Abstract
C-reactive protein (CRP) and interleukin-6 (IL-6) are pro-inflammatory proteins and important risk factors for atherosclerosis. Plasma CRP levels in snoring children may or may not be elevated. Since obesity is prevalent among snoring children and is associated with elevated CRP levels, we aimed to investigate the relative contributions of sleep-disordered breathing (SDB) and obesity to the inflammatory processes in snoring children in this prospective study. Two hundred forty-four children (mean age 8.9 ± 3.4 years) underwent polysomnographic evaluation. CRP was measured the following morning, and plasma IL-6 levels from 111 randomly selected children were also examined. Plasma CRP and IL-6 levels were elevated in children with SDB. Log plasma CRP levels were higher in the moderate-severe SDB group (apnea/hypopnea index, AHI ≥ 5) compared to the mild SDB group (AHI ≥ 1 and <5; p < 0.0001) or the control group (AHI < 1; p = 0.0001). Log plasma CRP levels correlated with AHI, arousal index, relative BMI, and SpO2 nadir (r = 0.30, p < 0.0001; r = 0.21, p = 0.002; r = 0.39, p < 0.0001, r = −0.36, p < 0.0001, respectively). Log plasma CRP levels were lower in children with SpO2 nadir ≥90 (p < 0.0001). Sub-analysis of the 116 non-obese children in the cohort revealed similar findings. Log plasma IL-6 levels were increased in children with moderate–severe SDB compared to controls (p = 0.03) and correlated with AHI (r = 0.28, p = 0.003) and SpO2 nadir (r = −0.24, p = 0.02). Children with SDB display significant severity-dependent increases in plasma CRP and IL-6 levels independent of obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep-disordered breathing (SDB) is a highly prevalent condition in children, affecting 2–3% of all children [1, 2]. In recent years, pediatric SDB has been associated with a higher risk for cardiovascular morbidity. Indeed, increased prevalence of hypertension [3], alterations in blood pressure regulation [4], and changes in cardiac geometry [5] have been reported in children with SDB and have been ascribed to the presence of sustained sympathetic activation [6], and to induction of endothelial dysfunction [7]. This induction of endothelial dysfunction is most likely resulting from initiation and propagation of inflammatory responses within the microvasculature.
C-reactive protein (CRP), an important circulating marker of inflammation, is one of the best predictors for future cardiovascular morbidity [8] and directly participates in atheromatous lesion formation [9]. In a previous study, we have shown that plasma CRP levels are increased in children with SDB compared to controls and are correlated with the severity of the disease, i.e., the degree of hypoxemia and of sleep fragmentation, independently from the degree of obesity [10]. In support of our findings, Larkin et al. [11] further reported elevated plasma CRP levels in adolescents with SDB and free of known cardiovascular disease, suggesting that SDB in children may confer additional risk for cardiovascular morbidity beyond that of obesity. However, in contrast to both studies, normal levels of plasma CRP were reported in Greek children with SDB [12]. One of the suggested explanations for these discrepant findings between these studies could involve different prevalence of obesity between the cohorts [13]. Interleukin-6 (IL-6) is a pro-inflammatory cytokine that largely controls the synthesis of CRP and is also an important risk factor for atherosclerosis and cardiovascular morbidity [14, 15]. IL-6 is also released by adipose tissue, such that IL-6 plasma levels may also reflect the degree of adiposity [16, 17]. Increased levels of IL-6 have been found in the plasma of adults with SDB and in obese adults without SDB [18, 19].
Therefore, to better understand the relative contributions of obesity and SDB severity to the inflammatory processes ultimately leading to increased cardiovascular risk, we examined the plasma levels of both CRP and IL-6 in a large cohort of snoring children.
Materials and methods
Consecutive snoring children being evaluated for the presence of SDB were enrolled in the study. Exclusion criteria were the presence of genetic disorders, cerebral palsy, neuromuscular diseases, or any underlying systemic diseases or acute infectious processes. In addition, we included 48 control children who were age-, sex-, and ethnicity-matched, who had no history of snoring, and in addition had normal polysomnographic findings (see below). Blood was drawn between 7:00 to 8:00 a.m., the morning after the child underwent a standard polysomnographic evaluation in the sleep laboratory at the Kosair Children’s Hospital. A standard complete blood count was performed by the hospital laboratory, and both the total white blood cell (WBC) count and platelet count were recorded. Plasma CRP was measured within 2–3 h after collection using the Flex reagent Cartridge (Date Behring, Newark, DE), which is based on a particle-enhanced turbidimetric immunoassay technique. This method has a detection level of 0.05 mg/dl and exhibits linear behavior up to 255 mg/dl, with intra-assay and inter-assay coefficients of variability of 9% and 18%, respectively. Plasma was obtained from the blood sample and was stored at −80°C until assayed. Plasma IL-6 levels from 111 randomly selected samples were examined using commercial ELISA kit (R&D systems, Minneapolis, MN). This method has a minimum detection level of 0.039 pg/ml with intra-assay and inter-assay coefficients of variability of 7.4 and 7.8, respectively.
A standard overnight multichannel polysomnographic evaluation was performed in the sleep laboratory. Children were studied for up to 12 h in a quiet, darkened room with an ambient temperature of 24°C in the company of one of their parents. No drugs were used to induce sleep. The following parameters were measured: chest and abdominal wall movement by respiratory impedance or inductance plethysmography, heart rate by ECG, air flow was monitored with a sidestream end-tidal capnograph, which also provided breath-by-breath assessment of end-tidal carbon dioxide levels (PETCO2; BCI SC-300, Menomonee Falls, WI), nasal pressure catheter, and an oronasal thermistor. Arterial oxygen saturation (SpO2) was assessed by pulse oximetry (Nellcor N 100; Nellcor, Hayward, CA), with simultaneous recording of the pulse waveform. The bilateral electrooculogram, eight channels of electroencephalogram, chin and anterior tibial electromyograms, and analog output from a body position sensor (Braebon Medical, NY) were also monitored. All measures were digitized using a commercially available polysomnography system (Rembrandt, MedCare Diagnostics, Amsterdam). Tracheal sound was monitored with a microphone sensor (Sleepmate, VA) and a digital time-synchronized video recording was performed.
Sleep architecture was assessed by standard techniques [20]. The proportion of time spent in each sleep stage was expressed as percentage of total sleep time (%TST). Central, obstructive, and mixed apneic events were counted. Obstructive apnea was defined as the absence of airflow with continued chest wall and abdominal movement for a duration of at least two breaths [21, 22]. Hypopneas were defined as a decrease in oronasal flow of ≥50% on either the thermistor or nasal pressure transducer signal with a corresponding decrease in SpO2 of ≥4% and/or arousal [22]. The obstructive apnea/hypopnea index (AHI) was defined as the number of apnea and hypopneas per hour of TST. Children with an AHI ≥ 1 but <5 per hour of TST were considered to have mild SDB, while children with AHI ≥ 5 per hour TST were considered to have moderate–severe SDB. Control children (CO) were defined as non-snoring children with AHI <1 per hour of TST.
The mean oxygen saturation, as measured by pulse oximetry (SpO2) in the presence of a pulse waveform signal void of motion artifact, and the nadir SpO2 were recorded. To further examine the role of hypoxemia, children were divided according to their SpO2 nadir into four groups: children with SpO2 nadir ≥90% (group A), children with SpO2 nadir of 80–89% (group B), children with SpO2 nadir of 70–79% (group C), and children with SpO2 nadir <70% (group D). Since criteria for arousals have not yet been developed for children, arousals were defined as recommended by the American Sleep Disorders Association Task Force report [23] using the 3-s rule and/or the presence of movement arousal [24].
Height and weight were obtained from each child. Body mass index (BMI) was calculated and also expressed as relative BMI (relBMI), using the following formula: (BMI/BMI of the 50th percentile for age and gender)×100, based on standardized percentile curves [25]. Obesity was defined as BMI greater than the 95th percentile for gender and age.
The study was approved by the institutional human study review committee, and parental consent, as well as child assent for children ≥7 years of age, was obtained.
Data analysis
Data are presented as means±SD unless otherwise indicated. All analyses were conducted using SPSS software (version 11.5; SPPS, Chicago, Ill.). Since plasma CRP and IL-6 levels were not normally distributed, logarithmic transformation was applied. Comparisons of demographics according to group assignment were made with independent t tests or analysis of variance followed by post hoc comparisons, with p values adjusted for unequal variances when appropriate (Levene’s test for equality of variances), or chi square (χ 2) analyses with Fisher’s Exact Test (dichotomous outcomes). Correlations of log CRP levels and log IL-6 with arousal index, AHI, SpO2 nadir, and relBMI were performed using linear regression, followed by calculation of Pearson correlation coefficients. All p values reported are two-tailed with statistical significance set at <0.05.
Results
Two hundred and forty-four children (59% boys), ages 3–17 years (mean 8.9 ± 3.4 years), participated in the study. Of these, 96 children (56 boys) were found to have moderate–severe SDB, 100 children (58 boys) had mild SDB, and 48 children (30 boys) were in the CO group. Subject characteristics are shown in Table 1. There were no significant differences in age and gender among the three groups. However, a significantly higher proportion of obese children was found in the moderate–severe SDB group compared to the control group. As expected, significant differences were found among the three groups in AHI, arousal index, and SpO2 nadir.
Since plasma CRP levels were not normally distributed, logarithmic transformation was applied. Log plasma CRP levels were significantly higher in the moderate–severe SDB group compared to mild SDB and CO (p < 0.0001 and p = 0.0001 respectively; Fig 1a). Log plasma CRP levels were significantly lower among children in group A (SpO2 nadir ≥90) compared to the other three hypoxia-severity groups (p = 0.0016 group A vs group B, p = 0.0004 group A vs group C, p = 0.007 group A vs group D, Fig 1b), with a clear trend of elevation in log CRP levels with parallel decrease in SpO2 nadir (p < 0.0001, Fig. 1b). Log plasma CRP levels were also found to be significantly higher in the obese children compared to the non-obese children (p < 0.0001; Fig. 1c).
a Mean±SD of log CRP levels in 244 children with AHI < 1 (CO), AHI ≥ 1, and <5 (mild SDB), and AHI ≥ 5 (moderate–severe SDB). Log CRP levels in the moderate–severe SDB group differed from mild SDB and CO (p = 0.001 and p < 0.0001 respectively). b Mean±SD of log CRP levels in 244 children with SpO2 nadir ≥90% (Gr A), SpO2 nadir of 80–89% (Gr B), SpO2 nadir of 70–79% (Gr C), and SpO2 nadir <70 (Gr D). Log CRP levels were significantly lower in children in Group A compared to the other three groups (p = 0.0016 group A vs group B, p = 0.0004 group A vs group C, p = 0.007 group A vs group D). c Mean±SD of log CRP levels in obese children compared to non-obese children (p < 0.0001)
Significant correlations were found between log CRP levels and AHI for the whole group (r = 0.30, p < 0.0001), as well as between log CRP levels and arousal index (r = 0.21, p = 0.002). In contrast, a significant negative correlation was found between SpO2 nadir and log CRP levels (r = −0.36, p < 0.0001). These correlations did not improve significantly when we examined only subjects with AHI greater than 5. Significant correlation was found between log CRP and relBMI (r = 0.39, p < 0.0001). However, the correlation with AHI, arousal index, and SpO2 nadir persisted after controlling for relBMI using partial correlation (r = 0.21, p < 0.007 for AHI; r = 0.18, p = 0.02 for arousal index; and r = −0.34, p < 0.0001 for SpO2 nadir).
To further investigate and better control the contribution of relBMI on plasma CRP levels, we performed a sub-analysis of 116 non-obese children in the cohort. Log CRP levels correlated significantly with AHI, SpO2 nadir, and arousal index in the non-obese children (r = 0.20, p = 0.04; r = −0.32, p = 0.001; and r = 0.29, p = 0.005 respectively).
Correlations of log CRP with relBMI, AHI, SpO2 nadir, and arousal index are summarized for the entire cohort, non-obese subjects, and obese subjects in Table 2.
Furthermore, when multiple linear regression was performed for the prediction of log CRP levels using age, sex, relBMI, AHI, SpO2 nadir, and arousal index as covariates, only relBMI and SpO2 nadir were retained in the model. RelBMI accounted for 19% of the variance with SpO2 nadir provided an additional 11% of the variance (adjusted R square, p < 0.0001). When we examined only the non-obese subjects, SpO2 nadir was the only covariate included in the model and accounted for 12% of the variance (adjusted R square, p < 0.0001).
Plasma IL-6 levels were measured in 111 subjects (56% male) out of the entire cohort. The mean age was 8.2 ± 2.8 years (range, 3–17 years). Thirty-eight children (34%) had moderate–severe SDB, 40 (36%) had mild SDB, and 33 (30%) were controls. Subject characteristics and plasma CRP levels are presented in Table 3. Significant correlation was found between log plasma CRP levels and log plasma IL-6 levels (r = 0.56, p < 0.0001). This correlation remained significant both among the obese group (r = 0.44, p = 0.04) and the non-obese group (r = 0.60, p = 0.003).
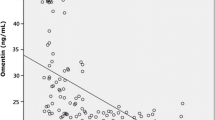
Log plasma IL-6 levels were significantly increased in children with moderate–severe SDB compared to controls (p = 0.03, Fig 2). No significant differences in log plasma IL–6 levels were found between obese and non-obese children. Significant correlation was found between log plasma IL-6 levels and AHI (r = 0.28, p = 0.003), while a significant negative correlation was found between log plasma IL-6 levels and SpO2 nadir (r = −0.24, p = 0.02). When we examined these correlations only among the non-obese subjects (n = 68), only the latter correlation remained significant (r = 0.29, p = 0.03). No correlation was found between log IL-6 levels and relBMI.
In the multiple linear regression for the prediction of log IL-6 levels using age, sex, relBMI, AHI, SpO2 nadir, arousal index, and log CRP as covariates, log CRP was the only covariate included in the model, which accounted for 33% of the variance (adjusted R square, p < 0.0001).
Of note, since acute infection could be theoretically present in some of the children studied (even though none of such children was symptomatic), we analyzed their WBC and platelet counts. None of the subjects participating in our study had elevated WBC counts. Moreover, no significant differences in WBC counts were found between subjects with “high” CRP levels (CRP > 0.3 mg/dl) compared to “low” CRP levels (CRP < 0.3 mg/dl; 6,876 ± 1,870/mm3 vs 6,717 ± 1,785/mm3, respectively; p not significant). Similarly, platelet counts, a sensitive acute phase reactant marker, failed to reveal any significant differences between subjects with high CRP levels compared to low CRP levels (323.6±66.6×103/mm3 vs 317.6±75.9×103/mm3, respectively; p not significant).
Discussion
This study, conducted in a large cohort of snoring children, confirms our previous report that children with moderate–severe SDB have elevated plasma CRP levels compared to children with mild SDB and controls, and that plasma CRP levels correlate significantly with SDB severity independently of obesity. Moreover, we now show in this study that children with moderate–severe SDB have elevated plasma IL-6 levels, another marker of inflammation that modulates CRP synthesis, and that IL-6 concentrations correlate only with disease severity and not with the degree of adiposity. Thus, SDB, primarily through hypoxemia, imposes an independent effect (in addition to obesity) on subclinical inflammatory processes, suggesting a role for SDB in modifying the risk for cardiovascular morbidity in early life.
SDB in adults is now widely recognized as an important and independent risk factor for cardiovascular morbidity, including hypertension, ischemic heart disease, and cerebrovascular accidents [26, 27]. One of the potential mechanisms linking the strong association between SDB and cardiovascular morbidity postulates that SDB-induced hypoxic stress modulates the expression of circulating inflammatory mediators and may lead to accelerated atherogenesis. Compared to adults, children may be a more suitable population to examine the role of SDB in cardiovascular outcomes, especially when using biological markers. Indeed, children are less likely to suffer from preexisting cardiovascular conditions and/or other confounders. However, obesity, one of the major confounders in investigating cardiovascular outcomes, has reached global epidemic proportions especially in the US [28]. Obesity in childhood is a strong predictor for the development of cardiovascular consequences in adulthood and is associated with earlier emergence of insulin resistance, hypertension, and dyslipidemia, all of which constitute potential risks for the development of cardiovascular morbidity [29, 30]. Using a large pediatric population with a wide range of SDB severity and BMI clearly improved our ability to identify the relative contributions of each potential risk factor to CRP and IL-6, and thus permitted a more thorough and reliable assessment of the potential role played by SDB in cardiovascular outcomes. Indeed, while a considerable proportion of our total sample would be considered obese (52%), we were able to conduct an adequately powered sub-analysis in non-obese children. This sub-analysis confirmed our findings for the entire cohort and showed that plasma CRP levels are increased in children with SDB and correlate with several parameters of disease severity, namely AHI, the degree of hypoxemia, and the degree of sleep disruption. These results concur with our previous report and with a recent report by Larkin et al. [10, 11] showing a dose–response relationship between SDB and CRP. However, these findings are in contrast to the report by Kaditis et al. [12], who described normal CRP levels in a cohort of Greek children with SDB. While obesity could have been a reason for the discrepancy between these different studies, the current study negates such possibility. However, both genetic factors (e.g., black race, apolipoprotein E subtypes) [31, 32] and environmental differences (i.e., reduced physical activity, high fat diet), rather than the degree of adiposity per se, could underlie the differences in the findings of these studies [33].
An important issue pertaining to this and other studies on CRP in SDB deserves a comment. Overall, plasma CRP levels were within the normal range, i.e., the range considered as not indicative of an acute infection or inflammatory process (normative range for our laboratory 0.05–0.49 mg/dl). However, in contrast to customary clinical practice reference values, plasma CRP levels >0.3 mg/dl should be viewed as bearing an increased risk for cardiovascular morbidity [30].
In a separate study from our laboratory, we found that children with SDB, similar to adults with SDB [34], have elevated plasma levels of adhesion molecules [7] and that such elevations correlate with the degree of hypoxemia and of sleep disruption and/or fragmentation, providing additional support to the notion that inflammatory processes associated with atherogenesis are elicited by SDB in children and may ultimately accelerate the atherosclerosis process in this population.
The role of the intermittent hypoxemia associated with SDB in the activation of inflammatory cascades and modulation of circulating CRP levels was further consolidated in the present study. Indeed, as shown in Fig. 1b, we found a dose–response relationship between hypoxemia and CRP levels, as well as a significant correlation between plasma IL-6 levels and SpO2 nadir. The intermittent hypoxemia and reoxygenation typically seen in SDB may trigger oxidative stress pathways and the release of inflammatory cytokines [35]. Such elevations in inflammatory cytokines including tumor necrosis factor alpha and IL-6 have been reported in adults with SDB [36]. Since plasma IL-6 levels in our cohort showed correlation only with SDB severity, primarily with hypoxemia, and not with the degree of adiposity, it is possible that the inflammatory pathways elicited by hypoxemia and involving IL-6 and CRP are distinct from the inflammatory pathways elicited by obesity, which ultimately contribute to CRP elevation.
The absence of an association between relBMI and plasma IL-6 levels was surprising considering previous reports [16, 17, 37]. While we cannot adequately explain such discrepancy, we can surmise that the two populations studied being different, i.e., normal children and snoring children, the relationship between ponderal index and inflammation in snoring children may be overcome by the stronger effect of snoring on IL-6. Indeed, we have also noticed such effect in the context of quality of life in snoring children and obese children, whereby snoring appears to supersede any effect of obesity on quality of life scales [38].
Sleep fragmentation is another potential mechanism that may mediate the association between SDB and cardiovascular morbidity. Recent data has shown that sleep deprivation is associated with changes in several biological markers including IL-6 and CRP [39, 40]. In the current study and in our previous report, we show the contribution, albeit modest, of sleep fragmentation to plasma CRP levels.
Although a major strength of our study lies in the large sample size and the wide range of age, BMI, and SDB disease severity, the possible effects of genetic determinants and of environmental factors such as exercise and diet on the cardiovascular morbidity in snoring children has not been studied and deserves further investigation.
In summary, children with SDB display significant severity-dependent increases in plasma CRP and IL-6 levels, which are independent from obesity. Such findings support the hypothesis that SDB in childhood imposes an independent risk for development of subclinical inflammation, which in turn may promote the onset and progression rate of atherosclerosis, particularly in risk-prone populations.
References
Ali NJ, Pitson D, Stardling JR (1993) Snoring, sleep disturbances and behavior in 4–5 year olds. Arch Dis Child 68:360–366
Rosen CL, Larkin EK, Kirchner HL, Emancipator JL, Bivins SF, Surovec SA, Martin RJ, Redline S (2003) Prevalence and risk factors for sleep disordered breathing in 8–11 year old children: association with race and prematurity. J Pediatr 142:383–389
Marcus CL, Greene MG, Carroll JL (1998) Blood pressure in children with obstructive sleep apnea. Am J Respir Crit Care Med 157:1098–1103
Amin RS, Carroll JL, Jeffries JL, Grone C, Bean JA, Chini B, Bokulic R, Daniels SR (2004) Twenty-four hour ambulatory blood pressure in children with sleep-disordered breathing. Am J Respir Crit Care Med 169:950–956
Amin RS, Kimball TR, Bean JA, Jeffries JL, Willging JP, Cotton RT, Witt SA, Glascock BJ, Daniels SR (2002) Left ventricular hypertrophy and abnormal ventricular geometry in children and adolescents with obstructive sleep apnea. Am J Respir Crit Care Med 165:1395–1399
Aljadeff G, Gozal S, Schechtman VL, Burrell B, Harper RM, Ward SL (1997) Heart rate variability in children with obstructive sleep apnea. Sleep 20:151–157
O’Brien LM, Serpero LD, Tauman R, Gozal D (2006) Plasma adhesion molecules in children with sleep-disordered breathing. Chest 129:947–953
Ridker PM, Hennekens CH, Buring JE, Rifai N (2000) C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med 342:836–843
Pasceri V, Willerson JT, Yeh ET (2000) Direct proinflammatory effect of C-reactive protein on human endothelial cells. Circulation 102:2165–2168
Tauman R, Ivanenko A, O’Brien LM, Gozal D (2004) Plasma C-reactive protein among children with sleep-disordered breathing. Pediatrics 113:e564–e569
Larkin EK, Rosen CL, Kirchner HL, Storfer-Isser A, Emancipator JL, Johnson NL, Zambito AMV, Tracy RP, Jenny NS, Redline S (2005) Variation of C-reactive protein levels in adolescents association with sleep-disordered breathing and sleep duration. Circulation 111:1978–1984
Kaditis AG, Alexopoulos EI, Kalampouka E, Kostadima E, germanis A, Zintzaras E, Gourgouliannis K (2005) Morning levels of C-reactive protein in children with obstructive sleep-disordered breathing. Am J Respir Crit Care Med 171:282–286
Kelly A, Marcus CL (2005) Childhood obesity inflammation and apnea—what is the future for our children? Am J Respir Crit Care Med 171:202–203
Castell J, Gomez-Lechion M, David M (1990) Acute phase response of human hepatocyte: regulation of acute phase protein synthesis by interleukin-6. Hepatology 12:1179–1186
Haddy N, Sass C, Droesch S, Zaiou M, Siest G, Ponthieux A, Lambert D, Visvikis S (2003) IL-6, TNF-alpha and atherosclerosis risk indicators in a healthy family population: the STANISLAS cohort. Atherosclerosis 170:277–283
Roytblat L, Rachinsky M, Fisher A, Greemberg L, Shapira Y, Douvdevani A, Gelman S (2000) Raised interleukin-6 levels in obese patients. Obes Res 8:673–675
Kern PA, Ranganathan S, Li C, Wood L, Ranganathan G (2001) Adipose tissue tumor necrosis factor and interleukin-6 expression in human obesity and insulin resistance. Am J Physiol Endocrinol Metab 280:E745–E751
Vgontzas AN, Papanicolaou DA, Bixler EO, Hopper K, Lotsikas A, Lin HM, Kales A, Chrousos GP (2000) Sleep apnea and daytime sleepiness and fatigue: relation to visceral obesity, insulin resistance, and hypercytokinemia. J Clin Endocrinol Metab 85:1151–1158
Yokoe T, Minoguchi K, Matsuo H, Oda N, Minoguchi H, Yoshino G, Hirano T, Adachi M (2003) Elevated levels of C-reactive protein and interleukin-6 in patients with obstructive sleep apnea syndrome are decreased by nasal continuous positive airway pressure. Circulation 107:1129–1134
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques and scoring systems for sleep stages of human subject. Publication no. 204. National Institutes of Health, Washington DC
Montgomery-Downs HE, O’Brien LM, Gulliver TE, Gozal D (2006) Polysomnographic characteristics in normal preschool and early school-age children. Pediatrics 117:741–753
American Thoracic Society (1996) Standards and indications for cardiopulmonary sleep studies in children. Am J Respir Crit Care Med 153:866–878
No authors listed (1992) EEG arousals: scoring and rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:173–184
Mograss MA, Ducharme FM, Brouillette RT (1994) Movement/arousals. Description, classification, and relationship to sleep apnea in children. Am J Respir Crit Care Med 150:1690–1696
Hammer LD, Kraemer HC, Wilson DM, Ritter PL, Dornbusch SM (1991) Standardized percentile curves of body mass index for children and adolescents. Am J Dis Child 145:259–263
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D’Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2000) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health. JAMA 283:1829–1836
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342:1378–1384
Ogden CL, Flegal KM, Carroll MD, Johnson CL (2002) Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA 288:1728–1732
Nishina M, Kikuchi T, Yamazaki H, Kameda K, Hiura M, Uchiyama M (2003) Relationship among systolic blood pressure, serum insulin and leptin, and visceral fat accumulation in obese children. Hypertens Res 26:281–288
Berenson GS, Srinivasan SR, Bao W, Newman WP, Tracy RE, Wattigney WA (1998) Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med 338:1650–1656
Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G (1999) Risk factors for sleep-disordered breathing in children. Associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med 159:1527–1532
Larkin EK, Patel SR, Redline S, Mignot E, Elston RC, Hallmayer J (2006) Apolipoprotein E and obstructive sleep apnea: evaluating whether a candidate gene explains a linkage peak. Genet Epidemiol 30:101–110
Carmelli D, Cardon LR, Fabsitz R (1994) Clustering of hypertension, diabetes, and obesity in adult male twins: same genes or same environments? Am J Hum Genet 55:566–573
El-Solh AA, Mador MJ, Sikka P, Dhillon RS, Amsterdam D, Grant BJ (2002) Adhesion molecules in patients with coronary artery disease and moderate-to-severe obstructive sleep apnea. Chest 121:1541–1547
Christou K, Markoulis N, Moulas AN, Pastaka C, Gourgoulianis KI (2003) Reactive oxygen metabolites (ROMs) as an index of oxidative stress in obstructive sleep apnea patients. Sleep Breath 7:105–110
Vgontzas AN, Papanicolaou DA, Bixler EO, Kales A, Tyson K, Chrousos GP (1997) Elevation of plasma cytokines in disorders of excessive daytime sleepiness: role of sleep disturbance and obesity. J Clin Endocrinol Metab 82:1313–1316
Gallistl S, Sudi KM, Aigner R, Borkenstein M (2001) Changes in serum interleukin 6 concentration in obese children and adolescents during weight reduction program. Int J Obes Relat Metab Disord 25:1640–1643
Crabtree V, Varni JW, Gozal D (2004) Quality of life and depressive symptoms in children with suspected sleep-disordered breathing. Sleep 27:1131–1138
Shearer WT, Reuben JM, Mullington JM, Price NJ, Lee BN, Smith EO, Szuba MP, Van Dongen HP, Dinges DF (2001) Soluble TNF-alpha receptor 1 and IL-6 plasma levels in humans subjected to the sleep deprivation model of spaceflight. J Allergy Clin Immunol 107:165–170
Meier-Ewert HK, Ridker PM, Rifai N, Regan MM, Price N, Dinges DF, Mullington JM (2004) Effect of sleep loss on C-reactive protein, an inflammatory marker of cardiovascular risk. J Am Coll Cardiol 43:678–683
Acknowledgements
This study was supported by the National Institutes of Health (grant HL-65270), The Children’s Foundation Endowment for Sleep Research, and the Commonwealth of Kentucky Challenge for Excellence Trust Fund. RT was supported by an Ohio Valley American Heart Association Fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tauman, R., O’Brien, L.M. & Gozal, D. Hypoxemia and obesity modulate plasma C-reactive protein and interleukin-6 levels in sleep-disordered breathing. Sleep Breath 11, 77–84 (2007). https://doi.org/10.1007/s11325-006-0085-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-006-0085-7