Abstract
Purpose
[18F]fluorodeoxysorbitol ([18F]FDS) is the first radiopharmaceutical specific for a category of bacteria and has the potential to specifically detect Enterobacteriaceae infections. The purpose of this study was to testify the safety and investigate the biodistribution and radiation dosimetry of [18F]FDS in healthy human bodies.
Procedures
Six healthy subjects were intravenously injected with 320–520 MBq [18F]FDS. On each subject, 21 whole-body emission scans and a brain scan were conducted at settled time points within the next 4 h. Residence time for each source organ was determined by multi-exponential regression. Absorbed doses for target organs and effective dose were calculated via OLINDA/EXM.
Results
No adverse events due to [18F]FDS injection were observed in the study. The tracer was cleared rapidly from the blood pool through the urinary system. A small portion was cleared into the gut through the hepatobiliary system. The effective dose (ED) was estimated to be 0.021 ± 0.001 mSv/MBq. The organ receiving the highest absorbed dose was the urinary bladder wall (0.25 ± 0.03 mSv/MBq).
Conclusions
[18F]FDS is safe and well tolerated. The effective dose was comparable to that of other F-18 labeled radiotracers. [18F]FDS is suitable for human use from a radiation dosimetry perspective.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bacterial infection is a major cause of morbidity and mortality around the world, in which billions of dollars are spent annually fighting infection. Unfortunately, as more multidrug-resistant bacteria emerge and more patients suffer from immunosuppression, the case is increasingly urgent. However, there have been almost no revolutionary advancements in the diagnosis of infection for many years [1].
Microbial culturing, the gold standard for infection diagnosis, is substantially hampered by the difficulties in assessing early-stage infections and deep-seated foci. Morphological imaging techniques (ultrasound, X-ray computed tomography (CT), and magnetic resonance imaging) can only depict late-stage anatomical changes caused by infection. In contrast, nuclear medicine imaging is able to identify infectious disease via immune cell trafficking or bacteria-specific metabolism; thus, various physiopathological processes can be detected in their preliminary stage before the infections manifest anatomically.
There has been a long list of putative radiopharmaceuticals ever since [67Ga] citrate was adopted as first generation radiotracer for infection imaging. This list includes [67Ga] citrate [2], radiolabeled autologous leukocytes [3], radiolabeled antigranulocyte antibodies [4], radiolabeled cytokines [5], and [18F]FDG [6], which were developed to describe the inflammation processes mainly by observing the nonspecific uptake mechanisms, such as blood supply expansion, vascular permeability increase, and inflammatory cell aggregation. The main disadvantage of these probes, however, is their inability to distinguish infection from sterile inflammation. Hence, the second-generation pathogen-specific imaging probes, namely radiolabeled antimicrobial peptide (AMP) [7], siderophore [8], chitinase [9], 1-(2′-deoxy-2′-fluoro-β-D-arabinofuranosyl)-5-iodouracil (FIAU) [10], and maltodextrin-based probes [11, 12], were developed to compensate for this deficiency in the first generation probes.
[18F]fluorodeoxysorbitol ([18F]FDS) is an analog of sorbitol, an Enterobacteriaceae metabolic substrate. In vitro and in vivo studies demonstrated that it avidly accumulates in Enterobacteriaceae infection foci, with little uptake in mammalian cells, sterile inflammation foci, or infection due to other bacteria species [13]. It holds tremendous potential for identifying and monitoring known or suspected infection caused by Enterobacteriaceae. We present here a preliminary study of [18F]FDS, performed on healthy volunteers, to evaluate the safety, biodistribution, and radiation dosimetry of this radiotracer.
Materials and Methods
Study Design and Population
All procedures of the study were approved by the Institutional Review Board of Peking Union Medical College Hospital. The study protocol is depicted in Fig. 1. All subjects signed written informed consent before study participation. The inclusion criteria demanded that all subjects should be above 18 years and should submit a health report, covering their medical history, physical examination, electrocardiogram, urinalysis, and standard blood tests. The exclusion criteria included pregnancy and breastfeeding. Six healthy volunteers (three men, three women) were enrolled in the study, while the average age was 42.5 ± 10.1 years, ranging from 27 to 57 years, whose average weight was 69.2 ± 9.9 kg, ranging from 58 to 81 kg (Table 1). No specific fasting or food protocol was required before the procedure.
Safety Assessment
Patient safety was assessed and graded according to Common Terminology Criteria for Adverse Events (version 4.03) [14], electrocardiograms, physical examination, and vital signs (blood pressure, respiratory rate, heart rate, body temperature). Within the first 72 h after [18F]FDS injection, the research team kept phone contact with each subject monitoring their adverse event (AE) responses.
Radiopharmaceutical Preparation
2-Deoxy-2-[18F]fluoro-D-glucose ([18F]FDG) (Beijing PET PET-MF-2V-IT-I module) was prepared as previously reported [15]. The product’s average radiochemical purity was 99 %, and its specific activity was greater than 37 GBq/μmol.
[18F]FDS was synthesized from [18F]FDG, similar to the method previously reported [16]. Briefly, [18F]FDG was firstly reduced with sodium borohydride at 45 °C under N2 bubbling for 15 min. When the reaction was complete, a diluted hydrochloric acid and sodium acetate (1.4 ml) buffer was added to the product to adjust its pH value to 6.5–7.5. Subsequently, the solution was filtered directly into a sterile product vial (10 ml size) through a Sep-Pak Alumina N cartridge with a sterile Millipore filter (0.22 μm, 4 mm).
Radiochemical purity and identity of the final product were confirmed comparing its Rf (retardation factor) to that of the standard FDS (ABX Corporation) via radio-TLC. Its specific activity was greater than 29.6 ± 6.5 GBq/μmol based on the intermediate [18F]FDG. And as radio-TLC reflected, its radiochemical purity was greater than 99 %.
PET/CT Acquisition
This research was carried out on a Biograph mCT positron emission tomography (PET)/CT scanner (Siemens Healthcare Molecular Imaging, Knoxville, USA). Before [18F]FDS administration, a low-dose CT scan from the base of their skull to proximate thigh (120 KeV; Care Dose4D technique for effective mAs; 0.8 pitch; 5 mm slice thickness; 0.5 s rotation time) was obtained on each subject for the purpose of positioning and attenuation correction.
Secondly, immediately after intravenous injection of 320–520 MBq [18F]FDS (injected volume ranging from 1 to 2 ml), 21 whole-body emission scans plus a brain scan were conducted at various time points within the first 4 h after injection. In regarding to the whole body scans, 17 successive scans (6*5 s/bed position, 5*30 s/bed position, 5*60 s/bed position, and 1*120 s/bed position), each with 6 bed positions, were conducted in the first hour and 4 sequential scans (120 s/bed position) in the following 3 h. As to the brain scan, it was obtained approximately 2 h after injection. The subjects were encouraged to drink water and urinate as much as possible during the breaks after the 1st-hour and 2nd-hour scans to quicken the tracer excretion.
Images were reconstructed using normalization and attenuation-weighted ordered-subsets expectation maximization (2 iterations, 21 subsets), and they were corrected for attenuation, dead time, random events, and scatter.
Biodistribution Assessment and Dosimetry Estimation
Reconstructed whole-body PET images were imported into the free open-source software, MITK Diffusion (available online) [17]. Source organs, including heart contents (defined as the blood in the ventricles), breasts, liver, spleen, gallbladder contents, small intestine contents, kidneys, urinary bladder, and skeleton, which displayed an activity above background were chosen from emission scans. Regions of interest (ROIs) along the boundaries of source organs were delineated manually by a single observer in accordance with what was visualized on CT images. The ROIs were mapped back to the PET images to determine whole-organ activities. The whole-body ROIs, as the ROIs of source organs, were also conducted at different time points to calculate the excreted urine radioactivity, as it was assumed to be the sole route of [18F]FDS excretion. As for the small intestine, gallbladder and urinary bladder, whose organ volume and location might change over time, ROIs were outlined frame-by-frame on the PET images. As for the skeletal system, only the lumbar vertebrae from L1 to L5 were chosen and drawn. Small regions, such as the seminal vesicles and ovaries, were not included in the analysis because they were not easily delineated on CT and were not easily distinguished from their adjacent urinary bladder radioactivity.
Each of these ROIs was saved as individual files and exported into PMOD software (PMOD Technologies Ltd., Zurich, Switzerland) so that the [18F]FDS activities within each ROI could be independently extracted with PMOD. The activities at different time points were documented as a percentage of injected dosage and fitted with multi-exponential functions, which was implemented in the OLINDA/EXM software [18]. Subsequently, time-activity curves (TACs) of source organs were generated. The residence time (τ) was calculated by integrating the resultant exponential function. Red marrow τ was determined from lumbar vertebrae ROIs. The red marrow in the total lumbar spine was assumed to occupy 16.1 % of the total red marrow (ICRP Publication 70) [19]. Urinary bladder τ was determined using the voiding bladder model implemented in OLINDA/EXM software, with a 2-h bladder-voiding interval. The remainder of the body τ was determined by subtraction of the organ τ from the whole body τ. Absorbed dose for all target organs and whole-body effective dose were determined with OLINDA/EXM software using adult male reference phantoms.
Result
Patient Safety
[18F]FDS was found to be safe and well tolerated in all subjects. No serious adverse events (AEs), or discontinuations due to AEs, of [18F]FDS injection were reported in the process of this research. Two of the six subjects (33.3 %) experienced mild to moderate back pain, shoulder discomfort, and muscle spasms, which were most likely attributed to the long imaging time. No significant changes in vital signs or electrocardiograms were observed after [18F]FDS injection.
Biodistribution and Image Characteristics
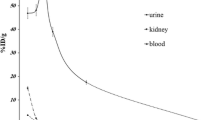
After [18F]FDS administration, radioactivity was initially visualized in the vascular compartment and then rapidly distributed to the liver and kidneys. The radiotracer was mainly excreted through the urinary system. Radioactivity could be visualized in the urinary bladder as early as 5 min after [18F]FDS injection. About 35 % of the injected activity (decay-corrected) was eliminated through the kidneys within the first hour, followed by an additional 37 % within the next 3 h.
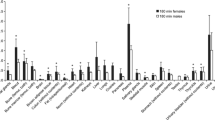
A small portion of the radiotracer was cleared into the gut through the hepatobiliary system. Segmental accumulation of [18F]FDS was observed in the small intestine. The gut radioactivity gradually moved towards the terminal ileum and finally into the ascending colon by the end of acquisition. No obvious uptake was observed in the colon within the first 4 h after injection. The liver, spleen, and breasts demonstrated moderate uptake, while the brain, lungs, thyroid, bone marrow, adrenal glands, and pancreas revealed only mild uptake. Representative images from one female subject are shown in Fig. 2. Decay-corrected TACs of source organs are depicted in Fig. 3. RTs of source organs are summarized in Table 2.
Decay-corrected TACs of source organs (except for the remainder of the body). Values were expressed as percentage injected dose per organ. a High uptake organs (kidneys, liver, and urinary bladder) are illustrated. b Low uptake organs (heart content (blood in the ventricles), breasts, red marrow, spleen, gallbladder, and intestine) are illustrated.
Dosimetry
The absorbed doses for various target organs are summarized in Table 3. The organ which received the highest absorbed dose was the urinary bladder wall (0.25 ± 0.03 mSv/MBq). None of the other organs received an absorbed dose higher than 0.05 mSv/MBq. The effective dose (ED) was estimated to be 0.021 ± 0.001 mSv/MBq.
Discussion
[18F]FDS was first synthesized via reducing [18F]FDG as described by Li, et al. [16]. As Li, et al. intended, this radiopharmaceutical was produced for brain tumor imaging since it showed no significant uptake in normal brain tissue. Later, Weinstein et al. further demonstrated that it can be applied as an analog of sorbitol, the Enterobacteriaceae-specific metabolic substrate, enabling the selective labeling, and tomographic imaging of Enterobacteriaceae in vivo, while showing no intensive uptake in mammalian cells, sterile inflammation foci, or infection by other bacteria species [13]. [18F]FDS is the first radiopharmaceutical with the potential to specifically detect infections due to Enterobacteriaceae. Therapeutic effect monitoring in animal models further proved that it might have broader application in bacterial infections.
However, its use in clinical practice needs to be evaluated in clinical studies. Low bacteria concentration in infection foci and limited bacteria spectrum might remain the major obstacles. Blood stream infection, for instance, in which no obvious infection foci can be found, is an important form of infection in clinical practice. The concentration of bacteria in the blood stream is relatively lower than in an abscess, and this may lead to false-negative images. Furthermore, there are many Gram-positive or Gram-negative bacteria that may yield a false-negative result.
We presented here a preliminary study to evaluate the safety, biodistribution, and radiation dosimetry of [18F]FDS in healthy human volunteers. The results show that [18F]FDS is safe and well tolerated. The stability of this tracer and its possible metabolites in blood circulation would potentially affect the biodistribution of tracer accumulation in tissue and organs, thus dosimetry. As for the in vivo stability in mice, 10 min after intravenous injection, one compound with a higher polarity than [18F]FDS was observed, and the percentage of intact probe was no less than 70 % at the meantime [20]. As for the stability in human blood circulation, it is still to be determined.
The ED of [18F]FDS was estimated to be 0.021 ± 0.001 mSv/MBq, which is comparable with the ED of [18F]FDG (0.019 mSv/MBq), [18F]choline (0.020 mSv/MBq), and [18F]FDOPA (0.025 mSv/MBq) [21]. The Code of Federal Regulations specifies the dose limit of a radioactive drug for research purposes as 30 mSv per administration, with a maximum annual dose of 50 mSv [22]. We estimate that when 370 MBq radioactivity is administered per [18F]FDS session, which is sufficient for a routine scan, the ED would be 7.8 mSv. The effective dose of a low-dose CT scan is 7–8 mSv [23]. The overall radiation exposure, contributed by both PET and CT, is well within the dose limits specified. More frequent, voiding can further reduce the radiation dose since the radiotracer is mainly excreted through the urinary system. It could also be helpful to identify suspected pelvic infections with limited urinary bladder influence.
As [18F]FDS clears much faster than [18F]FDG through urine [16], most organs apart from the urinary system and gut showed relatively low and steady background levels which is good for imaging of Klebsiella pneumoniae infection or deep-seated abscesses. Nonpathogenic Escherichia coli, which inhabits the large intestine, is one of the most commonly seen species of Enterobacteriaceae, while, in the small intestine, it is seldom seen. In our study, segmental accumulation in the gut were mainly located in the small intestine, which moved gradually towards the terminal ileum and finally into the colon by the end of acquisition, while only mild radioactivity could be observed in the large intestine within the first 4 hours after injection. This distribution pattern demonstrated that the uptake in the gut was most likely attributed to hepatobiliary excretion. Hence, the gut flora might not be a major interference in abdominal infection imaging—at least within a limited time after injection in consideration of the special location and migration of segmental gut uptake.
Our study has some limitations. To begin with, body parts above the base of the skull and below the proximate thigh were not included in the scan field. This could mildly influence the calculation of urine excretion. In addition, nonlinear least-squares regression analysis might not be the best method to calculate residence time for the kidneys, gall bladder, and small intestine. An alternative method, such as the trapezoid method, might be better suited for such analysis. Furthermore, patient morphology has a significant influence on dosimetry calculation [24]. The body weight of the subjects in this study range from 58 to 81 kg. The results using standard S factors from OLINDA/EXM could yield some deviations from the realistic values. Additional body weight correction might be a compensatory method and could give more accurate results.
Conclusion
In summary, [18F]FDS injection is safe and well tolerated. The ED of [18F]FDS was 0.021 ± 0.001 mSv/MBq, which is similar to that of other F-18 labeled radiotracers. At the typical clinically administered level (370 MBq), the organ dose and ED are all well within the regulatory limits for human research. Additional human studies are now warranted to evaluate the clinical utility of [18F]FDS in Enterobacteriaceae infection.
References
Wang X, Murthy N (2014) Bacterial imaging comes of age. Sci Transl Med 6:259fs43–259fs43
Littenberg RL, Taketa RM, Alazraki NP et al (1973) Gallium-67 for localization of septic lesions. Ann Intern Med 79:403–406
Erba PA, Martina S, Umberto C et al (2013) Radiolabeled wbc scintigraphy in the diagnostic workup of patients with suspected device-related infections. Jacc Cardiovasc Imaging 6:1075–1086
Pakos EE, Koumoulis HD, Fotopoulos AD et al (2007) Osteomyelitis: antigranulocyte scintigraphy with 99mTc radiolabeled monoclonal antibodies for diagnosis. Radiology 245:732–741
Bleeker-Rovers CP, Rennen HJJM, Boerman OC et al (2007) 99mTc-labeled interleukin 8 for the scintigraphic detection of infection and inflammation: first clinical evaluation. J Nucl Med 48:337–343
Qiu L, Chen Y (2012) The role of 18F-FDG PET or PET/CT in the detection of fever of unknown origin. Eur J Radiol 81:3524–9
Nibbering PH, Welling MM, Paulusma-Annema A et al (2004) 99mTc-labeled UBI 29-41 peptide for monitoring the efficacy of antibacterial agents in mice infected with staphylococcus aureus. J Nucl Med 45:321–326
Petrik M, Haas H, Laverman P et al (2014) 68Ga-Triacetylfusarinine C and 68Ga-Ferrioxamine E for Aspergillus infection imaging: uptake specificity in various microorganisms. Mol Imaging Biol 16:102–108
Siaens R, Eijsink VG, Dierckx R et al (2004) 123I-labeled chitinase as specific radioligand for in vivo detection of fungal infections in mice. J Nucl Med 45:1209–1216
Diaz LA, Foss CA, Thornton K et al (2007) Imaging of musculoskeletal bacterial infections by [124I]FIAU-PET/CT. PLoS ONE 2:e1007
Gowrishankar G, Namavari M, Jouannot EB et al (2014) Investigation of 6-[18F]-Fluoromaltose as a novel PET tracer for imaging bacterial infection. Plos One 9:e107951–e107951
Xinghai N, Wonewoo S, Seungjun L et al (2014) PET imaging of bacterial infections with fluorine-18-labeled maltohexaose. Angew Chem Int Ed 53:14096–14101
Weinstein EA, Ordonez AA, Demarco VP et al (2014) Imaging Enterobacteriaceae infection in vivo with 18F-fluorodeoxysorbitol positron emission tomography. Sci Transl Med 6:259ra146–259ra146
Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. National Cancer Institute. Published on June 14, 2010. www.ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_40
Tang GH, Tang XL, Wang MF et al (2006) High efficient automated synthesis of 2-[18F] fluoro-2-deoxy-D-glucose. Nucl Technol 29:531–536
Li ZB, Wu Z, Cao Q et al (2008) The synthesis of 18F-FDS and its potential application in molecular imaging. Mol Imaging Biol 10:92–98
Wolf I, Vetter M, Wegner I et al (2005) The medical imaging interaction toolkit. Med Image Anal 9:594–604
Stabin MG, Sparks RB, Crowe E (2005) OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med 46:1023–1027
International Commission on Radiological Protection (ICRP) (1994) Basic anatomical and physiological data for use in radiological protection: the skeleton. ICRP publication 70. Ann ICRP 25:66–67
Yao SB, Xing HQ, Zhu WJ et al (2016) Infection imaging with 18F-FDS and first-in-human evaluation, Nucl Med Biol 43:206–14
International Commission on Radiological Protection (ICRP) (2015) Radiation dose to patients from radiopharmaceuticals: a compendium of current information related to frequently used substances. ICRP Publication 128. Ann ICRP 44:107–109
Radioactive drugs for certain research uses. Code of Federal Regulations. Title 21, Volume 5. Sec. 361.1. http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr5361
Kaushik A, Jaimini A, Tripathi M et al (2015) Estimation of radiation dose to patients from (18) FDG whole body PET/CT investigations using dynamic PET scan protocol. Indian J Med Res 142:721–31
Divoli A, Chiavassa S, Ferrer L et al (2009) Effect of patient morphology on dosimetric calculations for internal irradiation as assessed by comparisons of Monte Carlo versus conventional methodologies. J Nucl Med 50:316–323
Acknowledgments
This work was supported in part by the National Natural Science Foundation of China (Grant No. 81071188 and 81571713). We would like to extend our heartiest gratitude to Prof. Yun Zhou for the support of data management and study preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures of the study were approved by the Institutional Review Board of Peking Union Medical College Hospital.
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhu, W., Yao, S., Xing, H. et al. Biodistribution and Radiation Dosimetry of the Enterobacteriaceae-Specific Imaging Probe [18F]Fluorodeoxysorbitol Determined by PET/CT in Healthy Human Volunteers. Mol Imaging Biol 18, 782–787 (2016). https://doi.org/10.1007/s11307-016-0946-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-016-0946-9