (normalized and not normalized) so as to avoid the potential criticisms that we are simply identifying surrogates for overall body size. Following this normalization, men had longer UAL / height, and the correlation to RDI was preserved (r = 0.423, p = 0.039). Thus, we believe that our findings are important, regardless of the methods we use in reporting them.
The issue of CT as a diagnostic or preoperative tool for OSAS is a matter of controversy. Currently, patients investigated for sleep-disordered breathing do not require routine CT on a clinical basis. Some authors who have reported anatomical abnormalities in OSAS have recommended CT clinically for OSAS patients. We expect that with additional data regarding UAL and surgical outcome this question may be better answered. We would also support investigation regarding the use of cephalometries to define the variables of interest and to stratify probability of surgical success.
Our study clearly has several limitations. First, we used a convenience sample such that there may be a selection bias since only patients who had CT of the neck (for reasons other than OSAS) and only patients studied by PSG were assessed. Thus, we suggest that the results of our study should not be regarded as definitive and may not generalize to other populations. Nevertheless, we are unaware of any reason for systematic bias in this study and thus we further believe the methods (and any random errors that may have resulted) should bias towards the null hypothesis. Second, the sample size in this study is modest, again emphasizing the need for further work in this area. Third, given the retrospective nature of this study, head position was not rigorously controlled and there could be minor variations influencing our results. These variations are likely to be random as we are aware of no particular reason to believe that they are systematic or biased in any specific direction. If head position is important in affecting our outcomes, random variations in its position would make it more difficult to show an association between UAL and RDI. Thus, we doubt that minor variations of head and jaw positioning importantly influenced our results. Finally, we assessed UAL as a straight line (from the upper margin of the hyoid bone up to the lower margin of the hard palate) and we cannot be sure if it accurately reflects the length of a curved airway. However, we have no data whether the curvature of the upper airway changes by gender or OSAS and cannot comment whether it had any effect on our results. Although techniques have been reported to straighten the airway, we are unclear how this “unfolding” process may affect pharyngeal mechanics.
Conclusion
We have demonstrated a significant predictive value of upper airway length on the severity of OSAS, which supports the theory that UAL may play a role in the pathophysiology of airway collapse and gender-related differences in the occurrence of OSAS. Further studies with larger sample sizes in other populations (e.g., those undergoing surgical manipulation and variable genders, ages, and body mass indices) are required to better understand the role of UAL in OSAS.
References
Teran-Santos J, Jimenez-Gomez A, Cordero-Guevara J (1999) The association between sleep apnoea and the risk of traffic accidents. Cooperative Group Burgos-Santander. N Engl J Med 340:847–851
Pepperell J, Ramdassingh-Dow S, Crosthwaite N, Mullins R, Jenkinson C, Stradling JR, Davies RJ (2002) Ambulatory blood pressure after therapeutic and subtherapeutic nasal continuous positive airway pressure for obstructive sleep apnoea: a randomised parallel trial. Lancet 359:204–210
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O’Connor GT, Boland LL, Schwartz JE, Samet JM (2001) Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 163:19–25
Tarasiuk A, Greenberg-Dotan S, Brin YS, Simon T, Tal A, Reuveni H (2005) Determinants affecting health-care utilization in obstructive sleep apnea syndrome patients. Chest 128(3):1310–1314
Malhotra A, White PD (2002) Obstructive sleep apnoea. Lancet 360(9328):237–246
Haponik EF, Smith PL, Bohlman ME, Allen RP, Goldman SM, Bleecker ER (1983) Computerized tomography in obstructive sleep apnea. Correlation of airway size with physiology during sleep and wakefulness. Am Rev Respir Dis 127(2):221–226
Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffman EA, Pack AI (1995) Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med 152(5 Pt 1):1673–1689
Avrahami E, Englender M (1995) Relation between CT axial cross-sectional area of the oropharynx and obstructive sleep apnea syndrome in adults. Am J Neuroradiol 16(1):135–140
Yucel A, Unlu M, Haktanir A, Acar M, Fidan F (2005) Evaluation of the upper airway cross-sectional area changes in different degrees of severity of obstructive sleep apnea syndrome: cephalometric and dynamic CT study. Am J Neuroradiol 26(10):2624–2629
Caballero P, Alvarez-Sala R, Garcia-Rio F, Prados C, Hernan MA, Villamor J, Alvarez-Sala JL (1998) CT in the evaluation of the upper airway in healthy subjects and in patients with obstructive sleep apnea syndrome. Chest 113(1):111–116
Malhotra A, Huang Y, Fogel RB, Pillar G, Edwards JK, Kikinis R, Loring SH, White DP (2002) The male predisposition to pharyngeal collapse: importance of airway length. Am J Respir Crit Care Med 166(10):1388–1395
Ronen O, Malhotra A, Pillar G (2007) The influence of gender and age on upper airway length during development. Pediatrics 120(4):e1028–e1034
Malhotra A, Huang Y, Fogel R, Lazic S, Pillar G, Jakab M, Kikinis R, White DP (2006) Aging influences on pharyngeal anatomy and physiology: the predisposition to pharyngeal collapse. Am J Med 119(1):72.e9–14
Rama AN, Tekwani SH, Kushida CA (2002) Sites of obstruction in obstructive sleep apnea. Chest 122(4):1139–1147 Review
Huang Y, Malhotra A, White DP (2005) Computational simulation of human upper airway collapse using a pressure-/state-dependent model of genioglossal muscle contraction under laminar flow conditions. J Appl Physiol 99(3):1138–1148
Ekstrom RE (1963) Buckling of cylindrical shells under combined torsion and hydrostatic pressure. Exp Mech 3:192–197
Huang Y, White DP, Malhotra A (2005) The impact of anatomic manipulations on pharyngeal collapse: results from a computational model of the normal human upper airway. Chest 128:1324–1330
Woodson BT, Conley SF (1997) Prediction of uvulopalatopharyngoplasty response using cephalometric radiograph. Am J Otolaryngol 18(3):179–184
Woodson BT, Conley SF, Dohse A, Feroah TR, Sewall SR, Fujita S (1997) Posterior cephalometric radiographic analysis in obstructive sleep apnea. Ann Otol Rhinol Laryngol 106(4):310–313
Sher AE, Schechtman KB, Piccirillo JF (1996) The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19(2):156–177 Review
Pillar G, Malhotra A, Fogel R, Beauregard J, Schnall R, White DP (2000) Airway mechanics and ventilation in response to resistive loading during sleep: influence of gender. Am J Resp Crit Care Med 162:1627–1632
Brooks LJ, Strohl KP (1992) Size and mechanical properties of the pharynx in healthy men and women. Am Rev Respir Dis 146(6):1394–1397
Brown IG, Zamel N, Hoffstein V (1986) Pharyngeal cross-sectional area in normal men and women. J Appl Physiol 61(3):890–895
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Segal, Y., Malhotra, A. & Pillar, G. Upper airway length may be associated with the severity of obstructive sleep apnea syndrome. Sleep Breath 12, 311–316 (2008). https://doi.org/10.1007/s11325-008-0191-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-008-0191-9