Abstract
Purpose
This work investigated whether fLuc-catalyzed oxidation of d-luciferin generates sufficient light to induce photodynamic toxicity in cancer cells.
Procedures
Light emission was assessed via cooled CCD (charge-coupled device) camera. Parental and fLuc expressing cancer cells were exposed to subtoxic concentrations of photosensitizers (Rose Bengal or hypericin) and d-luciferin, sunlight, or lamplight. Toxicity was assessed by MTT assay.
Results
fLuc expressing cells emitted up to 500-fold higher levels of photons than parental cell lines. Although exposure to photosensitizer and sunlight reduced survival of various cell lines, survival of fLuc expressing cells incubated with photosensitizer and d-luciferin, or photosensitizer and lamplight, did not differ significantly from parental or untreated cells.
Conclusions
Contesting recent reports, fLuc bioluminescence does not generate sufficient photons to induce Rose Bengal or hypericin photodynamic toxicity in a range of malignant and nonmalignant cell lines, and is not suitable as a generalizable approach to antineoplastic therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Light has been recognized as a therapeutic agent for more than 3,000 years [1]. In a serendipitous discovery in 1900, the chemical acridine was observed to have a lethal effect on infusoria in the presence of light, but to be harmless in the dark [2]. The discovery of this “photodynamic action” [3] marked the beginning of modern-day photodynamic therapy (PDT). Photodynamic therapy uses the combined toxic effect of two individually nontoxic events (a photosensitizing chemical and an appropriate wavelength excitation light) to induce cellular and tissue toxicity in the presence of oxygen. A photosensitizer molecule is transformed from ground energy state (singlet state) transiently to excited singlet state upon absorption of a photon. It then enters the comparatively long-lived triplet state. Triplet state photosensitizer confers damage to cells via two pathways. In type I reactions, it interacts with cellular structures, transfers a hydrogen atom, and induces the formation of radicals, which proceed to interact with oxygen to produce oxygenated end products. In type II reactions, triplet-state photosensitizer interacts directly with oxygen and induces the formation of singlet oxygen, a reactive oxygen species, which in turn causes cellular toxicity [4]. Over the last three decades, PDT has been successfully employed for tumor treatment, and a large number of new photosensitizing agents have been discovered. Photosensitizers are now approved for human therapeutic use against various tumors [5–10]. Photodynamic therapy is limited by light accessibility of the tumors (either directly or through invasive techniques, such as needle or endoscopy-guided fiber optics). Once tumors metastasize, it becomes difficult or impossible to reach and treat all sites of the disease. It would thus be of interest to develop a technique with which light could be delivered to tumors anywhere in the body.
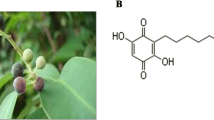
Genes coding for light-generating proteins, such as the firefly luciferase (fLuc) gene from American firefly (Photinus pyralis), are widely used in molecular and cell biology research applications. They monitor the expression of genes (“reporter genes”), or track the distribution of fusion proteins. In a process called “bioluminescence,” the fLuc protein oxidizes its substrate d-luciferin to oxyluciferin in the presence of oxygen, ATP, cofactors, and Mg+, leading to light production with a peak measurable at 562 nm. The fLuc system is inexpensive and has developed into one of the most widely used modalities in imaging molecular events in vitro and in vivo [11, 12].
Targeted gene delivery allows for the selective delivery of genes to certain tissues or tumors, whereas tumor- or tissue-specific promoters can be used to restrict the expression of genes to tissues or tumors of interest. Genes can be selectively delivered to tumors and their metastases with a range of vehicles (e.g., transferrin-coated polyethyleneimine complexes [13], genetically altered, “retargeted” adenoviruses that express tumor-targeting protein sequences within their knobs, or bispecific antibodies that target antigens both on the tumor and on the delivery virus). Tumor-specific gene expression can be driven by tissue- or tumor-specific promoters, such as the PSA promoter in prostate carcinoma [14], the Chromogranin A promoter in neuroendocrine tumors [15], or the glut1 promoter, which is specific for many neoplastic tissues [16]. Weak tissue specific promoters can be amplified by using strategies such as the two-step transcriptional activation, or the Cre–LoxP system [17, 18]. Recently, expression of the fLuc gene was detected in lung and bone metastases of prostate tumor cells after a systemic injection of an adenovirus carrying the gene. The prostate-specific enhancer permitted the expression of fLuc in metastases, but restricted its expression in the liver, which would normally be the site of the strongest expression [19].
Because light-producing genes such as fLuc can be selectively delivered to neoplastic tissues via gene therapy strategies, the method has been implied as a possible solution of the light delivery dilemma that PDT is faced with. If sufficient light were generated by fLuc bioluminescence, then enough light could in theory be delivered to tumors and metastases anywhere in the body [20]. Carpenter et al. [21] reported that fLuc induced activation of hypericin and had an antiviral effect on equine infectious anemia virus. However, doubts remain whether fLuc can generate enough photons to induce a phototoxic effect on tumors. Irradiances commonly used in PDT clinical trials using lasers for photon generation amount reach about 50 mW/cm2 [22]. In spite of these considerations, a 90% reduction in the survival rate of fLuc-transfected NIH3t3 mouse fibroblast cells was recently reported following incubation with the photosensitizer Rose Bengal [23]. Although fibroblasts tend to be less resistant to various forms of cellular stress (e.g., chemotherapy, PDT, radiation, etc.) than cancer cell lines, we took this report as an indicator that bioluminescence-activated PDT might indeed be successful in spite of considerations that light output might not be sufficient. It was the aim of this study to clarify whether the principle of bioluminescence-activated PDT can be applied to tumor cells with the long-term goal of using fLuc as a photon donor for in vivo PDT.
Materials and Methods
Cell Culture
Cells were maintained at 37°C in an atmosphere of room air and 5% CO2. C6 rat glioma cells (kindly provided by Dr. M.E. Black, Washington State University, Pullman, WA, USA), Neuro 2a (N2a) neuroblastoma cells (a gift from Dr. V. Mauro, Scripps Research Institute, La Jolla, CA, USA), NIH3t3 mouse fibroblasts [American Type Culture Collection (ATCC), Manassas, VA, USA], MCF7 human breast cancer cells (donated by Dr. I. Wapnir, Stanford University, Palo Alto, CA, USA), 3T3-L1 mouse adipocytes (ATCC), and A375M human melanoma cells (a gift from Dr. M. Kolodny; University of California, Los Angeles, CA, USA) were kept in Dulbecco's modified Eagle medium (high glucose) (Gibco, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS; Gibco), 100 μg/mL penicillin/100 μg/mL streptomycin (Gibco), 100 μM nonessential amino acids (Gibco), 1 mM Na pyruvate (Gibco), and 10 mM HEPES buffer (Gibco). CHO hamster ovarian carcinoma cells (ATCC) were cultured in DMEM/Hams F12 50/50 medium (Gibco) supplemented with 10% FBS and penicillin/streptomycin. 293T human embryonic kidney cells (ATCC) were maintained in minimum essential medium (Gibco) supplemented with 10% FBS and penicillin/streptomycin. C6fLuc and N2afLuc were cultivated in growth medium of the respective parental cell line supplemented with 500 ng/mL Geneticin (Gibco).
Generation of Stably Transfected Cell Lines
Stably transfected cell lines C6fLuc and N2afLuc were generated by transfecting C6 or N2a cells, respectively, with the eukaryotic expression plasmid pcDNAfLuc, which contains the fLuc gene under the control of the cytomegalovirus promoter in a pcDNA3.1 vector backbone (Promega). For transient transfections, Superfect transfection reagent (Qiagen, Valencia, CA, USA) was used following the protocol recommended by the manufacturer. Forty-eight hours after transfection, 500 ng/mL Geneticin was added to the growth medium. Clones of surviving cells were isolated 2 weeks later and analyzed for fLuc expression using the Luciferase Reporter Assay System (Promega). Reactions were measured in a TD 20/20 luminometer (Turner Designs, Sunnyvale, CA, USA) for a period of 10 s. The clones with the highest fLuc expression (RLU/μg protein as determined by Bradford assay) were chosen for further experiments.
Assessment of Light Emission From fLuc Expressing N2afLuc and C6fLuc and Control Cells
Light emission from fLuc expressing cell lines (C6fLuc, N2afLuc) and control cells without fLuc expression (C6, N2a) was assessed by serial imaging with a CCD (charge-couple device) camera (IVIS 100; Xenogen, Inc.). Cells (104) were seeded into black 96-well tissue culture wells and left to attach overnight. In the morning, growth medium was replaced by phosphate-buffered saline containing 600 μg/mL d-luciferin, and serial CCD camera imaging was started immediately (acquisition time, 60 s). Regions of interest were drawn over wells and quantified by using the Living Image Software version 2.20. Bioluminescence signals were recorded as maximum [photons/second/cm2/steradian (photons/s/cm2/sr)].
PDT Using fLuc Bioluminescence as Photon Donor
To exclude any influence of ambient light, all therapy experiments were performed in complete darkness. Handling in the dark was done with the help of an infrared videocamera (Sony digital video camera recorder DCR-TRV-30, Sony, Japan). When not handled or exposed to sunlight or lamplight, cells were wrapped in light tight aluminum foil at all times. Stably fLuc expressing cell lines (C6fLuc, N2afLuc) and control cells without fLuc expression (C6, N2a) were seeded into black 96 well plates with clear bottoms at densities of 104 cells per well. Cells were incubated for 3 h in serum-free medium without phenol red containing the following concentrations of photosensitizers: Rose Bengal (RB, Sigma) (0, 1, 10, or 50 μM) or hypericin (Hy, Sigma) (0, 0.1, 1, 10, or 100 μM). Medium was then changed to normal growth medium containing the following concentrations of d-luciferin (Xenogen, Inc.): 0, 50, 100, or 500 nM, or 0.4, 2, 4, or 20 μM. After incubation for 24 h, cell death was assessed by MTT assay (Sigma) according to the instructions of the manufacturer.
PDT Using Sunlight as Photon Donor
Various cell lines (C6fLuc, C6, N2afLuc, N2a, NIH3t3, MCF7, 3T3, CHO, 293T, A375) were plated as described above and incubated for 3 h without photosensitizer, with 10 μM RB, or with 1 μM Hy as described above. Cells were then either incubated in the dark for 24 h or exposed to midday sunlight for 1 h and incubated in the dark for 23 h before MTT assays as described above.
PDT Using Lamplight as Photon Donor
A375 and 293T cells were plated as described above and incubated either without photosensitizer, with 10 μM RB, or with 1 μM Hy as described above. Cells were then exposed to lamplight from a Philips E32T8/TL741 lamp for 0, 5, 15, 30, 60, or 120 min, incubated in complete darkness for 22–24 h and analyzed for cell survival by MTT assay.
Statistical Testing
Statistical significance between groups was assessed via Student's t-test. P < 0.05 was considered statistically significant.
Results
High Levels of Light Generation in Stably Transfected Cell Lines
C6 cells stably expressing fLuc (C6fLuc) and N2a cells stably expressing fLuc (N2afLuc) were generated by transient transfection of C6 or N2a cells with pcDNAfLuc, subsequent selection with Geneticin, and clonal expansion. Light emission as measured by luminometer was detected in both cell lines, and was 3 log orders higher in N2afLuc cells (479.893 RLU/μg protein) than in C6fLuc cells (0.449 RLU/μg protein). Relative to parental cell lines, light emission was increased by 500-fold in N2afLuc and by 7-fold in C6fLuc.
Long Duration of Light Emission from fLuc Expressing Cells
Maximal levels of light emission as measured by a CCD camera were reached within 25 min of exposure to d-luciferin in both C6fLuc and N2afLuc (Fig. 1). Maximal light emission was higher from N2afLuc (2.3 × 103 photons/s/cell) than from C6fLuc (2.0 × 101 photons/s/cell), N2a (4.6 × 100 photons/s/cell), or C6 (2.8 × 100 photons/s/cell) cells. Levels of light generation fell subsequently, reaching two thirds of maximum after 2.5 h, and background levels after 19 h. After reaching background levels, light emission from N2afLuc cells declined further to 60% of nontransfected N2a cells at 24 h (2.8 × 10−1 vs. 4.8 × 10−1 photons/s/cell). In contrast, light emission of C6fLuc cells did not decrease beneath that of C6 cells in the observed interval (4.3 × 100 vs. 3.4 × 10−1 photons/s/cell).
fLuc-Bioluminescence-Induced Photodynamic Toxicity is Absent In Cancer Cells
Survival of C6fLuc cells as measured by MTT assay following incubation with 0.1, 1, or 10 μM hypericin did not differ significantly from that of cells incubated without photosensitizer. Also, no significant difference in survival was observed between C6fLuc cells and C6 parental cells, which did not express fLuc (Fig. 2A). The same result was found at varying concentrations of d-luciferin ranging from 0 to 500 nM. Survival of C6fLuc cells compared to either C6 parental cells or C6fLuc cells without photosensitizer was not significantly decreased after incubation with 1, 10, or 50 μM Rose Bengal (Fig. 2B). Similarly, there was no significant change in survival between N2afLuc cells following incubation with either of the photosensitizers under the conditions mentioned above and either N2a parental cells or N2afLuc cells not incubated with photosensitizers (Fig. 2C and D). To assess what levels of d-luciferin or hypericin would be toxic, N2afLuc and N2a cells were exposed to increasing concentrations of the chemicals (0.4, 2, 4, and 20 μM of d-luciferin, and 10 and 100 μM of hypericin, respectively) (Fig. 3). d-Luciferin levels of 4 μM and higher led to a significant decrease in cell survival regardless of photosensitizer concentration. Hypericin concentrations of 10 μM led to a small, but insignificant, decrease in cell survival, whereas hypericin concentrations of 100 μM led to a marked and significant reduction in cell survival (Fig. 3) regardless of d-luciferin concentration.
(A) PDT of fLuc transfected and parental cancer cell lines using fLuc as a photon donor. Triplicate MTT assays of C6/C6fLuc (upper panel) and N2a/N2afLuc (lower panel) following a 3-h incubation period with 0 μM (white column), 1 μM (light gray column), 10 μM (dark gray column), or 50 μM (black column) Rose Bengal and a 24-h incubation with 0, 50, 100, or 500 nM d-luciferin. (B) PDT of fLuc transfected and parental cancer cell lines using fLuc as a photon donor. Triplicate MTT assays of C6/C6fLuc (upper panel) and N2a/N2afLuc (lower panel) following a 3-h incubation period with 0 μM (white column), 0.1 μM (light gray column), 1 μM (dark gray column), or 100 μM (black column) hypericin, and a 24-h incubation with 0, 50, 100, or 500 nM d-luciferin.
Sunlight Induces Photodynamic Toxicity in the Presence of Rose Bengal or Hypericin
To ascertain whether any cytotoxic effect could be achieved at all with the photosensitizers used in this study, C6, C6fLuc, N2a, and N2afLuc cells were exposed to the California midday sun in April (ca. 100 mW/cm2) for 1 h (ca. 360 J/cm2) after incubation with Rose Bengal (0, 1, 10, or 50 μM) or hypericin (0, 0.1, 1, or 10 μM) (Fig. 4). Rose Bengal did not induce photodynamic toxicity in any of the cells lines at the concentrations tested. Hypericin, however, caused a significant reduction in the survival of N2afLuc and N2a cells at 1 μM (64.5 ± 5.4% to 69.3 ± 2.6% of controls treated with 0 M hypericin), and almost complete cell death in all cell lines at 10 μM (4.4 ± 0.8% to 12.1 ± 4.7% of controls). To determine whether other cell lines might be more vulnerable to PDT than the ones we initially chose, we exposed the following cell lines to sunlight following a 3-h incubation period with the highest nontoxic concentrations of Rose Bengal (10 μM) and hypericin (1 μM): MCF7, NIH3T3, 3T3L1, CHO, 293T, A375M. We observed significant (P < 0.05) reductions in survival as compared to cells not exposed to either photosensitizer or sunlight in the following cell lines: MCF7 (Hy, 71.7 ± 3.6% of untreated), NIH3t3 (RB, 53.9 ± 7.1%; Hy, 61.6 ± 11.3%), CHO (RB, 65.9 ± 13.1%), 293T (RB, 69.0 ± 18.1%), A375 (RB, 40.6 ± 0.7%, Hy, 55.6 ± 1.9%). All other reductions in cell survival were not significant (Fig. 5).
PDT using sunlight as a photon donor. Upper panel: triplicate MTT assays of N2a/N2afLuc and C6/C6fLuc cancer cells following a 3-h incubation period with 0 μM (white column), 1 μM (light gray column), 10 μM (dark gray column), or 50 μM (black column) Rose Bengal, 1 h of sunlight, and a 24-h incubation in the dark. Lower panel: triplicate MTT assays of N2a/N2afLuc and C6/C6fLuc cancer cells after a 3-h incubation period with 0 μM (white column), 0.1 μM (light gray column), 1 μM (dark gray column), or 100 μM (black column) hypericin, 1 h of sunlight, and a 24-h incubation in the dark.
PDT in various cell lines using sunlight as a photon donor. Upper panel: triplicate MTT assays of MCF7, NIH3T3, 3T3L1, CHO, 293T, and A375M cells following a 3-h incubation period without Rose Bengal and 1 h of darkness (white column), 3 h incubation period without Rose Bengal and 1 h of sunlight (light gray column), 3 h incubation period with 10 μM Rose Bengal and 1 h of darkness (dark gray column), 3 h incubation period with 10 μM Rose Bengal and 1 h of sunlight (black column), and a 24-h incubation in the dark. Lower panel: triplicate MTT assays of MCF7, NIH3T3, 3T3L1, CHO, 293T, and A375M cells following a 3-h incubation period without hypericin and 1 h of darkness (white column), 3 h incubation period without hypericin and 1 h of sunlight (light gray column), 3 h incubation period with 1 μM hypericin and 1 h of darkness (dark gray column), 3 h incubation period with 1 μM hypericin and 1 h of sunlight (black column), and a 24-h incubation in the dark.
Lamplight-Induced Photodynamic Toxicity is Absent In 293T and A375M Cells
We chose two cell lines that had been susceptible to photosensitizer toxicity in combination with sunlight (293T and A375M), and incubated them for 3 h without photosensitizer, with Rose Bengal (10 μM), or with hypericin (1 μM), and exposed them to lamplight from a Philips E32T8/TL741 lamp (ca. 0.1 mW/cm2 in our experimental setup) for up to 2 h (ca. 720 mJ/cm2). However, we did not observe any significant change in survival of 293T and A375 cells after up to 2 h exposure to lamplight with either photosensitizer (Fig. 6).
PDT in A375M (upper panel) and 293T (lower panel) cells using lamplight as a photon donor. Triplicate MTT assays of cells following a 3-h incubation period without photosensitizer (white column) with 10 μM Rose Bengal (gray column), or with 1 μM hypericin (black column), 0, 5, 15, 30, 60, or 120 min of Philips E32T8/TL741 lamplight, and a 22- to 24-h incubation in the dark.
Discussion
PDT of malignant disease is presently faced with the dilemma of deeper-lying tumor sites or metastases being inaccessible to therapeutic light. The bioluminescent protein encoded by the reporter gene fLuc can potentially deliver photons to any site in the body by using targeted gene delivery and targeted gene expression technology. Using fLuc as the source of therapeutic photons has been proposed as a possible solution to the problem of accessibility in PDT of malignant disease [20]. However, doubts remain whether photon output of fLuc transfected cells is sufficient to induce a photodynamic effect when compared to light doses usually administered in clinical PDT (around 50 mW/cm2, and above 1 J/cm2 [22]).
Photon output from fLuc transfected cells in our laboratory reaches 2.3 × 103 photons/s/cell, which approximately corresponds to only 4.6 × 10−13 mW/cell, or 1.2 × 10−9 mW/cm2 (for calculations, see below). Challenging these findings, a 90% reduction in survival of fLuc expressing NIH3T3 fibroblasts was recently reported after incubation with the photosensitizer Rose Bengal and d-luciferin, the substrate of fLuc [23], supporting the idea that fLuc can generate enough photons for a marked photodynamic effect on cells in the presence of a suitable photosensitizer.
Malignant cells tend to be more resistant to various forms of therapy than fibroblasts, and it was not clear whether this finding could be extrapolated to cancer cells in general. Also, in vitro conditions may favor the occurrence of a photodynamic effect, which is dependent on the presence of oxygen, and less pronounced under hypoxic conditions, such as a malignant tumor in vivo [4, 24]. It was the aim of this work to understand whether fLuc-catalyzed oxidation of d-luciferin could induce a photodynamic effect in cancer cells in the presence of suitable photosensitizers in spite of the theoretical considerations hinting at insufficient photon generation. If PDT using fLuc as the photon donor proved to be a generalizable approach to in vitro PDT of malignant tumors, it was our aim to investigate whether these findings could be reproduced in an in vivo setting.
Photon flux and total light exposure dose are among the most important variables influencing the degree of a photodynamic effect [4]. We found light emission from N2afLuc (2.3 × 103 photons/s/cell) to be higher by approximately a factor of 40 than that reported by Theodossiou et al. [23], and lower by a factor 3 in C6fLuc (2.0 × 101 photons/s/cell). Also, we observed increased light output until up to 19 h, further increasing total light exposure dose as compared to fLuc expressing NIH3t3 cells, for which kinetics are only reported for up to 83 min, when light emission reached background levels. As far as photon flux and total light exposure dose are concerned, and compared to data presented by Theodossiou et al. [23], N2afLuc cells appeared a promising candidate for in vitro PDT. N2afLuc luminescence fell below background levels (generated by spontaneous oxidation of d-luciferin), indicating that all d-luciferin in the N2afLuc assay had been depleted. C6fLuc cells appeared a less obvious choice for PDT, because photon flux was lower, but were still considered worth being evaluated, as the longer duration of light emission might compensate for lack of photon flux by increasing total light exposure dose.
The peak of fLuc light emission (550–600 nm) lies in a region of the wavelength spectrum where both photosensitizers have strong absorbance peaks (Rose Bengal at 559 nm [25], hypericin at 540–600 nm [26]). However, we observed no significant photodynamic effect, testing various concentrations of the two photosensitizers and d-luciferin. The conditions we tested included the exact replication of the conditions reported to result in a 90% reduction of fLuc expressing NIH3t3 cells (10 μM Rose Bengal and 500 nM d-luciferin, [23]). To ascertain that the experimental setup was correct and to exclude potential interfering factors connected to the photosensitizers we used, we investigated whether a photodynamic effect could be shown at maximal light levels, such as sun exposure (ca. 100 mW/cm2, and 360 J/cm2). This experiment resulted in decreased survival of both cell lines when incubated with hypericin, but not when incubated with Rose Bengal. As experimental conditions were otherwise analogous to those reported to result in a 90% reduction of NIH3T3 cell survival [23], we next investigated whether different cell types showed different response to PDT and could potentially explain the discrepancies.
We next tested a range of malignant and nonmalignant cell lines (including NIH3t3) with maximal light levels and maximal subtoxic levels of photosensitizers, and finally observed marked reductions in cell survival with maximal levels of sunlight. However, even after exposure to maximal levels of light for 1 h, none of our cell lines, including NIH3t3, showed a reduction in survival that was close to the levels reported by Theodossiou et al. [23] after incubation of fLuc transfected NIH3t3 cells with d-luciferin. To quantify light exposure better, we used a Philips E32T8/TL741 lamp for light delivery to those cell lines that were most sensitive to PDT using sunlight. Based on the manufacturer's data and our experimental setup, we estimate that roughly 0.1 mW/cm2, and up to 720 mJ/cm2, was delivered to the surface of the cells. Again, no cell death was observed over a wide range of light exposure, making it further unclear what had caused the marked drop in cell survival reported in the literature [23]. We have no immediately evident explanation for this discrepancy of results between the two reports. One might argue that the intracellular distribution of photosensitizers may play a role. Indeed, it has been shown that the subcellular compartments to which photosensitizers localize affect the localization and the type of damage conferred to a cell [27–29]. However, this does not explain why NIH3t3 cells, which should have a similar subcellular distribution of Rose Bengal whether transfected with fLuc or not, should show markedly lower sensitivity to sunlight in our work than reported for (nonvisible) fLuc-generated light. Another theory seeking to explain the differences is that the subcellular distribution of fLuc protein may affect the place where photons are generated, which may in turn affect higher damage to closer-lying, potentially more sensitive subcellular structures [21]. Whether or not this is the case, it should not affect the sensitivity of NIH3t3 cells to PDT when sunlight is used as a photon donor. Monolayer cells in cell culture are translucent enough to permit sunlight to pass through them without marked absorption, unless they produce a light-absorbing pigment, such as melanin, which is not the case for NIH3t3. Since enough photons are present in sunlight to pass through the cells and still be visible on the other side, this should allow every structure in the cell to be reached by many more photons than are produced by fLuc-catalyzed oxidation of d-luciferin, which is, after all, not visible to the naked eye unless helped by a CCD camera. The only possible explanation, to us, appears to be that the particular stable cell line used in the report by Theodossiou et al. [23] contains an unknown mutation increasing the sensitivity to PDT by a yet to be determined mechanism. This appears all the more likely when one considers the photon output of the cells used in this study and compares it to light doses usually administered in clinical PDT. Using Einstein's photoelectric effect formula E = hc/L, where h (Planck's constant) = 6.626 × 10−34 J s, c (speed of light) = 3 × 108 m/s, and assuming L (wavelength) = 0.5 μm, one can roughly assume an average energy of 2 × 10−19 J per photon. Under this assumption, N2afLuc cells produce approximately 4.6 × 10−13 mW/cell during maximal light emission. Assuming a density of confluent cells of 2.6 × 104 cells/cm2 would result in 1.2 × 10−9 mW/cm2, as compared to irradiance of around 50 mW/cm2 commonly used in clinical trials [22]. Even assuming that maximal levels of photons were emitted for 24 h (which is not the case in our experimental setting), the total energy delivered would only be 1.03 × 10−4 mJ/cm2, as opposed to above 1 J/cm2 in clinical trials involving laser light. Future studies should carefully observe the amount of photons, and energy, which is produced by cells, and correlate this to any potential photodynamic effect.
Although it appears unlikely that any of the photosensitizers used in this study should work when activated by fLuc bioluminescence, it is theoretically conceivable that under ideal conditions, cellular damage may occur. The efficiency of energy transfer in a nonradiative Foerster energy transfer mechanism is highly dependent on distance [21], and likewise, damage is most likely to occur when radicals are formed as close as possible to the sensitive structure. Assuming that both high levels of fLuc-generated light and photosensitizer are directly in the cellular compartment that is targeted, one could envision a possible effect. However, for the time being, further study is necessary to optimize photosensitizer activation, subcellular localization, and targeting and enhancement of fLuc light production.
In our study, fLuc bioluminescence does not generate enough photons to induce a photodynamic effect of the photosensitizers Rose Bengal and hypericin in a range of malignant and nonmalignant cell lines. This is even more relevant for PDT in vivo. Compared to in vitro cell culture, tumors in animal or humans have much lower oxygen concentrations, which dramatically decreases PDT efficacy. In addition, successful delivery of photosensitizer, fLuc gene, and fLuc substrate to the tumor remains a challenge. In the light of our data, it appears safe to conclude that, because of insufficient photon generation, fLuc-induced photodynamic toxicity is not likely a generalizable antineoplastic therapy.
References
Ackroyd R, Kelty C, Brown N, Reed M (2001) The history of photodetection and photodynamic therapy. Photochem Photobiol 74:656–669
Raab O (1900) Ueber die Wirkung fluoreszierender Stoffe auf Infusorien. Z Biol:524–546
Von Trappeiner H, Jodlbauer A (1907) Die Sensibilisierende Wirkung fluorieszierender Stoffe. Gesammte Untersuchungen ueber die photodynamische Erscheinung. F.C.W. Vogel, Leipzig
Dolmans DE, Fukumura D, Jain RK (2003) Photodynamic therapy for cancer. Nat Rev Cancer 3:380–387
Schweitzer VG (1990) Photodynamic therapy for treatment of head and neck cancer. Otolaryngol Head Neck Surg 102:225–232
McCaughan JS Jr, Hicks W, Laufman L, May E, Roach R (1984) Palliation of esophageal malignancy with photoradiation therapy. Cancer 54:2905–2910
Kelly JF, Snell ME (1976) Hematoporphyrin derivative: A possible aid in the diagnosis and therapy of carcinoma of the bladder. J Urol 115:150–151
Hayata Y, Kato H, Konaka C, Ono J, Takizawa N (1982) Hematoporphyrin derivative and laser photoradiation in the treatment of lung cancer. Chest 81:269–277
Hayata Y, Kato H, Okitsu H, Kawaguchi M, Konaka C (1985) Photodynamic therapy with hematoporphyrin derivative in cancer of the upper gastrointestinal tract. Semin Surg Oncol 1:1–11
Ward BG, Forbes IJ, Cowled PA, McEvoy MM, Cox LW (1982) The treatment of vaginal recurrences of gynecologic malignancy with phototherapy following hematoporphyrin derivative pretreatment. Am J Obstet Gynecol 142:356–357
Schipper ML, Gambhir SS (2006) Imaging gene expression: Concepts and future outlook. In: Schiepers C (ed) Diagnostic Nuclear Medicine, 2nd revised edition. Springer, Berlin, pp. 311−342.
Massoud TF, Gambhir SS (2003) Molecular imaging in living subjects: Seeing fundamental biological processes in a new light. Genes Dev 17:545–580
Hildebrandt IJ, Iyer M, Wagner E, Gambhir SS (2003) Optical imaging of transferrin targeted PEI/DNA complexes in living subjects. Gene Ther 10:758–764
Iyer M, Wu L, Carey M, et al. (2001) Two-step transcriptional amplification as a method for imaging reporter gene expression using weak promoters. Proc Natl Acad Sci USA 98:14595–14600
Schipper ML, Weber A, Behe M, et al. (2003) Radioiodide treatment after sodium iodide symporter gene transfer is a highly effective therapy in neuroendocrine tumor cells. Cancer Res 63:1333–1338
Sieger S, Jiang S, Kleinschmidt J, et al. (2004) Tumor-specific gene expression using regulatory elements of the glucose transporter isoform 1 gene. Cancer Gene Ther 11:41–51
Ray S, Paulmurugan R, Hildebrandt I, et al. (2004) Novel bidirectional vector strategy for amplification of therapeutic and reporter gene expression. Hum Gene Ther 15:681–690
Sundaresan G, Paulmurugan R, Berger F, et al. (2004) MicroPET imaging of Cre-loxP-mediated conditional activation of a herpes simplex virus type 1 thymidine kinase reporter gene. Gene Ther 11:609–618
Adams JY, Johnson M, Sato M, et al. (2002) Visualization of advanced human prostate cancer lesions in living mice by a targeted gene transfer vector and optical imaging. Nat Med 8:891–897, Epub 2002 Jul 22
Babincova M, Sourivong P, Babinec P (2000) Gene transfer-mediated intracellular photodynamic therapy. Med Hypotheses 54:180–181
Carpenter S, Fehr MJ, Kraus GA, Petrich JW (1994) Chemiluminescent activation of the antiviral activity of hypericin: A molecular flashlight. Proc Natl Acad Sci USA 91:12273–12277
Gerscher S, Connelly JP, Beijersbergen Van Henegouwen GM et al. (2001) A quantitative assessment of protoporphyrin IX metabolism and phototoxicity in human skin following dose-controlled delivery of the prodrugs 5-aminolaevulinic acid and 5-aminolaevulinic acid-n-pentylester. Br J Dermatol 144:983–990
Theodossiou T, Hothersall JS, Woods EA et al. (2003) Firefly luciferin-activated rose bengal: In vitro photodynamic therapy by intracellular chemiluminescence in transgenic NIH 3T3 cells. Cancer Res 63:1818–1821
Gomer CJ, Razum NJ (1984) Acute skin response in albino mice following porphyrin photosensitization under oxic and anoxic conditions. Photochem Photobiol 40:435–439
Seybold PG, Gouterman M, Callis J (1969) Calorimetric, photometric and lifetime determinations of fluorescence yields of fluorescein dyes. Photochem Photobiol 9:229–242
Giese AC (1980) Hypericism. Photochem Photobiol Rev 5:229–255
Dougherty TJ, Gomer CJ, Henderson BW, et al. (1998) Photodynamic therapy. J Natl Cancer Inst 90:889–905
Moan J, Berg K (1991) The photodegradation of porphyrins in cells can be used to estimate the lifetime of singlet oxygen. Photochem Photobiol 53:549–553
Peng Q, Moan J, Nesland JM (1996) Correlation of subcellular and intratumoral photosensitizer localization with ultrastructural features after photodynamic therapy. Ultrastruct Pathol 20:109–129
Acknowledgments
This study was supported in part by a research scholarship No. SCHI 644/1-1 (to M.L.S.) from the Deutsche Forschungsgemeinschaft (German Research Society, DFG), and by grant NIH 5RO1CA082214-06 (to S.S.G.) from the NIH.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schipper, M.L., Patel, M.R. & Gambhir, S.S. Evaluation of Firefly Luciferase Bioluminescence Mediated Photodynamic Toxicity in Cancer Cells. Mol Imaging Biol 8, 218–225 (2006). https://doi.org/10.1007/s11307-006-0048-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-006-0048-1