Abstract
Obstructive sleep apnea (OSA) is a prevalent sleep disorder that disproportionately affects blacks. While clinical and epidemiologic data indicate intraethnic differences in several medical diseases, little is known about whether OSA symptoms differ within the black ethnic group. We estimated the rate of OSA symptoms in a community-based sample of Caribbean-born black men and women. We also ascertained which sociodemographic and/or medical factors were associated with OSA risk. A total of 554 patients (mean age = 48.17 ± 16.75 years) participated in the study; 55% were women. Data were collected in four primary-care clinics in Brooklyn, NY. A health educator explained the purpose of the study to interested patients and assisted consenting participants in completing questionnaires, which required 15 min to complete. Participants reporting habitual snoring, excessive daytime sleepiness, and sleep fragmentation were considered at high OSA risk. The rate of OSA symptoms was: snoring (45%), excessive daytime sleepiness (33%), and difficulty maintaining sleep (34%). Many reported falling asleep while watching television (47%) or while driving (14%). Based on logistic regression analysis, a history of heart disease was the most important predictor of the likelihood of expressing OSA symptoms, with a corresponding multivariate-adjusted odds ratio of 11 (95% confidence interval = 3.03–40.63). Findings suggest the need to investigate whether Caribbean-born blacks are at greater risk for developing OSA than African Americans and whites. Caribbean-born blacks with a history of heart disease should be a prime target for interventions that promote adequate screening and timely OSA diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a prevalent sleep disorder characterized by recurrent apnea and hypopnea episodes resulting from partial or complete closure of the upper airway during sleep [1]. Resulting breathing pauses lead to intermittent nighttime hypoxemia, which in turn causes recurrent cortical arousals associated with sleep fragmentation, loud snoring [2], and hemodynamic changes [3, 4]. Consequences of untreated OSA include altered sleep architecture [5], cognitive deficits and poor performance [6], excessive daytime sleepiness, and fatigue [7]. Furthermore, OSA has been linked to cardiovascular morbidity [8–11], automobile accidents [12, 13], and excess mortality [9, 14].
Results of an important epidemiological study conducted in 1993 indicated that 2% of middle-aged women and 4% of middle aged men met the diagnostic criteria for OSA [15]. Investigators concluded that 9% of women and 24% of men have an apnea–hypopnea index (AHI) greater than or equal to 5 and thus are at an increased risk for OSA. More recent studies suggest that the number of American adults at risk for OSA is increasing. According to the 2005 National Sleep Foundation survey, 26% of US adults (men = 31% and women = 21%) are at high risk for OSA [16]. Despite the alarming increase in OSA estimates, only 10% of the US population has received adequate screening. It is estimated that 82% of men and 93% of women with moderate to severe sleep apnea remain undiagnosed [17].
It remains unclear whether available prevalence estimates are applicable to each ethnic group comprising the US population. In the last decade, some effort has been made to study differences in the prevalence and severity of OSA among blacks and whites. Evidence shows that the incidence, prevalence, and severity of OSA are strikingly higher among blacks relative to whites [16–21]. A home sleep study performed among community-dwelling adults (age ≥65) showed that blacks were 2.5 times more likely to have an AHI of 30 or higher compared to whites [18]. Ethnic disparities in OSA estimates might even be greater if one considered a respiratory disturbance index greater than 10. In effect, in a study comparing 225 black and 622 white volunteers, aged 2–86 years, 31% of blacks versus 10% of whites had OSA [22]. Another worthy observation in that study is that young blacks (≤25 years) may be at a greater risk for OSA than their young white counterparts. Some have argued that there may be a genetic basis for OSA pointing to data suggesting a segregation in the codominant pattern of inheritance among blacks, with an allele frequency of 0.14 explaining 35% of the variance in OSA severity [23].
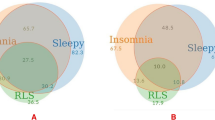
Data addressing intraethnic health disparities in sleep is scant, although available clinical and epidemiologic data indicate that intraethnic differences exist in several physical health measures [24–29]. For example, US-born blacks (African Americans) have a higher mortality rate than Caribbean-born blacks (Caribbean-born blacks) [30]. Using 1990 US Census data for New York City, African Americans ages 25 to 44 years had a death rate from coronary heart disease that was four times the rate for Caribbean Americans of the same sex and age [30]. This is consistent with a report from the NYC Department of Health and Mental Hygiene, indicating that Caribbean Americans are less likely to have medical illnesses upon migration to the USA, although risks tended to be similar after integration in mainstream society, usually occurring after 4 years of residence [31]. Regarding the sleep profile itself, a recent study conducted in Brooklyn, NY, showed that Caribbean Americans reported fewer insomnia complaints relative to African Americans (41.8% vs. 49.2%, respectively) [28]; the influence of duration of residence in New York on sleep could not be established in that study.
The evidence presented above suggests that African Americans are characteristically different from whites in regard to OSA prevalence and severity, but no comparative data exist for Caribbean Americans. Consistent with the increase in the Caribbean population in New York, there has been a growing interest to study the risk profile for diseases among men and women in that ethnic group. In the present study, we estimated the rate of OSA symptoms in a community-based sample of Caribbean men and women residing in Brooklyn, NY. We also ascertained whether those symptoms were associated with medical morbidity and sociodemographic factors.
Materials and methods
A total of 554 patients were recruited for the study. Their average age was 48.17 ± 16.75 years, range = 20–90 years. Of the sample, 55% were women and 45% were men. This study was conducted in four primary-care clinics in Central Brooklyn, serving primarily individuals born in the Caribbean. For data collection purposes, all patients who were 18 years old or older were eligible to participate. Eligible patients were approached by a health educator who explained the purpose of the study and obtained informed consent using procedures approved by the Institutional Review Board at Kingsbrook Jewish Medical Center. The health educator assisted all participants in completing questionnaires.
Questionnaires were available in both English and Haitian Creole, requiring approximately 15 minutes to complete. They included basic demographic questions as well as self-rated items on health status, sleep apnea symptoms, insomnia, and mood. Participants reporting habitual snoring, excessive daytime sleepiness, and sleep fragmentation were considered at high risk for sleep apnea. Physicians were encouraged to refer patients with positive screening results to see a sleep specialist.
Statistical analysis
All data were first entered in an Excel spreadsheet and were later converted into SPSS 15.0 for statistical analysis. The present analysis examined OSA symptoms and assessed associations of those factors with medical morbidity and sociodemographic variables. Frequency and measures of central tendency were used to describe the sample.
In preliminary analyses, Pearson and Spearman correlations were used to explore relationships between variables of interest. Fisher’s exact test was employed to assess differences in insomnia-related complaints comparing respondents at a high risk for OSA and those at low risk. The OSA risk factor classified individuals into two groups: those who reported snoring, excessive daytime sleepiness, and sleep fragmentation vs. those who did not. Relationships of OSA risk to medical factors and sociodemographic variables were examined with multiple logistic regression analysis. As indicated in Table 2, ten factors were entered in the final regression model. Factors were selected based on their theoretical importance; all correlated with the dependent measure (OSA risk) in preliminary analyses. Medical comorbidities were adjusted in the model.
Results
The rate of OSA symptoms in this sample was: snoring (45%), witnessed apneas (36%), and excessive daytime sleepiness (33%). Many of the respondents indicated falling asleep while watching television (47%) or while driving (14%). Overall, 34% reported difficulty initiating sleep, 34% difficulty maintaining sleep, and 44% early morning awakening; 35% indicated daytime napping and 11% used sleep medicine.
Of the sample, 35% reported a history of hypertension and 16% a history of heart problems. Thirty-four percent reported difficulty concentrating during the day. Sixty-four percent rated their health status as good to excellent and 36% as fair to poor; 34% were satisfied with their habitual sleep. The average body mass index (BMI) of the patient was 29.15 ± 7.16 kg/m2.
Using Fisher’s exact test, we found significantly greater rates of difficulty initiating sleep, early morning awakening, and daytime napping among respondents at high OSA risk (see Table 1). Based on logistic regression analysis, a history of heart disease was the most important predictor of the likelihood of reporting OSA symptoms. The corresponding multivariate-adjusted odds ratio was 11 (95% confidence interval = 3.034–40.625). Other factors showing significant relationships with OSA risk were a history of hypertension, sleep satisfaction, ability to concentrate during the day, and falling asleep while watching television (see Table 2).
Discussion
The recognition that health disparities exist has given the impetus for a number of studies investigating physical health characteristics in underserved minority communities. Epidemiologic and clinical studies have shown that generally blacks are characterized by more severe sleep apnea compared with their white counterparts [18, 32-35]. Our study is the first to examine symptoms of OSA among Caribbean men and women residing in Brooklyn, NY. The main finding of the study is that a significant number of Caribbean Americans reported OSA symptoms (i.e., snoring and excessive daytime sleepiness) and that a history of heart disease is a strong predictor of the likelihood of reporting these symptoms.
The estimate of habitual snoring, the typical symptom of OSA, in our sample (45%) was greater than estimates derived from the general US population or from other ethnic groups, including African Americans. According to the National Sleep Foundation, 32% of American adults (≥18 years) snore habitually [36]. This is consistent with data from the Cardiovascular Health Study, showing that 33% of respondents were habitual snorers [37]. Prevalence data specific to US-born blacks (African Americans) do not exist, but available clinical data suggest that snoring rates for blacks as a whole (29%) are greater than observed for whites (18%) [32, 33]. It is difficult to estimate how many respondents in the aforementioned studies might have been Caribbean-born blacks, since most published reports use aggregate ethnic groupings, precluding an assessment of intragroup differences. It may be that snoring rates for Caribbean-born blacks, as noted in our study, are in fact greater than observed among African Americans.
These findings are in line with previous reports suggesting that snoring is observable across cultures and countries, although its prevalence seems to vary on the basis of which country or culture is under investigation. Among French and British people for instance, snoring rates for middle-age adults were 35% and 40%, respectively [38, 39]. Snoring rates may be much lower among adults from Sweden (15%) [40] and from Singapore (6.8%) [41]; it was interesting to note ethnic differences comparing Chinese (6.2%), Malay (8.1%), and Indian respondents (10.9%). It seems reasonable to conclude that snoring rates among Caribbean American men and women might be greater than rates found for other ethnic groups, but definitive conclusions await population-based studies.
Excessive daytime sleepiness, another symptom highly suggestive of greater OSA risk, tended to be more common in our sample as well. Specifically, 33% of the participants reported excessive daytime sleepiness. By contrast, the estimated rate of daytime sleepiness in the 2005 Sleep in America poll was 27% [36], which might have included African Americans and Caribbean Americans. Comparatively, estimates of daytime sleepiness in Sweden, France, and in the UK were 16%, 20%, and 15%, respectively [39, 42, 43]. Of particular interest is the observation that rates of daytime sleepiness among Caribbean-born blacks in our study were also higher than that generally observed for blacks (19%) [44], who typically experience more severe daytime sleepiness than do age-matched whites [18, 34, 35]. These findings support the notion that blacks in America do not constitute a homogenous group regarding snoring and daytime sleepiness, two of the most frequent symptoms of OSA.
Our study raises an important question regarding the rationale for aggregating blacks of differing ethnic backgrounds in published reports. Our findings and others from the social science literature point to the need to consider intraethnic variations in physical health characteristics [24, 45-50]. The same could be said for other ethnic groups as well. In a previous study, comparing American women from six ethnic groups (US-born white, East Europe, Haiti, Barbados, Trinidad and Tobago, and Jamaica), we observed differences in both physical health characteristics and sleep complaints [29]. In sum, care should be exercised when interpreting sleep data collected from participants of differing ethnicities. This is supported by a recent report from the World Health Organization, evidencing that the prevalence of sleep apnea varies considerably across countries [51].
The second important finding from our analysis is that a history of heart disease was the strongest independent predictor of OSA risk among Caribbean men and women. The odds of reporting OSA symptoms (i.e., snoring, daytime sleepiness, and sleep fragmentation) were 11 times greater for respondents with a history of heart disease. To a lesser degree, the likelihood of reporting OSA symptoms was also associated with a history of hypertension, reduced satisfaction with sleep, reduced ability to concentrate, and inability to stay awake while watching TV. It is interesting to note that BMI was not an independent predictor of OSA risk in our analyses. One explanation for this observation is that BMI had shared variance with two other significant factors in the model namely, a history of heart disease and a history of hypertension.
The association of heart disease with OSA symptoms was expected, since numerous studies have established that OSA is more prevalent among individuals with cardiovascular disease [8, 10, 52, 53], congestive heart failure [9], and arrhythmias [52]. Furthermore, data from the Sleep Heart Health Study evidence that sleep apnea increases the risk of heart failure by 140%, the risk of stroke by 60%, and the risk of coronary heart disease by 30% [9]. However, we were surprised by such a high frequency of OSA symptoms among participants with a history of heart disease. This is particularly alarming given the fact that only 10% of patients with OSA have received a diagnosis, which is often attributed to a lack of training among primary-care physicians [54–57] and lack of referrals for sleep assessment when symptoms are detected [58].
One implication of these findings is that Caribbean-born patients with a history of heart disease should be a prime target for interventions that promote adequate screening and timely diagnosis of sleep apnea. A recent chart audit survey conducted in a sleep clinic serving primarily minority patients in Brooklyn revealed that black patients do not routinely adhere to the physician’s recommendation to see a sleep specialist (unpublished data). Caribbean American patients with a history of heart disease should receive a brief screening for sleep apnea while attending regular visits in primary-care facilities. Screening instruments are available and can be easily administered by the medical staff. Appropriate referrals for comprehensive sleep assessment should be encouraged.
Conclusion
As expected, individuals at high risk for OSA had a higher prevalence of sleep-related complaints, compared with individuals at low risk for OSA. The fact that Caribbean-born blacks in the present study had a higher rate of sleep-related complaints than previously determined [28] might reflect the fact that respondents in the present study were recruited in the clinical setting, although they were not necessarily seeking help for sleep problems. Thus, estimates derived from our sample cannot be used in a head-to-head match with population-based estimates.
Our study has some limitations regarding generalizability to the whole population of Caribbean-born individuals. Judging from the geographic location of the participating clinics, most of the patients were either from Jamaica, Haiti, and Trinidad and Tobago, which by no means constituted an accurate sampling of Caribbean people living in Brooklyn, NY. Additionally, our sample comprised patients attending regular visits with their physicians, who evidently had medical problems likely affecting their sleep. Notwithstanding this limitation, our data suggests the possibility that Caribbean-born blacks may be at greater risk for developing OSA than African Americans and whites and that those with a history of heart disease might be particularly vulnerable. This suggests that more aggressive effort should be made to increase screening rates for sleep apnea in that population, thereby increasing the likelihood for early detection and treatment to prevent cardiovascular complications. Future studies should assess sleep patterns among Caribbean Americans using epidemiologic methodologies.
References
Hudgel DW (1992) Mechanisms of obstructive sleep apnea. Chest 101:541–549
Patil SP, Schneider H, Schwartz AR, Smith PL (2007) Adult obstructive sleep apnea: pathophysiology and diagnosis. Chest 132:325–337
Pinto JM, Garpestad E, Weiss JW, Bergau DM, Kirby DA (1993) Hemodynamic changes associated with obstructive sleep apnea followed by arousal in a porcine model. J Appl Physiol 75:1439–1443
Somers VK, Dyken ME, Clary MP, Abboud FM (1995) Sympathetic neural mechanisms in obstructive sleep apnea. J Clin Invest 96:1897–1904
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
El Ad B, Lavie P (2005) Effect of sleep apnea on cognition and mood. Int Rev Psychiatry 17:277–282
Guilleminault C, Stoohs R, Clerk A, Cetel M, Maistros P (1993) A cause of excessive daytime sleepiness. The upper airway resistance syndrome. Chest 104:781–787
Kiely JL, McNicholas WT, Zgierska A, Gorecka D, Radzikowska M, Baranowska B, Plywaczewski R, Bednarek M, Przybylowski T, Korczynski P, Zielinski J (2000) Cardiovascular risk factors in patients with obstructive sleep apnoea syndrome [Obstructive sleep apnea and risk factors for coronary artery disease]. Eur Respir J 16:128–133
Wright J, Johns R, Watt I, Melville A, Sheldon T (1997) Health effects of obstructive sleep apnoea and the effectiveness of continuous positive airways pressure: a systematic review of the research evidence. BMJ 314:851–860
Findley LJ, Weiss JW, Jabour ER (1991) Drivers with untreated sleep apnea. A cause of death and serious injury. Arch Intern Med 151:1451–1452
Newman AB, Nieto FJ, Guidry U, Lind BK, Redline S, Pickering TG, Quan SF (2001) Relation of sleep-disordered breathing to cardiovascular disease risk factors: the Sleep Heart Health Study. Am J Epidemiol 154:50–59
Findley LJ, Weiss JW, Jabour ER (1991) Drivers with untreated sleep apnea. A cause of death and serious injury. Arch Intern Med 151:1451–1452
Stoohs RA, Guilleminault C, Itoi A, Dement WC (1994) Traffic accidents in commercial long-haul truck drivers: the influence of sleep-disordered breathing and obesity. Sleep 17:619–623
Lavie P, Herer P, Peled R, Berger I, Yoffe N, Zomer J, Rubin AH (1995) Mortality in sleep apnea patients: a multivariate analysis of risk factors. Sleep 18:149–157
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Hiestand DM, Britz P, Goldman M, Phillips B, Young T, Evans L, Finn L, Palta M (2006) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Chest 130:780–786
Young T, Finn L (1998) Epidemiological insights into the public health burden of sleep disordered breathing: sex differences in survival among sleep clinic patients. Thorax 53(Suppl 3):S16–S19
Ancoli-Israel S, Klauber MR, Stepnowsky C, Estline E, Chinn A, Fell R (1995) Sleep-disordered breathing in African-American elderly. Am J Respir Crit Care Med 152:1946–1949
Gottlieb DJ, Whitney CW, Bonekat WH, Iber C, James GD, Lebowitz M, Nieto FJ, Rosenberg CE (1999) Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Respir Crit Care Med 159:502–507
Ancoli-Israel S, Klauber MR, Stepnowsky C, Estline E, Chinn A, Fell R (1989) Sleep-disordered breathing in African-American elderly. J Gerontol 44:M18–M21
Redline S, Tishler PV, Hans MG, Tosteson TD, Strohl KP, Spry K (1997) Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med 155:186–192
Redline S, Tishler P, Hans M, Tosteson T, Strohl K, Spry K (1997) Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med 155:186–192
Buxbaum SG, Elston RC, Tishler PV, Redline S (2002) Genetics of the apnea hypopnea index in Caucasians and African Americans: I. Segregation analysis. Genet Epidemiol 22:243–253
Flack JM, Amaro H, Jenkins W, Kunitz S, Levy J, Mixon M, Yu E (1995) Epidemiology of minority health. Health Psychol 14:592–600
Mayberry RM, Mili F, Ofili E (2000) Racial and ethnic differences in access to medical care. Med Care Res Rev 57(Suppl 1):108–145
Penn NE, Kar S, Kramer J, Skinner J, Zambrana RE (1995) Ethnic minorities, health care systems, and behavior. Health Psychol 14:641–646
Jean-Louis G, Zizi F, Casimir G, Compas J (2007) Sleep in America: is race or culture an important factor? In: Leger D, Pandi-Perumal SR (eds) Sleep disorders: their impact on public health. Taylor & Francis, Oxford, UK, pp 37–39
Jean-Louis G, Magai C, Cohen CI, Zizi F, von Gizycki H, DiPalma J, Casimir G (2001) Ethnic differences in reported sleep problems in older adults. Sleep 24:926–933
Jean-Louis G, Magai C, Casimir GJ, Zizi F, Moise F, McKenzie D et al (2008) Insomnia symptoms in a multiethnic sample of American women. J Women’s Health 17:15–25
Fang J, Madhavan S, Alderman MH (1996) The association between birthplace and mortality from cardiovascular causes among black and white residents of New York City. N Engl J Med 335:1545–1551
Frieden T (2006) The health of immigrants in New York City: a report from the New York City Department of Health and Mental Hygiene. New York City Department of Health and Mental Hygiene, New York, pp 1–27
O’Connor GT, Lind BK, Lee ET, Nieto FJ, Redline S, Samet JM, Boland LL, Walsleben JA, Foster GL (2003) Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep 26:74–79
Kalra M, Bernstein D, Daftary A, Kalra H, LeMasters G (2005) Prevalence of snoring among young adult females with atopy. Chest 128:224S
Durrence HH, Lichstein KL (2006) The sleep of African Americans: a comparative review. Behav Sleep Med 4:29–44
Friedman M, Bliznikas D, Klein M, Duggal P, Somenek M, Joseph NJ (2006) Comparison of the incidences of obstructive sleep apnea–hypopnea syndrome in African-Americans versus Caucasian-Americans. Otolaryngol Head Neck Surg 134:545–550
National Sleep Foundation (2005) Omnibus sleep in America poll. National Sleep Foundation, Washington, DC, pp 1–51
Enright PL, Newman AB, Wahl PW, Manolio TA, Haponik EF, Boyle PJ (1996) Prevalence and correlates of snoring and observed apneas in 5,201 older adults. Sleep 19:531–538
Teculescu D, Benamghar L, Hannhart B, Montaut-Verient B, Michaely JP (2007) Habitual snoring. Prevalence and risk factors in a sample of the French male population. Rev Mal Respir 24:281–287
Ohayon MM, Guilleminault C, Priest RG, Caulet M (1997) Snoring and breathing pauses during sleep: telephone interview survey of a United Kingdom population sample. BMJ 314:860–863 [see comments]
Lindberg E, Taube A, Janson C, Gislason T, Svardsudd K, Boman G (1998) A 10-year follow-up of snoring in men. Chest 114:1048–1055
Ng TP, Seow A, Tan WC (1998) Prevalence of snoring and sleep breathing-related disorders in Chinese, Malay and Indian adults in Singapore. Eur Respir J 12:198–203
Soldatos CR, Allaert FA, Ohta T, Dikeos DG (2005) How do individuals sleep around the world? Results from a single-day survey in ten countries. Sleep Med 6:5–13
Ohayon MM, Caulet M, Philip P, Guilleminault C, Priest RG (1997) How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med 157:2645–2652
Qureshi AI, Giles WH, Croft JB, Bliwise DL (1997) Habitual sleep patterns and risk for stroke and coronary heart disease: a 10-year follow-up from NHANES I. Neurology 48:904–911
Giles DE, Perlis ML, Reynolds CF, Kupfer DJ (1998) EEG sleep in African-American patients with major depression: a historical case control study. Depress Anxiety 8:58–64
Hwu HG, Yeh EK, Chang LY (1989) Prevalence of psychiatric disorders in Taiwan defined by the Chinese Diagnostic Interview Schedule. Acta Psychiatr Scand 79:136–147
Poland RE, Rao U, Lutchmansingh P, McCracken JT, Lesser IM, Edwards C, Ott GE, Lin KM (1999) REM sleep in depression is influenced by ethnicity. Psychiatry Res 88:95–105
Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS (1994) Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry 51:8–19
Briones B, Adams N, Strauss M, Rosenberg C, Whalen C, Carskadon M, Roebuck T, Winters M, Redline S (1996) Relationship between sleepiness and general health status. Sleep 19:583–588
kleinman A (1981) Culture and patient care: psychiatry among the Chinese. Drug Therapy 11:134–140
Bousquet J, Khaltaev N (2007) Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. World Health Organization, Geneva, pp 1–146
Mehra R, Benjamin EJ, Shahar E, Gottlieb DJ, Nawabit R, Kirchner HL, Sahadevan J, Redline S (2006) Association of nocturnal arrhythmias with sleep-disordered breathing: the Sleep Heart Health Study. Am J Respir Crit Care Med 173:910–916
The National Commission on Sleep Disorders Research (1993) Wake up America: a national sleep alert. US Government Printing Office, Washington DC
Ball EM, Simon RD Jr., Tall AA, Banks MB, Nino-Murcia G, Dement WC (1997) Diagnosis and treatment of sleep apnea within the community. The Walla Walla Project. Arch Intern Med 157:419–424
Bahammam A, Kryger M (1999) Decision making in obstructive sleep-disordered breathing: putting it all together. Otolaryngol Clin North Am 32:333–348
Chung SA, Jairam S, Hussain MR, Shapiro CM (2001) Knowledge of sleep apnea in a sample grouping of primary care physicians. Sleep Breath 5:115–121
Silverberg DS, Oksenberg A, Iaina A (1997) Sleep related breathing disorders are common contributing factors to the production of essential hypertension but are neglected, underdiagnosed, and undertreated. Am J Hypertens 10:1319–1325
Kramer NR, Cook TE, Carlisle CC, Corwin RW, Millman RP (1999) The role of the primary care physician in recognizing obstructive sleep apnea. Arch Intern Med 159:965–968
Acknowledgments
Funding from NIH (1R24MD001090 and HL085042) supported this work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zizi, F., Jean-Louis, G., Fernandez, S. et al. Symptoms of obstructive sleep apnea in a Caribbean sample. Sleep Breath 12, 317–322 (2008). https://doi.org/10.1007/s11325-008-0190-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-008-0190-x