Abstract
We designed this study to assess the signal failure and sensor loss of unattended type 2 comprehensive polysomnography (PSG) and compared that with in-lab attended PSG. Type 2 PSG was performed for 41 patients. The signal failure was estimated and compared to the signal failure in 60 patients for the in-lab PSGs. The signal failure in each individual electroencephalographic (EEG) channel, complete EEG signals, electro-oculography (EOG), naso–oral flow, and thoracic belt were significantly greater in the unattended sleep studies. The failure rate for the different signals ranged from 0.128 min in electrocardiography (EKG) to 67.36 min in the thoracic belt signal. However, that did not affect the success rate of the studies. Acceptable scorable data was available in 97% of the performed unattended PSGs. Unattended type 2 sleep studies can be performed for clinical use in the evaluation of sleep disordered breathing with low signal failure and sensor loss if the proper hook-up procedure was followed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep disordered breathing (SDB) is a relatively common problem [1]. The standard approach to diagnosing SDB is in-lab, technician-attended polysomnography (PSG). However, proper in-lab PSG is not readily available to all institutes, which results in improper patient evaluation and long waiting lists for patients needing diagnostic sleep study. The availability of the needed diagnostic equipment is one obstacle; however, in my view, the main obstacle facing practicing doctors in developing countries is the availability of an adequate number of trained sleep technologists who can run the service in the sleep disorder centers (SDCs) on a full-time basis. As a result, some practicing doctors relied on their clinical judgment for diagnosing SDB and adopted the practice of continuous positive airway pressure (CPAP) titration as an in-patient procedure under pulse oximetry monitoring and thereby prescribed CPAP without proper evaluation [2]. To help solve the problem of the availability of proper SDCs and an adequate number of trained technologists needed to run the service, portable monitoring (PM) has been proposed as an alternative to in-lab PSG. The proponents of PM suggest that it is less time-consuming and requires less expertise. The term “PM” covers a wide range of devices that can record as much data as an attended in-lab PSG does or one single channel only, such as pulse oximetry. The American Sleep Disorders Association (ASDA) classified sleep monitoring into four types [3]. Type 1 (standard in-lab attended PSG) was considered to be the reference standard to which other monitoring types are compared; type 2, comprehensive portable PSG, which incorporates a minimum of seven channels, including neuro-cardio-respiratory monitoring; type 3, which incorporates a minimum of four channels, including cardio-respiratory monitoring; and type 4, which incorporates one or two channels, typically, oxygen saturation or air flow.
A number of factors of can interfere with the signal of PSG recordings, such as the improper use of sensors, improper filtering of signals, and excessive movement of the studied subject. Unlike attended PSGs, trained personnel are not available during unattended studies to identify and resolve technical pitfalls during the study.
In our experience, failed studies due to technical issues are rare in attended PSGs since a technologist can correct most of these problems during the study. However, the failure rate is unpredictable in unattended studies. A limited number of studies addressed the issue of data loss in unattended type 2 PSG and, to our knowledge, only one study directly addressed the issue of sensor loss in this type of PSG [4]. In that study, a large number of unattended PSGs were performed, but no control group was included. We designed this study to assess the signal failure and sensor loss of unattended type 2 comprehensive sleep studies to compare with in-lab attended PSG and to describe the technique we used for the hook-up of patients in the unattended studies to minimize signal loss.
Materials and methods
This study was approved by the Ethics Committee of the College of Medicine at King Saud University, Saudi Arabia and informed consents were taken from all participants. The study was performed between February 2001 and January 2002.
Study population
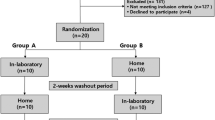
The participants for the unattended sleep studies were consecutive patients admitted to the cardiology service and were clinically suspected during their hospital stay to have SDB. Before being discharged, the patients were asked to stay for one more night for sleep study. They were kept in a quiet private room in the ward for the overnight sleep study. Type 2 unattended PSG was carried out for each patient. Patients with any of the following were excluded: confused patients, those who received sedatives or narcotics within 48 h of the overnight sleep study, or patients who underwent any surgical intervention during their hospital stay. The sleep study technique was explained to the patients in detail. The patients were instructed not to sleep during the day time and not to take any stimulants (tea, coffee, soda) after midday.
The participants of the attended sleep studies were consecutive patients referred to the SDC for the first time with a clinical suspicion of SDB.
Polysomnography
The unattended PSG tests were recorded using Alice 4 diagnostic equipment from Respironics Inc., Murrysville, PA, USA. The data was stored using a PCMCIA (Personal Computer Memory Card International Association) flash disk (approximately 20 MB per study). The data was then downloaded onto an IBM personal computer. The system contained a lead crystalline display (LCD) for visualizing signals after hook-up, and to check the impedance. During PSG, the following parameters were monitored: brain activity by four electroencephalographic (EEG) placements (C1–A4, C2–A3, O1–A4, and O2–A3); muscle tone by chin electromyography (EMG); eye movements by electro-oculography (EOG); heart rate by electrocardiography (EKG); oxygen saturation by finger pulse oximeter; chest and abdominal wall movements by thoracic and abdominal belts; naso-oral air flow by thermistor; sleep position by position sensor; and snoring by microphone. Leg EMG was not recorded. The hook-up process was performed by a trained technologist. Several unattended studies were initially performed on the volunteers to explore the possible technical problems and to detect the causes of failure of individual signals. The hook-up technique was modified based on the preliminary results in order to minimize sensor loss and signal failure. The sensors were attached with collodion glue for EEG, chin EMG, EOG, mastoid reference, and ground references, in addition to tape and gauze. a crepe bandage was wrapped around the patient’s head, extending down to the chin, to minimize the risk of sensor loss. While fixing the EOG electrode, the patient was asked to close their eyes and the gauze was put over their eyes until the application was completed. The pulse oximeter was affixed using double-sided tape. For EKG, disposable self-adhesive electrodes were used. Signals were visualized on the LCD and the impedance values were checked. Sensor positions were adjusted to improve the signal quality, and electrodes were replaced if the impedance values were above 5 kΩ. At the end of the hook-up process, the technologist completed a signal verification form. Low- and high-frequency filters were set prior to acquisition. However, the system allows re-filtering of the data after acquisition.
The hook-up process took approximately 1 h. Before leaving, the technician assured the comfort of the patient and instructed him/her not to remove or manipulate any of the sensors. The attending nursing staff in the ward who had no training on sleep studies were instructed not to manipulate the sensors or equipment. The dinner meal was given to the patients before hook-up. After the hook-up process, patients were allowed to drink but not to eat to minimize the risk of losing the naso-oral flow signal. The machine was programmed to start recording at 23:00 and end recording at 06:00. The technologist returned to the hospital at 07:00 to un-hook the patient.
The attended PSG studies were performed in the SDC and Alice 4 diagnostic equipment was used for data acquisition. A trained technologist connected the participants to the monitor and stayed in the SDC throughout the study, monitoring the recording in the control room. During PSG, the following parameters were monitored: four EEG placements (C1–A4, C2–A3, O1–A4, and O2–A3); muscle tone and leg movements by chin and leg EMG; eye movements by EOG; heart rate by EKG; oxygen saturation by finger pulse oximeter; chest and abdominal wall movements by thoracic and abdominal belts; air flow by thermistor; sleep position by position sensor; and snoring by microphone. The electrodes were attached with collodion glue for EEG, and with tape for EMG, mastoid reference, ground references, and EKG. For bearded men, collodion glue was used to attach the chin EMG electrodes. Recording started at approximately 10:00 and ended at approximately 06:00.
Analysis and scoring of PSG data
Page-by-page analysis and scoring of the electronic raw data was done manually by the same person to determine the total time in bed (TIB), total sleep time (TST), sleep efficiency, and arousal index [5, 6]. Obstructive apneas were identified as a decrease in peak inspiratory flow to below 10% of the surrounding baseline for at least 10 s; central apneas were defined as the absence of flow and rib/thoracic movement during the event for at least 10 s; and hypopneas were defined as any visually appreciable decrease in flow amplitude for two or more consecutive breaths followed by arousal or oxygen desaturation of at least 3%. To calculate the apnea hypopnea index (AHI), the total number of respiratory events (apneas and hypopneas) was divided by the TST. The failure rate of each EEG electrode, absence of all EEG signals (complete EEG failure), EOG failure, pulse oximeter failure, EKG failure, and respiratory signal for air flow were checked manually epoch by epoch and documented. Reports were generated using the Alice 4 software.
Study quality
We adopted and modified the criteria used in the Sleep Heart Health Study (SHHS) project to define study failure [4]. Studies were considered a failure if they lack one or more of the following: 4 h of oximetry data; 4 h of contiguous data from either abdominal, chest, or thermocouple sensors; or an EEG signal of good quality to allow sleep stage scoring. Insufficient TST was defined as TST less than 200 min.
Statistical analysis
The data were expressed as mean±standard error (SE) in the text and tables. Student’s t-test was used to compare the two groups. If the normality test failed, the rank sum test was used. Sigma Stat, Version 3 (SPSS Inc., Chicago, IL, USA) statistical software was used for the analysis.
Results
The 41 patients who underwent the unattended part of the study included 34 men and seven women, with a mean age of 51.4±1.7 years and a range of 27–80 years. In one case, the study was performed as per our protocol, but the data was not stored on the PCMCIA card. Therefore, complete data was available for only 40 patients (97.6%). On the other hand, 60 patients completed the attended part of the study (43 men and 17 women). The mean age was 49.9±1.8 years with a range of 16–80 years. Table 1 shows the demographic and PSG characteristics of both groups. Body mass index (BMI), TST, and TIB were not different between the groups. Sleep efficiency was better in the attended group.
Table 2 demonstrates the duration of signal failure in both groups. Individual EEG signal failure as well as complete EEG signal failure were significantly more common in the unattended sleep studies. However, none of the sleep studies met the adopted failure criteria. Signal failure was also significantly more in the EOG, flow, and thoracic belt signals. During the unattended studies, chin EMG failure was more among males (5.6±4.6 min) versus no failure for females. However, this difference was not of statistical significance.
Based on the SHHS criteria to define sleep study failure, all recorded unattended sleep studies performed in this project were successful. One patient damaged the naso-oral flow sensor during one of the unattended studies.
Discussion
Although type 2 monitors should, theoretically, most resemble in-lab polysomnography (PSG) in calculating the apnea hypopnea index (AHI) and scoring sleep stages, relatively few published data addresses this issue [7]. In contrast, data loss in type 3 monitors recording simple cardio-respiratory parameters was reported to be low ranging from 3% to 18% [3, 8–10]. However, as type 2 monitors record both cardio-respiratory and neurological signals, a high rate of data loss in the unattended setting has been a concern. Data loss in type 2 monitors was reported in three studies only. One study [11] reported no loss of any home monitoring and a scorable data set in more than 95% of epochs. Another study [12] reported a 20% loss of data. The success rate in the Sleep Heart Health Study (SHHS) project was 90.6% [4].
The present study demonstrates that type 2 unattended sleep study is a successful and reliable way to monitor patients with suspected sleep disordered breathing (SDB). More than 97% of the performed unattended studies were successful in obtaining more than 4 h of adequate neuro-cardio-respiratory data (in one study, data was not recorded). As we did not record leg movements, we cannot draw conclusions about the success rate in leg electromyography (EMG). A previously published study of unattended type 2 studies recording bilateral anterior tibialis EMG activity reported a scorable signal in more than 95% of epochs [11].
Our results showed that unattended type 2 comprehensive sleep studies had a statistically higher failure rate in most recorded signals; however, this difference may not be of clinical significance. Naso-oral flow signal had a relatively high failure rate compared to other signals. This finding agrees with Portier et al. [12], who reported an 11% flow signal failure.
The differences in study quality among different trials may be attributed to the fixation technique used and the guidance given to the patients. The overall low signal failure can be attributed to the technique we used for hook-up. Chin EMG is one of the electrodes causing problems during PSG in bearded men. We recommend using collodion to attach chin EMG electrodes in this category of patients. We described the technique we used for the hook-up process in the unattended sleep studies, which was slightly different from the attended studies. We lost one of the unattended studies due to failure of the equipment to store data, which stresses the importance of considering the reliability of both the hardware as well as the software when selecting the portable monitoring (PM) device.
Sleep efficiency was better during in-lab PSG; this could be related to the patient’s concerns about safety or equipment failure during unattended studies. In attended studies, the presence of a sleep technologist gives reassurance to the patient.
Type 2 unattended PSG is a reliable diagnostic technique with a high success rate in patients with SDB. We advocate using such techniques in patients with suspected SDB. Such application will decrease the load on established sleep disorder centers (SDC)s and help institutes that do not have a designated SDC to perform good quality and reliable studies. Such techniques can also be useful in patients who need follow-up PSG tests to assess response to treatment instead of waiting for few more months for the availability of a repeat study.
One of the limitations of the current study is the fact that unattended PSG was not performed at home. However, we tried to eliminate this problem by performing studies in a quiet private room in the general ward and instructing the nursing staff at night not to interfere with data acquisition.
In summary, our findings demonstrate that unattended type 2 sleep studies can be performed for clinical use in the evaluation of suspected SDB with low signal failure and sensor loss if proper a hook-up procedure was followed.
References
Young T, Palta M, Dempesy J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Bahammam A, Rahman AA (2000) Hospital nights utilized for CPAP titration in obstructive sleep apnea syndrome patients in the absence of a proper sleep disorders center. Ann Saudi Med 20:83–85
Ferber R, Millman R, Coppola M, Fleetham J, Murray CF, Iber C, McCall V, Nino-Murcia G, Pressman M, Sanders M, Strohl K, Votteri B, Williams B (1994) ASDA standards of practice: portable recording in the assessment of obstructive sleep apnea. Sleep 17:378–392
Kapur VK, Rapoport DM, Sanders MH, Enright P, Hill J, Iber C, Romaniuk J (2000) Rates of sensor loss in unattended home polysomnography: the influence of age, gender, obesity, and sleep-disordered breathing. Sleep 23:1–7
Rechtschaffen A, Kales A (eds) (1968) A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. National Institutes of Health (NIH) publication number 204, US Government Printing Office, Washington, DC
American Sleep Disorders Association, Atlas Task Force (1992) EEG arousals: scoring rules and examples. Sleep 15:174–184
Chesson AL, Berry BR, Pack A (2003) Practice parameters for the use of portable monitoring in the investigation of suspected obstructive sleep apnea in adults. Sleep 26:907–913
Ancoli-Israel S, Mason W, Coy TV, Stepnowsky C, Clausen JL, Dimsdale J (1997) Evaluation of sleep disordered breathing with unattended recording: the night watch system. J Med Eng Technol 21:10–14
White DP, Gib TJ, Wall JM, Westbrook PR (1995) Assessment of accuracy and analysis time of a novel device to monitor sleep and breathing in the home. Sleep 18:115–126
Whittle AT, Finch SP, Mortimore IL, MacKay TW, Douglas NJ (1997) Use of home sleep studies for diagnosis of the sleep apnoea/hypopnoea syndrome. Thorax 52:1068–1073
Fry J, DiPhillibo MA, Curran K, Goldgerg R, Baran S (1998) Full polysomnography in the home. Sleep 21:635–642
Portier F, Portmann A, Czernichow P, Vascaut L, Devin E, Benhamou D, Cuvelier A, Muir JF (2000) Evaluation of home versus laboratory polysomnography in the diagnosis of sleep apnea syndrome. Am J Respir Crit Care Med 162:814–818
Acknowledgements
I would like to thank the technologists at the Sleep Disorders Center, Mrs. Marila Bien, Ms. Eden Pierella, and Mrs. Saji Thomas for their great help. This study was supported by a grant from King Abdulaziz City for Science and Technology (KACST), Riyadh, Saudi Arabia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
BaHammam, A.S. Signal failure of type 2 comprehensive unattended sleep studies in patients with suspected respiratory sleep disordered breathing. Sleep Breath 9, 7–11 (2005). https://doi.org/10.1007/s11325-005-0001-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-005-0001-6