Abstract
The role of 2-deoxy-2-[F-18]fluoro-d-glucose-positron emission tomography (FDG-PET) imaging in the clinical management of paraneoplastic neurological syndrome (PNS) is in evolution. The initial results are promising, and the potential of this modality in this setting has been demonstrated in the literature. In the setting of PNS, FDG-PET imaging can be of value from the following standpoints: (1) detection of the occult malignant focus and (2) objective assessment of the presence and extent of the functional abnormality in the brain and correlation of the imaging findings with the clinical features and disease activity. For this communication, we have not considered case reports described in the literature, while tabulating the results of the published studies. However, we have referred to important observations made in such reports. In part, this effort has been made because of the relative paucity of the existing literature on this issue. The studies investigating the role of FDG-PET imaging in detecting the sites of malignancy can be divided into two broad categories: (A) studies that incorporated FDG-PET at the initial work up of PNS along with other modalities and (B) studies where FDG-PET was applied after conventional modalities had failed to detect the offending malignancy. While majority of the studies have been of the second category, both categories have demonstrated the incremental role of FDG-PET in the detection of the primary cancer in this setting. Also, it is evident that serial studies at certain intervals should be carried out if the initial FDG-PET scan is negative. The literature describing the central nervous system findings with PET in PNS are primarily restricted to paraneoplastic limbic encephalitis (PLE) and paraneoplastic cerebellar degeneration (PCD). FDG-PET usually shows hypermetabolism in one or both temporal lobes in the setting of paraneoplastic limbic encephalitis, and the magnetic resonance imaging (MRI) findings correlate with the FDG-PET scan results in only a fraction of cases. The functional–anatomic discordance between PET and MRI in PLE needs to be examined further, which might open up new insights into the disease process and might generate further subgroups within this entity. Both modalities complement each other in PLE, and frequently, abnormalities noted on FDG-PET images can provide additional clinical information which is of great value in further patient management. In the setting of paraneoplastic cerebellar degeneration, FDG-PET generally reveals cerebellar hypometabolism similar to the cerebellar atrophy demonstrated by MRI, and FDG-PET tends to show the abnormality more often than MRI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The role of 2-deoxy-2-[F-18]fluoro-d-glucose-positron emission tomography (FDG-PET) in paraneoplastic neurological syndrome (PNS) is in evolution. Nevertheless, increasingly, the potential of this modality in this setting is emphasized in various peer review reports. We have reviewed the existing literature with regard to the FDG-PET imaging results in PNS to define its precise role and to determine whether this technique should be incorporated into the management of these patients on a routine basis. The role of FDG-PET in PNS can be viewed from two major standpoints: (1) Detection of the occult malignant focus and (2) Assessment of the functional consequences of the disease in the brain as well as their clinical correlates and changes that follow after therapeutic interventions.
At present, there is a dire necessity for detecting the offending malignant disease, as frequently, no tumor can be identified at the initial evaluation by the conventional anatomic imaging modalities. Hence, the majority of research studies until date [1–5] have focused their objectives in this particular domain. This has been also emphasized in several case reports that have appeared in the peer review literature. In general, FDG-PET imaging performs well in detecting the tumor in patients with PNS who have had negative test results after an initial work up with radiological methods. The brain FDG-PET findings have been explored by a handful of reports where the PET imaging results have been compared with the clinical presentation, and the pattern of the abnormalities in the PET images usually correlate well with the corresponding clinical settings. As PNS is a rare disorder, it is imperative to pool the existing data from different centers to examine and define the role of various investigational modalities in this important clinical setting.
Brief Overview of PNS
PNS are a rare group of central nervous system disorders that are triggered by an immune system response to a neoplasm, or cancerous tumor. The classical neurological syndromes in the PNS include encephalomyelitis, limbic encephalitis, subacute cerebellar degeneration, opsoclonus–myoclonus, and subacute sensory neuronopathy [1]. The well-characterized onconeuronal antibodies in PNS include Anti-Hu, Anti-Yo, Anti-CV2, Anti-Ri, Anti-Ma2, and Anti-amphiphysin [1]. In addition to these, there are several partially characterized onconeuronal antibodies as well. The diagnostic criteria [1] for a “definitive PNS” include any of the following: (a) classical syndrome and malignancy that develops within five years of the diagnosis of the neurological disorder, (b) nonclassical syndrome that resolves or significantly improves after therapy for the malignant disorder without concomitant immunotherapy, provided that the syndrome is not susceptible to spontaneous remission, (c) nonclassical syndrome with onconeuronal antibodies (well characterized or not), and malignancy that develops within five years of the diagnosis of the neurological disorder, (d) a neurological syndrome (classical or not) with well-characterized onconeural antibodies (anti-Hu, Yo, CV2, Ri, Ma2, or amphiphysin), and no cancer. The criteria for “possible PNS” include (a) a classical syndrome, no onconeural antibodies, no cancer but at high risk to have an underlying tumor, (b) a neurological syndrome (classical or not) with partially characterized onconeural antibodies and no cancer, (c) a nonclassical neurological syndrome, no onconeural antibodies, and the diagnosis of cancer within two years of clinical manifestation. In about two thirds of cases with an antineuronal antibody, the neurological symptoms precede the tumor diagnosis up to four years [2]. The treatment of the underlying malignancy, when it can be detected, is considered as the optimal treatment for paraneoplastic neurological syndromes. Hence, modern imaging modalities including FDG-PET whole body survey has been investigated to speed up the tumor diagnosis.
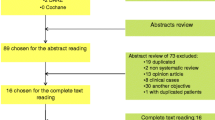
For this review, the published data were identified by searching the Pubmed on the role of FDG-PET in paraneoplastic neurological syndrome. Reports published in English were considered with no restriction on publication date. We have considered studies incorporating more than five cases, taking into account the relative paucity of FDG-PET data in PNS. Case reports were reviewed with regard to the importance of findings, but were not included in statistical tabulation. Two classical examples are selected from the published literature from our Institute and are illustrated in the present review (Figs. 1 and 2).
Demonstration of the tumor with FDG-PET and analysis of expression of Yo (cdr2) antigen. a, b The body FDG-PET obtained in 2005 (b) demonstrates FDG hyperactive abnormalities in the right axillary region that were not present in 2003 a. c, d Sections of tumor incubated with patient’s biotinylated IgG, containing anti-Yo antibodies. The reactivity observed in C (brown staining) was abrogated if the patient’s IgG was pre-absorbed with Yo antigen (d), confirming that the tumor reactivity was Yo-specific. ×400, counterstained with hematoxylin (reproduced with permission from the Elsevier Inc for Mathew et al. [8]).
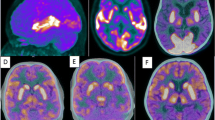
Follow-up MRI and FDG-PET in patient 7. MRI FLAIR sequences and T1 with gadolinium (T1 with GAD) obtained at three time points during the clinical course of patient 7. Note the presence of bilateral medial temporal lobe FLAIR hyperintensities with progressive evolving atrophy (arrows point to the progressive volume loss in the left hippocampus), and transient FLAIR abnormality in the right insula (October 2003). After gadolinium administration (T1 with GAD), there was mild enhancement in the left medial temporal lobe (February 2003) that resolved in the follow-up studies. The FDG-PET obtained in February 2003 showed hyperactivity in the vermis of the cerebellum (arrow) that preceded by 4 months the development of gait ataxia, and hyperactivity in the medial temporal lobes (bilateral arrows in coronal sections) that correlated with the limbic dysfunction and MRI FLAIR abnormalities in the temporal lobes. The FDG-PET in December 2003 shows resolution of the hyperactivity that correlated with transient stabilization of symptoms and decreased CSF pleocytosis after treatment with cyclophosphamide and corticosteroids (Reproduced with permission from the Oxford University Press for Ances et al. [7]).
FDG-PET in Diagnosis of Occult Malignancy in PNS
The studies investigating the role of FDG-PET imaging in detection of malignancy can be separated into two broad categories (Table 1): (A) Studies where FDG-PET was incorporated into the work up at the initial presentation of PNS along with other modalities and (B) Studies where FDG-PET was employed when conventional modality had failed.
A relative lack of uniformity of patient inclusion criteria was observed among the published studies similar to what is observed in literature in carcinoma of unknown primary with cervical lymphadenopathy. Nonetheless, the usefulness was proven irrespective of inclusion criteria of enrolment of patients who were included for the analysis.
Studies Incorporating FDG-PET at the Initial Work Up of PNS
To date, there has been one study [3] examining the efficacy of FDG-PET vis-à-vis the other modalities at the initial work up of PNS (Table 1). Linke et al. directly compared computed tomography (CT) and FDG-PET imaging in a series of 13 consecutive patients with various antineuronal antibodies. They performed CT scan and FDG-PET in parallel for detection of a tumor or tumor recurrence. A new tumor or tumor recurrence was detected in 10 out of 13 patients (five small-cell lung cancer, two ovarian cancer, and one each neuroblastoma, Hodgkin’s lymphoma, and lymph node metastasis of adenocarcinoma) in this series. Histopathological correlation was available in all tumors except in one with clinical evidence for small-cell lung cancer who did not have confirmation of diagnosis. CT was positive for malignancy in 3 of 10 patients (sensitivity of 30%), which FDG-PET detected in 9 of 10 (sensitivity of 90%), and the difference between the two methods was significant (p < 0.01), However, the combination of both methods showed a sensitivity of 100%. In this study, the probability of tumor given a positive result (PD+) was threefold higher with FDG-PET compared to that noted with CT (77% vs 23%; odds ratio = 7.5). But the most reliable results were obtained when both tests were combined together (sensitivity = 100%).
Studies Investigating the Role of FDG-PET when Conventional Modality had Failed
Four studies have investigated the efficacy of FDG-PET in PNS (Table 1) when the conventional work up had failed to discover the tumor. Antoine et al. [4] investigated 15 patients with PNS and anti-Hu antibodies. Radiological methods led to the diagnosis of malignancy in 12 patients, and test results were negative in three. FDG-PET showed abnormal foci in the mediastinum in these three patients. Of these, two had undergone mediastinoscopy and biopsy, which detected small-cell lung carcinoma. In the third case, repeat CT failed to show any mediastinal adenopathy that could undergo a biopsy. Rees et al. [5] retrospectively studied records of 43 unselected patients with suspected PND referred for FDG-PET scanning to determine the utility of this technique when conventional imaging was negative. There were discrete areas of hypermetabolism suggestive of malignancy (positive) in 16 patients (37%). Only one patient with a negative scan was diagnosed subsequently as having malignancy on prolonged follow-up. Younes-Mhenni et al. [6] prospectively studied 20 patients with paraneoplastic antibodies in whom conventional imaging gave negative or inconclusive results. In these 20 patients, abnormal uptake in FDG-PET was demonstrated in 18 patients. After FDG-PET, the histological diagnosis of the tumor was made in 14 cases (small-cell lung carcinoma in eight cases, breast adenocarcinoma in two, lung adenocarcinoma in two, axillary metastasis of ovary carcinoma in one, and malignant thymoma in one). Two other patients with abnormal FDG uptake showed radiological evidence of lung cancer, but a histological diagnosis could not be obtained. In two other patients, initial FDG-PET showed abnormal FDG uptake that was not confirmed a few months later by repeat FDG-PET. In the two patients with negative FDG-PET, peritoneal carcinomatosis was diagnosed in one, and no tumor was found in the other. In this study, the sensitivity of FDG-PET for tumor detection was 83.33%. However, in this series, the specificity of FDG uptake was only 25% due to unexplained abnormal FDG uptake in three patients and in abnormal FDG uptake due to a benign tumor in one patient. Ances et al. [7] studied seven patients with subacute limbic encephalitis initially considered of uncertain etiology. All patients underwent CT of the chest, abdomen, and pelvis, and, if negative, body FDG-PET. A tumor was found in five patients, four demonstrated by CT and one with FDG-PET (papillary carcinoma of the thyroid) where CT was negative. A careful and critical analysis of the results of these studies indicates an incremental value of FDG-PET in the detection of the malignancy even when conventional diagnostic work up had failed to diagnose the malignancy.
In an interesting report by Mary Mathew et al. [8], FDG-PET demonstrated tumor (a metastatic right axillary node from poorly differentiated breast carcinoma) in a patient (Fig. 1) with anti-Yo-associated paraneoplastic cerebellar degeneration (PCD). Tumor was demonstrated five years after the patient had developed PCD. This underscores the importance of performing serial FDG-PET studies even if the initial study is negative. Also, it is interesting to note the solitary report of discovery of a second malignancy (adenocarcinoma of the cecum) by whole-body survey with FDG-PET in an unresolving anti-Ma1/Ma2-positive PLE [20]. Two months after surgical removal of the second primary anti-Ma antibodies were negative. The authors concluded that a second malignancy should be considered, if an effective cancer treatment does not lead to improvement or stabilization of a PNS.
PET/CT in Detection of Tumor in PNS
The utility of PET/CT in detection of malignancy in PNS is in evolution. There have not been any carefully conducted clinical trials in this regard. Fused PET and CT images have the potential to provide critical information within a single study: the presence of a viable tumor and its accurate location. Frings et al. [9], in a preliminary report, described the utility of dual modality PET/CT in one patient of anti-Yo-associated PCD. PET/CT accurately detected axillary metastases of hormone receptor-negative lobular breast cancer in this particular case.
PNS and Brain FDG-PET
Paraneoplastic Limbic Encephalitis
The majority of the publications with regard to brain FDG-PET studies have been confined to case reports except for Ances et al. [7], who studied the value of brain magnetic resonance imaging (MRI) and FDG-PET in seven patients with subacute limbic encephalitis. All patients in this series had abnormal cerebral spinal fluid (CSF) examination: six pleocytosis and six had increased protein concentration, and three of five examined had oligoclonal bands. In four patients with predominant hippocampal dysfunction, MRI abnormalities were restricted to one or both medial temporal lobes. In this series except for one patient, all showed hypermetabolism in one or both temporal lobes. One patient had additional hyperactivity in the brainstem and hypoactivity in the occipital lobes, and two patients had additional sites of abnormal activity in the cerebellum. PET and MRI complemented each other but did not overlap in 50% of the patients. All patients had temporal lobe abnormalities, and in five patients, additional sites of abnormality were seen on PET. In one patient, FDG hyperactivity in the brainstem that was normal on MRI correlated with central hypoventilation; in another case, hyperactivity in the cerebellum anticipated ataxia. This is important as both these cases represented examples of incremental value of brain FDG-PET in paraneoplastic limbic encephalitis (PLE) and provided valuable information about the further clinical manifestation of the disease. There was a good correlation between the FDG activity and clinical symptoms and CSF abnormalities in this population. Fig. 2 depicts a case example from this study where the follow-up FDG-PET showed resolution of the hyperactivity after treatment with cyclophosphamide and corticosteroids which correlated with transient stabilization of clinical symptoms and reduction of CSF pleocytosis. Scheid et al. [10] performed serial MRI and FDG–PET in a patient with anti-Ma2-positive PLE. They observed increasing focal hypermetabolism on FDG-PET in the left medial temporal lobe (from the first to the fourth examination) in the context of stable MRI findings. This increase was associated with an increase in the Western blot serum anti-Ma2 antibody titers [10]. A critical review of the literature by these authors [10] revealed pronounced discrepancies between MRI and PET findings, and around half of the investigators concluded that the focal hypermetabolism on PET may represent seizure activity [11, 12], which the other half considered as the PET abnormalities representing an underlying inflammatory process [13–15]. Overall, it can be concluded that FDG-PET usually shows hypermetabolism in one or both temporal lobes in the setting of paraneoplastic limbic encephalitis, and brain MRI correlates with FDG-PET in only a fraction of cases. We believe, this functional–anatomic discordance requires to be probed further in future studies which might open up new insights into the disease process and might generate further subgroups within this entity.
Pareneoplastic Cerebellar Degeneration
Paraneoplastic cerebellar degeneration (PCD) is characterized clinically by the subacute development of cerebellar symptoms including severe ataxia, dysarthria, and nystagmus. Neuropathologically, this entity is characterized by severe loss of Purkinje cells, while the granular and molecular layers and the cerebellar nuclei are usually spared [16]. A brain PET generally reveals decreased FDG activity in the cerebellum and brain MRI depicts cerebellar atrophy, usually in the late stages of the disease. At times, both studies may appear normal in the early stages of the disease, although usually, FDG-PET tends to show abnormality more often than MRI [17]. There have been two reported exceptions [18, 19] in the literature with regard to the abovementioned facts. Choi et al. [18] reported a solitary case where cerebellar hypermetabolism was observed rather than hypometabolism which has been consistently detected with FDG-PET in the literature. This, they concluded, is because of an acute inflammatory process associated with an immunological reaction [18]. Scheid et al. [19] reported a patient in whom cerebellar atrophy was documented by MRI very early in the disease course, a finding which is usually observed in the late stages of the disease process.
So far, no typical brain features have been described in literature in other types of PNS like opsoclonus–myoclonus, subacute sensory neuronopathy. More data requires to be accrued through carefully conducted prospective studies on these issues, and functional imaging with FDG-PET has the potential to subserve multidimensional role in the clinical management of the patients suffering from this important disorder.
Conclusion
To conclude, FDG-PET appears to play a pivotal role in detecting the offending malignancy responsible for PNS. The role of PET/CT, although not examined in detail, has the potential to become the investigational modality of choice in the future. Serial FDG-PET studies should be performed even if the initial FDG-PET is negative for malignancy. Brain FDG-PET and brain MRI are both complementary to each other, and frequently, abnormalities noted on FDG-PET images can provide additional information which is clinically significant. Another point of interest is the impact of the PET diagnosis on the well-being of the patients. Does PET-CT in PNS have any effect on the outcome or well-being of the patient, or can the quality of life be improved? Theoretically, early identification of the underlying malignancy at a stage when it is localized and more amenable to treatment is likely to be beneficial in halting the ongoing immune assault to the nervous system, but this requires to be examined further.
References
Graus F, Delattre JY, Antoine JC et al (2004) Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry 75:1135–1140
Voltz R (2002) Paraneoplastic neurological syndromes: an update on diagnosis, pathogenesis and therapy. Lancet Neurol 1:294–305
Linke R, Schroeder M, Helmberger T, Voltz R (2004) Antibody-positive paraneoplastic neurologic syndromes: value of CT and PET for tumor diagnosis. Neurology 63(2):282–286, Jul 27
Antoine JC, Cinotti L, Tilikete C, Bouhour F, Camdessanche JP, Confavreux C, Vighetto A, Renault-Mannel V, Michel D, Honnorat J (2000) [18F]fluorodeoxyglucose positron emission tomography in the diagnosis of cancer in patients with paraneoplastic neurological syndrome and anti-Hu antibodies. Ann Neurol 48(1):105–108, Jul
Rees JH, Hain SF, Johnson MR, Hughes RA, Costa DC, Ell PJ, Keir G, Rudge P (2001) The role of [18F]fluoro-2-deoxyglucose-PET scanning in the diagnosis of paraneoplastic neurological disorders. Brain 124(Pt 11):2223–2231, Nov
Younes-Mhenni S, Janier MF, Cinotti L, Antoine JC, Tronc F, Cottin V, Ternamian PJ, Trouillas P, Honnorat J (2004) FDG-PET improves tumour detection in patients with paraneoplastic neurological syndromes. Brain 127:2331–2338, Oct
Ances BM, Vitaliani R, Taylor RA, Liebeskind DS, Voloschin A, Houghton DJ, Galetta SL, Dichter M, Alavi A, Rosenfeld MR, Dalmau J (2005) Treatment-responsive limbic encephalitis identified by neuropil antibodies: MRI and PET correlates. Brain 128(Pt 8):1764–1777, Aug
Mathew RM, Cohen AB, Galetta SL, Alavi A, Dalmau J (2006) Paraneoplastic cerebellar degeneration: Yo-expressing tumor revealed after a 5-year follow-up with FDG-PET. J Neurol Sci 250(1–2):153–155, Dec 1
Frings M, Antoch G, Knorn P, Freudenberg L, Bier U, Timmann D, Maschke M (2005) Strategies in detection of the primary tumour in anti-Yo associated paraneoplastic cerebellar degeneration. J Neurol 252(2):197–201, Feb
Scheid R, Lincke T, Voltz R, von Cramon DY, Sabri O (2004) Serial 18F-fluoro-2-deoxy-d-glucose positron emission tomography and magnetic resonance imaging of paraneoplastic limbic encephalitis. Arch Neurol 61(11):1785–1789 Review, Nov
Franck G, Sadzot B, Salmon E et al (1987) Paraneoplastic limbic encephalopathy, inappropriate secretion of ADH, and recurrent infraclinical epileptic seizures: clinical anatomo-pathological and metabolic correlations by positron emission tomography. Rev Neurol (Paris) 143:657–669
Fakhoury T, Abou-Khalil B, Kessler RM (1999) Limbic encephalitis and hyperactive foci on PET scan. Seizure 8:427–430
Provenzale JM, Barboriak DP, Coleman RE (1998) Limbic encephalitis: comparison of FDG PET and MR imaging findings. AJR Am J Roentgenol 170:1659–1660
Na DL, Hahm DS, Park JM, Kim SE (2001) Hypermetabolism of the medial temporal lobe in limbic encephalitis on 18FDG-PET scan: a case report. Eur Neurol. 45:187–189
Kassubek J, Juengling FD, Nitzsche EU, Lücking CH (2001) Limbic encephalitis investigated by 18FDG-PET and 3D MRI. J Neuroimaging 11:55–59
Lantos PL, Louis DN, Rosenblum MK et al (2002) Paraneoplastic syndromes. In: Graham DI, Lantos PL (eds) Greenfield’s neuropathology. 7th edn. Arnold, London, pp 975–980
Rubello D, Vitaliani R, Rigoni MT, Rampin L, Giometto B, Casara D, Zonzin GC, Zavagno G, Capirci C, Shapiro B, Muzzio PC (2005) A rare case of paraneoplastic cerebellar degeneration discovered by whole-body F-18 FDG PET. Clin Nucl Med 30(10):704–706, Oct
Choi KD, Kim JS, Park SH, Kim YK, Kim SE, Smitt PS (2006) Cerebellar hypermetabolism in paraneoplastic cerebellar degeneration. J Neurol Neurosurg Psychiatry 77(4):525–528, Apr
Scheid R, Voltz R, Briest S, Kluge R, von Cramon DY (2006) Clinical insights into paraneoplastic cerebellar degeneration. J Neurol Neurosurg Psychiatry 77(4):529–530, Apr
Leyhe T, Schule R, Schwarzler F, Gasser T, Haarmeier T (2006) Second primary tumor in anti-Ma1/2-positive paraneoplastic limbic encephalitis. J Neurooncol 78(1):49–51, May
Acknowledgment
This work was supported in part by the International Union against Cancer (UICC), Geneva, Switzerland, under the ACSBI fellowship.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Basu, S., Alavi, A. Role of FDG-PET in the Clinical Management of Paraneoplastic Neurological Syndrome: Detection of the Underlying Malignancy and the Brain PET-MRI Correlates. Mol Imaging Biol 10, 131–137 (2008). https://doi.org/10.1007/s11307-008-0134-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-008-0134-7