Abstract
More than two thirds of stroke patients suffer from sleep apnea. A recent study showed that mirtazapine reduced the respiratory disturbance index (RDI) of a stroke patient by 80%. These promising results prompted us to offer mirtazapine to non-depressed stroke patients who suffered from sleep apnea and refused treatment with a continuous positive airway pressure (CPAP) device. Polysomnography was performed between 2200 and 0600 hours. We examined ten inpatients [nine male, one female; mean age of 68.7 ± 1.5 years ± SE; body mass index of 26.1 ± 1.2 kg/m2, basal ganglia bleeding (n = 3), middle cerebral artery ischemia (n = 4), basal ganglia ischemia (n = 1), cerebellar bleeding (n = 2)] in the Neurologic Clinic’s sleep laboratory. The mean duration of illness before the first polysomnography was 52.6 ± 11.4 days. Mirtazapine effectively consolidated sleep in all patients, i.e., sleep efficiency significantly increased from 63.1 ± 4.8% to 75.7 ± 5.0%. A moderate increase in RDI (137.4 ± 15.3% of baseline) occurred during initial mirtazapine administration (intake duration 15.8 ± 5.5 days). After 51.9 ± 8.4 days, the RDI was either reduced (51.9% in “responders” who were identified arbitrarily by a reduction in RDI ≥ 25% at any time point of the investigation) or increased (154.4% in “non-responders”). Mirtazapine administration was stopped in the four patients with increased RDI. Mirtazapine may be a probably effective treatment in stroke survivors with obstructive sleep apnea who refuse nasal CPAP treatment. As it may worsen central and mixed sleep apnea, patients who receive mirtazapine to alleviate sleep apnea or to control post-stroke depression with sleep disturbances should be monitored for changes in breathing parameters during sleep.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
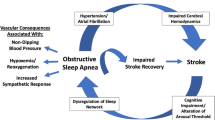
Stroke is one of the leading causes of death and a major cause of disability [1]. More than two thirds of stroke patients suffer from sleep apnea [2], which is also associated with poor outcome [3].
While the gold standard in the treatment of sleep apnea in these patients is nasal continuous positive airway pressure (nCPAP) therapy, only a minority of stroke victims are cognitively able to use nCPAP [4].
Mirtazapine is increasingly being used as an effective psychopharmacological agent to treat depressive disorders, and a recent case report [5] showed that it also reduced the respiratory disturbance index (RDI) by 80% in an 80-year-old man. Mirtazapine blocks central α2-autoreceptors at noradrenergic and serotonergic synapses and stimulates α1-adrenoreceptors at serotonergic neurons in the raphe nucleus, thus increasing noradrenaline and serotonine release. Mirtazapine stimulates 5-hydroxytryptamine 1 (5-HT1) receptors in the brain and may suppress apneas in non-rapid eye movement (REM) via 5-HT1A receptors [6]. The antagonism at 5-HT2 and 5-HT3 receptors in the central and peripheral nervous systems may be responsible for the suppression of apneas in REM [7]. Mirtazapine may further reduce apneas by augmenting slow-wave sleep [8].
This suggests that mirtazapine may be a useful medical treatment for stroke patients with post-stroke depression and/or sleep apnea. We therefore offered mirtazapine to ten stroke patients who suffered from severe sleep apnea and refused to use an nCPAP device.
Materials and methods
We examined ten patients (nine male, one female; mean age = 68.7 ± 1.5 years ± SE) with the following characteristics: mean BMI, 26.1 ± 1.2 kg/m2; basal ganglia bleeding (n = 3); middle cerebral artery ischemia (n = 4); basal ganglia ischemia (n = 1); cerebellar bleeding (n = 2); mean Barthel-index (BI) [9], 21.5 ± 7.7 at baseline. The BI [9] was developed in 1965 as a scoring technique that measures the patient’s performance in ten activities of daily life. The items can be divided into a group that is related to self-care (feeding, grooming, bathing, dressing, bowel and bladder care, and toilet use) and a group related to mobility (ambulation, transfers, and stair climbing). The maximal score is 100 if five-point increments are used, indicating that the patient is fully independent in physical functioning. The lowest score is 0, representing a totally dependent bedridden state. The mean duration of illness until first polysomnography (PSG) was 52.6 ± 11.4 days. All underwent a PSG in the sleep laboratory of the Neurologic Clinic and were diagnosed to have moderate to severe sleep apnea. All were routinely invited to a second night of PSG to calibrate nCPAP during sleep. Eight patients refused nCPAP without trying it, and two patients refused nCPAP after the first treatment night. All patients were then offered to take mirtazapine (15 mg at bedtime) after giving their informed consent. One patient was lost to follow-up after 9 days of mirtazapine intake. One patient had to stop taking mirtazapine after 2 weeks due to side effects and worsening of the RDI; he subsequently was convinced to begin nCPAP treatment.
Patients were tested at baseline (n = 10), after 15.8 ± 5.5 days (n = 6, mirtazapine early), and/or after 51.9 ± 9.4 days (n = 7, mirtazapine late) of intake of mirtazapine. Three patients were examined at the early time point only; their data were carried forward to the late time point. We were able to examine three patients at all three time points. PSG was performed between 2200 (lights out) and 0600 (lights on) hours in the sleep laboratory including the electroencephalogram (C3-A2, C4-A1), using the international 10–20 electrode system [10], an electrooculogram, and a submental electromyogram (EMG) in accordance with standardized guidelines [11] and an EMG of both anterior tibialis muscles. Obstructive apneas were defined as >80% reduction in airflow lasting ≥10 s. Hypopneas required a 50% reduction of the airflow and/or effort plus a desaturation of minimum 4% and/or an arousal. Central apneas were identified by the absence of respiratory effort during cessation of airflow. Mixed apneas began like central apneas, but the effort started earlier than the airflow. Scoring of sleep stages and respiratory events was done according to standard criteria [11, 12]. The sum of apneas and hypopneas per hour of sleep was expressed in the RDI and was calculated over the whole night. Sleep apnea was diagnosed when the RDI was >10/h to have a clear pathological value. Statistical analysis was performed with the Student’s t test.
Results
At baseline, all patients had fragmented sleep, including poor slow wave (SWS) and REM sleep. Mirtazapine significantly increased the mean sleep efficiency (from 63.1 ± 4.8% to 75.7 ± 5.0%, p < 0.05) by reducing the proportion of wake time after sleep onset (from 30.9 ± 4.6% to 15.5 ± 2.0%, n.s.), increasing SWS (from 7.5 ± 1.7% to 15.0 ± 3.7%, n.s.) and REM sleep (from 6.1 ± 1.1% to 11.3 ± 3.7%, p < 0.05) in all patients (observations made only at the early time point (n = 3) carried forward to the late time point). The respiratory parameters (Table 1) worsened during the initial phase of mirtazapine intake in four patients and remained stable (i.e., change from baseline <10%) in two patients (Fig. 1, 1). At the late time point, there was a slight decrease in RDI (Table 1), which was due to the improvement in four patients and the stability or worsening in three patients (Fig. 1, 1). A further analysis revealed that obstructive apneas remained stable at the early time point and decreased at the late time point (Table 1). In contrast, central apneas increased with time (Table 1). The mixed apneas initially increased and then fell near to baseline values (Table 1).
We defined sleep apnea treatment response as reduction in RDI ≥ 25% at any time point of the investigation, thus dividing the patients into responders and non-responders. At the first time point, no responder and only one non-responder had an RDI higher than 25% above baseline. At the late time point, responders had a significant (p < 0.05) reduction of 50% of the RDI, but non-responders showed an increase of 50% (Fig. 1, 1 and 2). The analysis of apnea subgroups showed that the number of all three types of apneas (i.e., obstructive, central, and mixed) decreased in responders, whereas the number of central and especially mixed apneas increased in non-responders at the early time point, the difference to responders being significant (p < 0.05, Fig. 2). The non-responders had a slightly higher value of mixed apneas already at baseline (4.5/h versus 1.8/h). Among those were two of the patients who were evaluated at all three time points. Only the mixed apneas were reduced at the late time point, while the number of central apneas was further increased in the non-reponders (Fig. 2). A comparison of the change in RDI with time of intake showed only a weak correlation between lower RDIs and longer duration of mirtazapine intake (Fig. 3). Also, there was no correlation of duration of illness with the number of central or mixed apneas in our sample.
Discussion
Mirtazapine improved sleep quality in stroke patients. It also reduced the RDI in some of the patients (the “responders”), which may decrease the risk of another cardiovascular event, including a new stroke [13]. In other patients (the “non-responders”), however, mirtazapine worsened sleep apnea and thus may secondarily exacerbate the neurological deficits [3, 13]. Therefore, the intake of mirtazapine by stroke patients should be paralleled by sleep apnea screening, at least by continuous overnight monitoring of oxygen saturation, because the oxygen desaturation index (ODI) may serve as an equivalent to the RDI [14], before and within the first 4–6 weeks of administration of the drug. Thereby, one would be able to identify those patients who may be at risk of worsening their sleep apnea by an increase in ODI/RDI because only in responders there was no change of the RDI at the early time point and a decrease in RDI at the late time point. Although the effect of mirtazapine in lowering the RDI was not comparable with an effective nCPAP treatment [15], it can be recognized as a probably effective treatment, as only 20% of stroke victims use nCPAP [4].
The responders may experience a further reduction of the RDI because the effect on the brainstem network controlling breathing may need more than 8 weeks.
There are several possible explanations to the mechanisms by which mirtazapine acts. Both central and obstructive apneas reflect, at least in part, dysregulation of central neural motor output patterning to the respiratory system. In upper airways predisposed to collapse by anatomic, mechanical, or muscular factors, this dysregulation may be manifested primarily by obstructive apneas. In mechanically stable upper airways, dysregulation of respiratory motor output patterning may be expressed primarily by central apneas or hypopneas. Therefore, any factor that destabilizes respiratory drive during sleep promotes apnea genesis. Thus, interventions stabilizing respiratory drive during sleep may reduce or eliminate apnea. Mirtazapine blocks presynaptic a2-adrenoreceptors and postsynaptic 5-HT2 and 5-HT3 receptors [16, 17]. Antagonism of presynaptic a2-receptors located on serotonergic neurons enhances serotonin release. Due to the parallel antagonistic action at 5-HT2A, 5-HT2C, and 5-HT3 receptors, the net effect is increased postsynaptic 5-HT1 activity within the brain and reduced 5-HT2 and 5-HT3 postsynaptic activity in the central and peripheral nervous systems. Each of these pharmacologic effects may serve to stimulate respiration and suppress apnea. Buspirone, a 5-HT1A agonist associated with respiratory stimulation, decreased overall apnea index by 35% in a group of five male patients with SAS [6]. Yoshioka and colleagues [7] demonstrated that central apneas in anesthetized rats could be blocked by 5-HT2 or 5-HT3 antagonists acting primarily at the nodose ganglia. Thus, the combined 5-HT2 and 5-HT3 antagonist activity of mirtazapine in the peripheral nervous system may contribute to the apnea suppression. Another mechanism relates to the impact of mirtazapine on sleep architecture. Mirtazapine increased slow-wave sleep, suggesting improved sleep consolidation, deeper NREM sleep, and suppression of apnea, as apneas are more likely to occur in light sleep states [8].
It is unlikely that the observed effect of mirtazapine was due to the natural time course of sleep apnea in stroke patients because obstructive apneas remain on a stable level during the period of recovery from stroke, while central apneas decline with time [18]. In our patients, we observed the opposite effect during mirtazapine intake with decreasing obstructive and increasing central and mixed apneas in the non-responders. In a series of patients suffering from sleep apnea, it had recently been shown that mirtazapine reduced obstructive apneas but was not recommended as therapy due to the main side effects sedation and weight gain [19]. However, in stroke patients who refuse nCPAP, where we have no good alternatives in treating sleep apnea, mirtazapine may be beneficial in reducing obstructive apneas. From our data, it is likely that non-responders are patients in whom central and mixed apneas increase during the first 7 to 10 days and can hence be identified and excluded from further use of mirtazapine.
It remains a matter of debate whether the mechanism of mirtazapine, which influences sleep apnea, differs in patients with and without neurological problems.
Our findings have to be replicated on a larger group in a randomized controlled trial.
References
Murray CJ, Lopez AD (1997) Alternative projections of mortality and disability by cause 1990–2020: global burden of disease study. Lancet 349:1498–1504
Bassetti C, Aldrich MS (1999) Sleep apnea in acute cerebrovascular disease: final report on 128 patients. Sleep 22:217–223
Good DC, Henkle JQ, Gelber D, Welsh J, Verhulst S (1996) Sleep-disordered breathing and poor functional outcome after stroke. Stroke 27:252–259
Palombini L, Guilleminault C (2006) Stroke and treatment with nasal CPAP. Eur J Neurol 13:198–200
Castillo JL, Menendez P, Segovia L, Guilleminault C (2004) Effectiveness of mirtazapine in the treatment of sleep apnea/hypopnea syndrome (SAHS). Sleep Med 5:507–508
Mendelson W, Maczaj M, Holt J (1991) Buspirone administration to sleep apnea patients. J Clin Psychopharmacol 11:71–72
Yoshioka M, Goda Y, Togashi H, Matsumoto M, Saito H (1992) Pharmacological characterization of 5-hydroxytryptamine-induced apnea in the rat. J Pharmacol Exp Ther 26:917–924
Redline S, Lester Kirchner HL, Quan SF, Gottlieb DJ, Kapur V, Newman A (2004) The Effects of Age, Sex, Ethnicity, and Sleep-Disordered Breathing on Sleep Architecture. Arch Intern Med 164:406–418
Mahoney F, Barthel D (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Jasper HH (1958) The ten-twenty electrode system of the International Federation. Electroencephalogr Clin Neurophysiol 10:371–375
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. UCLA Brain Information Service, Brain Research Institute, Los Angeles
The Report of an American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Marin JM, Carrizo SJ, Vicente E, Agusti AGN (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnoea–hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet 365:1046–1053
Fietze I, Dingli K, Diefenbach K, Douglas NJ, Glos M, Tallafuss M, Terhalle W, Witt C (2004) Night-to-night variation of the oxygen desaturation index in sleep apnoea syndrome. Eur Respir J 24:987–993
Abad VC, Guilleminault C (2006) Pharmacological management of sleep apnoea. Expert Opin Pharmacother 7:11–23
DeVane C (1998) Differential pharmacology of newer antidepressants. J Clin Psychiatry 59(Suppl. 20):85–93
deBoer T (1996) The pharmacologic profile of mirtazapine. J Clin Psychiatry 57(Suppl. 4):19–25
Parra O, Arboix A, Bechich S, García-Eroles L, Montserrat JM, López JA, Ballester E, Guerra JM, Sopena JJ (2000) Time course of sleep-related breathing disorders in first-ever stroke or transient ischemic attack. Am J Respir Crit Care Med 161:375–380
Carley DW, Olopade C, Ruigt GS, Radulovacki M (2007) Efficacy of mirtazapine in obstructive sleep apnea syndrome. Sleep 30:35–41
Acknowledgments
The author wishes to thank D. Dervic, I. Eichardt, A. Habenicht, B. Heinen, B. Rosenlehner, and M. Schroeder for their excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brunner, H. Success and failure of mirtazapine as alternative treatment in elderly stroke patients with sleep apnea—a preliminary open trial. Sleep Breath 12, 281–285 (2008). https://doi.org/10.1007/s11325-008-0177-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-008-0177-7