Abstract
There is evidence that gonadal hormones may affect the perception of painful stimulation, although the underlying mechanisms remain unclear. This investigation was undertaken to determine whether the adenosine 5′-triphosphate (ATP) receptor subunit, P2X3, is involved in the modulatory action of estrogen in peripheral pain signal transduction in dorsal root ganglion (DRG). The mechanical pain behavior test, real-time quantitative reverse transcription–polymerase chain reaction analysis, and Western blot methods were used to determine the mean relative concentrations and functions of P2X3 receptors in DRG in sham, ovariectomized (OVX), and estradiol replacement (OVX+E2) female rats and in sham and orchiectomized male rats. The mechanical hyperalgesia appeared after ovariectomy, which was subsequently reversed after estradiol replacement, whereas it was not observed after orchiectomy in male rats. Plantar injection of 2′(3′)-O-(2,4,6-trinitrophenyl) ATP (TNP-ATP), a P2X3 and P2X2/3 receptor antagonist, resulted in an increase of the pain threshold force in OVX rats while had no effect on sham rats. Furthermore, A-317491, a selective P2X3/P2X2/3 receptor antagonist, significantly reversed the hyperalgesia of OVX rats. Injection of ATP into the plantars also caused a significant increase of the paw withdrawal duration in OVX rats compared with that seen in the sham group, which became substantially attenuated by TNP-ATP. P2X3 receptors expressed in DRG were significantly increased in both mRNA and protein levels after ovariectomy and then reversed after estrogen replacement, while a similar increase was not observed after orchiectomy in male rats. Furthermore, P2X3 mRNA was significantly decreased 24 h after the application of 17β-estradiol in a concentration-dependent manner in cultured DRG neurons. ICI 182,780, an estrogen receptor antagonist, blocked the reduction in the protein level. These results suggest that the female gonadal hormone, 17β-estradiol, might participate in the control of peripheral pain signal transduction by modulating P2X3 receptor-mediated events in primary sensory neurons, probably through genomic mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been established that gonadal hormones may affect the perception of painful stimuli [1, 2]. Estrogenic modulation of pain is an exceedingly complex, multi-faceted phenomenon, with estrogens producing both pro- and antinociceptive effects [3]. Evidence has shown that estradiol primarily elicits antinociceptive effect on a relatively short-lived pain [2, 3]. The latencies to tailflick and pawlick in response to radiant heat were increased in pro-estrous rats, with higher concentrations of estradiol and progesterone [4–6]. The temporomandibular joint nociceptive behavior of females with proestrus levels of estradiol was significantly lower than that in the diestrus phase [7]. Ovariectomized (OVX) mice developed a robust mechanical hyperalgesia and allodynia [8], which could be reversed by estrogen [9]. Administration of estradiol induced a reduction of nociceptive responses [10] and an increase of latencies in response to heat stimuli [11] and vaginal distension [12] in OVX rats. Furthermore, elevated estrogen and progesterone, as occurs during pregnancy, is antinociceptive [13, 14]. In contrast, the chronic pain conditions such as irritable bowel syndrome, interstitial cystitis, and orofacial pain are more prevalent in females than in males [15, 16]. The threshold to evoke a visceromotor reflex or pressor response to colorectal distention or to activate uterine and vaginal primary afferents is lowest in proestrus [17–19]. Although the reason for this discrepancy is unclear, estrogen modulation of pain is highly specific to the type of nociceptive test, the occurrence of pain, and the characteristics of pain syndromes developed [3, 20].
Estrogen receptors, consisting of two subtypes (ERα and ERβ), have been demonstrated to be widely distributed throughout the central and peripheral nervous systems [21, 22]. Peripheral sensory neurons express both estrogen receptor-α (ERα) and estrogen receptor-β (ERβ), with ERα being selectively localized on small-diameter sensory neurons [23], which have been regarded as nociceptors. Therefore, estrogen can potentially alter the nociceptive process at the primary level.
In peripheral sensory transduction of noxious stimuli, ATP acts through P2X receptors. To date, seven P2X receptors subunits (P2X1−7) have been identified, of which P2X3 and P2X2/3 receptors are expressed in afferent sensory pathways, such as dorsal root ganglia (DRG) and trigeminal ganglia [24, 25], and thus participate in pain perception [26, 27]. In DRG neurons, estradiol attenuated ATP-induced Ca2+ influx through ERα receptors [28] and selectively modulates P2X3 receptor-mediated transient currents [29]. In addition, upregulation of P2X3 receptors in urinary bladder after ovariectomy induced an oversensitivity of urinary bladder to stretch stimuli and thus induced bladder dysfunction [30]. P2X3 receptor expression was increased in DRG 10 days after pregnancy [31]. These results indicate the relation between the expression or function of P2X3 receptors and female hormone levels. In this study, we have investigated the possible effects of estradiol on ATP-mediated peripheral pain signal transduction on DRG and its isolated cultured neurons. We aim to observe the effect by estrogen on the expression and function of homomeric P2X3 receptors in order to elucidate the underlying mechanisms of the effects of sex steroids on pain perception.
Material and methods
Animals
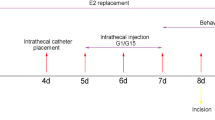
Adult male and female Sprague–Dawley rats were used (200–250 g). The male rats were randomly divided into two groups: a group orchiectomized bilaterally (GDX) and a group receiving the same surgical procedure without removing the testes (sham surgery). The female rats were randomly divided into three groups: a group ovariectomized bilaterally (OVX); a group receiving the same surgical procedure without removing the ovaries (sham surgery), with both groups receiving vehicle injection; and a group ovariectomized bilaterally and receiving estrogen treatment. E2 replacement therapy was carried out in the ovariectomized rat 1 week after surgery and by daily subcutaneous injection of 17β-estradiol (30 μg/kg, 0.4 mL/day); the same volume of vehicle was injected into sham and OVX rats daily. Estrogen plasma levels in the 5 weeks after estrogen replacement was maintained at 108 ± 6.9 pg/mL (n = 8) using an ELISA kit of rat E2 from BioTNT (Transhold Navigation Technology, Shanghai, China). DRG neurons were isolated and cultured from normal female rats. All experimental procedures were approved by the Institutional Animal Care and Use Committee at Second Military Medical University.
Drugs and injections
ATP, 2′(3′)-O-(2,4,6-trinitrophenyl)-ATP (TNP-ATP), A-317491, 17β-estradiol (water-soluble), and charcoal were obtained from Sigma Chemical Co. (Poole, UK). Hank’s balance solution, L-15 medium, and DMEM/F-12 medium were from Gibco Co. (UK). ICI 182,780 was purchased from Tocris. Solutions of ATP and other drugs were prepared using deionized water and stored frozen, except for ICI 182,780 which was dissolved in dimethyl sulfoxide to 1 mM. In the behavior studies, all drugs were then diluted in phosphate-buffered saline (PBS) to the final concentration. In the studies of cultured DRG neurons, 17β-estradiol and ICI 182,780 were then diluted in the medium.
Drug injections were in a volume of 50 μl and delivered into the plantar surface of the hindpaw with a 30-gauge needle. For the dose–response curve, ATP (10–1,000 μmol/L) was administered in a vehicle of normal saline. In the antagonist experiment, TNP-ATP (200 nmol/L) was diluted in normal saline or co-administered with ATP (100 μmol/L) in saline.
Behavior experiments
Behavior test
The mechanical pain threshold was tested before and from 1 to 6 weeks after operation in the three groups of female rats and two groups of male rats. The thermal pain behavior was tested 4 weeks after operation. On the day of experimentation, rats were placed under a Plexiglass dome and allowed to settle for at least 30 min before beginning behavioral experiments.
Mechanical stimulation
The hind paw withdrawal threshold (PWT) was measured to the lateral plantar surface of the tested paw until it withdrew, in response to stimulation of Von Frey filaments (ranging from 0.0174 to 263 g, Institute of Autonomic Neuroscience, London). Each filament was used ten times in ascending order of force and the number and intensity of withdrawal responses were noted. The filaments were applied for 1–2 s with an inter-stimulus interval of 10 s. The withdrawal threshold was taken as the force at which the animal withdrew the paw from at least five consecutive stimuli. The P2X3 and P2X2/3 receptor antagonists, TNP-ATP (200 nmol in 50 μL), and A-317491 (100 nmol in 50 μL) were injected into the rat hindpaw 1 day later.
Thermal stimulation
Thermal nociceptive thresholds were determined according to the method described by McGaraughty et al. [32]. Briefly, through the glass surface, a radiant heat source (BME-410C, Plantar Analgesia Tester, Institute of Biomedical Engineering, CAMS) was focused onto the plantar surface of the hindpaw. The rat’s paw withdrawal latency to this stimulus was recorded. Each animal’s latency score was an average of two trials, which were separated by at least 5 min.
Nocifensive behavioral studies
Nocifensive behavioral studies were conducted using a procedure similar to that described by Hamilton et al. [33]. Briefly, various concentrations of ATP (10–1,000 μmol/L, 50 μL) [34] or PBS was injected subcutaneously into the hindpaw. Following the injection, rats were immediately put back under the Plexiglass dome and the flinching behavior was assessed by determine the paw withdrawal duration (PWD). To study the effect of the P2X receptor antagonist on flinch responses, TNP-ATP (200 nmol/L) was co-administered with the ATP solution (100 μmol/L, 50 μL). Rats were tested twice, with ATP injection in the right hindpaw and co-application of ATP and TNP-ATP in the same hindpaw after an interval of 48 h. The persons conducting the behavioral measurements were blind to the treatments.
Real-time quantitative reverse transcription–polymerase chain reaction analysis
RNA isolation and complementary DNA synthesis
Total RNA was extracted by RNeasy Mini Kit (QIAGEN, Clifton Hill, Australia). DRG were isolated from the three female group rats and the two male group rats 6 weeks after surgery, and purity determination was obtained by ultraviolet spectrophotometer (A260/280), with quantity fixed. Then, the RNA was reversed-transcribed to complementary DNA and cDNA was synthesized from 2 μg of total RNA in a 20 μL reaction mixture containing 1× reverse transcriptase buffer (15 mM MgCl2, 375 mM KCl, 250 mM Tris–HCl at pH 8.3, 50 mM DTT; Promega Corp.), dNTP at 10 mM (Promega Corp.); 20 U of RNase inhibitor (Promega Corp.); 200 U of M-MLV reverse transcriptase (Promega Corp.); and 50 ng of oligo (deoxythymidine)15 primer; reaction time was at least 1 h at 42°C. The cDNA was stored at −20°C for the amplification of the P2X3 gene by quantitative real-time PCR (QT-RT-PCR).
Quantitative real-time PCR
QT-RT-PCR amplifications were performed with SYBRGreen using Roto-gene RG3000 in 20 μL reaction. The solution consisted of 1.0 mL diluted RT-PCR product, 0.25 μM of each of the paired primers, and 10 mL real-time PCR SYBR Green Master Mix. The primer pair used for application of P2X3 was: TGGCGTTCTGGGTATTAAGATCGG (forward); CAGTGGCCTGGTCACTGGCGA (reverse). The PCR conditions for the P2X3 were: 95°C for 2 min, followed by 40 cycles of 95°C, 20 s; 65°C, 25 s; and 72°C, 25 s. To allow standardization of the amount of cDNA added to each PCR reactions and minimize the effects of individual difference on the results, RT-PCR for the housekeeping gene β-actin was performed for each sample. The primer pair used for the application of β-actin was: ATGGTGGGTATGGGTCAGAAGG (forward); TGGCTGGGGTGTTGAAGGTC (reverse). The PCR conditions for β-actin were: 95°C for 2 min, followed by 40 cycles of 95°C, 20 s; 58°C, 25 s; and 72°C, 25 s. The absolute mRNA level in each sample was calculated according to a standard curve set up using serial dilutions of known amounts of specific templates against the corresponding cycle threshold values. Then, the ratio of the P2X3 gene over the reference gene in each sample was obtained to the normalized expression of the target gene.
Western blotting analysis
For the tissue experiments, DRG were harvested from the three female group rats 6 weeks after surgery. For the cell experiments, the cultured DRG neurons were harvested. The samples were homogenized in cold lysis buffer (50 mM Tris–HCl, pH 7.4, 150 mM NaCl, 1% Triton X-100, 1% deoxycholic acid sodium salt, 0.1% SDS, and a protease inhibitor mixture) using a homogenizer (Ultra Turrax T 18 basic, IKA, Germany). The homogenate was centrifuged at 12,000×g (10 min, 4°C) and the supernatant was collected. Total protein concentration was determined by the Bradford method using bovine serum albumin as a standard (Bio-Rad, Hercules, CA). Proteins were separated using SDS-PAGE on 10% Tris–HCl gels (Bio-Rad) and electrophoretically transferred to polyvinylidene difluoride membranes. The membranes were blocked in blocking buffer consisting of 20 mM Tris–HCl, pH 7.4, 137 mM NaCl, 0.1% Tween 20, and 5% nonfat milk at room temperature for 2 h and then incubated with P2X3 primary antibody (1:1,000, Santa Cruz Biotechnology, Santa Cruz, CA) or β-actin (1:1,000, Santa Cruz Biotechnology) overnight at 4°C. The blots were washed, incubated with HRP-conjugated secondary antibody (1:1,000, Proteintech Group, Proteintech, USA) for 2 h at room temperature, and finally visualized in ECL solution (Santa Cruz Biotechnology) for 1 min and exposed onto Kodak film (Rayco company) for 1–30 min. For control of correct gel loading, β-actin quantification was used. To quantify Western blot signals, band density was measured using UMAX PowerLook III (Synpix) and normalized with respect to the control.
Cell culture
Cell culture procedures were selected as reported previously [29]. Namely, eight normal female rats were killed by decapitation. Lumbar DRG were rapidly dissected out. The ganglia were desheathed, cut, and incubated in 4 mL Ca2+- and Mg2+-free Hanks’ balanced salt solution with 10 mM HEPES buffer (pH 7.4; HBSS, Life Technologies) containing 1.5 mg/mL collagenase (class II, Worthington Biochemical Corporation, UK) and 6 mg/mL bovine serum albumin (Sigma) at 37°C for 45 min. The tissue was then incubated in 4 mL HBSS containing 1 mg/mL_trypsin (Sigma) at 37°C for 15 min. The solution was replaced with 1 mL growth medium comprising L-15 medium supplemented with 10% bovine serum, 50 ng/mL nerve growth factor, 0.2% NaHCO3, 5.5 mg/mL glucose, 200 IU/mL penicillin, and 200 IU/mL streptomycin. The ganglia were then dissociated into single neurons by gentle trituration. The neurons were plated onto 35-mm Petri dishes coated with 10 μg/mL laminin (Sigma) and maintained at 37°C in a humidified atmosphere containing 5% CO2. In the experiments, cells were incubated with steroid-free medium (SFM) for 1 day before applying the drugs. This medium was composed of phenol red-deficient DMEM/F-12 (GIBCO) containing 8% heat-inactivated fetal bovine serum that was previously treated with charcoal to remove steroids. The preparation of charcoal-treated serum has been described previously [35].
Statistical analysis
Data were expressed as means ± SEM. Data in the behavior test were analyzed using two-way ANOVA. One-way ANOVA analysis in SPSS11was performed in P2X3 receptor expression levels from groups. The multiple comparisons were then made using the least significant difference test (t test). Differences among the groups were considered statistically significant when the p value was lower than 0.05 (p < 0.05).
Results
Mechanical hyperalgesia after ovariectomy and estrogen reversal of established mechanical hyperalgesia
Changes in the mechanical pain threshold were observed among groups of either female or male rats. In the first week after surgery, Von Frey hair tests showed no difference of PWT (showed with force of von Frey hair) among the three female groups (p > 0.05, n = 8 for each group). In contrast, in the second week after surgery, Von Frey hair tests showed that OVX rats with vehicle developed a robust mechanical hyperalgesia (OVX, 18.7 ± 4.3 g vs. sham, 43.3 ± 7.2 g; Fig. 1a). The hyperalgesia state remained in the following 3, 4, 5, and 6 weeks after surgery (Fig. 1a). The PWT of estrogen replacement rats at week 1 after treatment returned to control values (36.8 ± 12.3 g), and this was maintained at least 5 weeks later. Von Frey hair tests showed no difference of PWT between sham and GDX male rat groups (p > 0.05, n = 8 for each group; Fig. 1b) in the 2, 4, and 6 weeks after orchiectomy.
a Comparison of responses to von Frey hair among sham, OVX, and estrogen-treated (OVX+E2) female rats before and 1–6 weeks after operation (n = 8 for each group). Development of prolonged mechanical hyperalgesia appeared after ovariectomy. Paw withdrawal threshold in response to von Frey filament stimulation decreased in the OVX group. This mechanical hyperalgesia in the OVX group started at 2 weeks after surgery and persisted for at least 6 weeks. Estrogen replacement reversed the hyperalgesia 1 week after daily injection. b Comparison of responses to von Frey hair among sham and GDX male rats before and 2–6 weeks after operation. c Comparison of responses to thermal stimulation among sham and GDX rats 4 weeks after operation
Hindpaw withdrawal latency (PWL) was tested in two groups of female rats and two groups of male rats 4 weeks after operation. The results showed that OVX rats with vehicle had a similar pain behavior to the sham rats (OVX, 7.0 ± 0.3 s vs. sham, 7.0 ± 0.2, n = 6 for each group, p > 0.05; Fig. 1c). In male rats, orchiectomized rats had a similar thermal pain threshold to the sham rats (GDX, 6.2 ± 0.3 s vs. sham, 6.56 ± 0.4 s, p > 0.05, n = 6 for each group; Fig. 1c).
P2X receptors mediate the mechanical hyperalgesia developed after ovariectomy
We then determined whether the mechanical hyperalgesia in OVX rats was mediated by P2X receptors using the P2X3 and P2X2/3 receptor antagonist TNP-ATP. Since the actual concentrations of the antagonists reaching the P2X receptor sites in vivo are uncertain, high concentrations of TNP-ATP (200 nmol in 50 μL), doses similar to those selected by other investigators [36, 37], were used. Compared with PBS, injection of TNP-ATP in the hindpaw had no significant effect on the PWT in the sham group (n = 6, p > 0.05; Fig. 2a), suggesting that P2X receptors do not participate in the responses to von Frey filaments in the sham rat group. A similar experiment was carried out in the OVX group where TNP-ATP reversed the hyperalgesic effect (n = 6, p < 0.05) to 85.8 ± 19.0 g 20 min after injection, which was significantly higher than the control (23.2 ± 2.3 g, Fig. 2b). Thus, the hyperalgesic response in the OVX group was reversed after TNP-ATP application. The TNP-ATP effect was maintained for 60 min and then subsided within 100 min (Fig. 2b). Furthermore, we carried out similar experiments using A-317491, another selective P2X3 receptor antagonist [32], in both sham and OVX rats. The results showed that A-317491 (100 nmol) significantly reversed the hyperalgesia of OVX rats (Fig. 2c) while having no effect on sham rats (Fig. 2d).
Comparison of the paw withdrawal threshold (PWT) after injection of PBS (50 μL), TNP-ATP (200 nmol in 50 μL), or A-317391 (100 nmol in 50 μL) in the rat hindpaws between sham and OVX group. a There was no significant difference between PBS and TNP-ATP injection in the sham group (n = 6). b Compared with that after PBS injection, the mechanical pain threshold after TNP-ATP injection in the hindpaws increased significantly in OVX group (n = 6). *p < 0.05. c There was no significant difference between PBS and A-317491 injection in the sham group (n = 6). d Compared with that after PBS injection, the mechanical pain threshold after A-317491 injection in the hindpaws increased significantly in the OVX group (n = 6). *p < 0.05, **p < 0.01
ATP (100 μmol/L, 50 μL) was applied to the plantar paw of sham, OVX, or estrogen-treated rats. The injection caused rats to repeatedly lift the injected paw (flinching) to apparently avoid putting weight on it. Injection of PBS rarely evoked flinch behaviors in either sham or OVX groups. In sham rats, ATP caused a PWD of 0.5 ± 0.34 s (n = 8, Fig. 3a), and in OVX rats, the responses to ATP were greatly potentiated, with the PWD being 60-fold longer than that in sham rats (60 ± 0 s, p < 0.01, n = 8; Fig. 3a). After estradiol replacement, ATP-induced PWD was decreased to 33.5 ± 14.6 s, which was significantly lower than that in OVX group (p < 0.01, n = 8; Fig. 3a). To confirm that the responses were mediated by P2X receptors, TNP-ATP (200 nmol in 50 μL) was co-injected with ATP (100 μmol/L, 50 μL). In the three groups of rats, the PWD decreased to 0.17 ± 0.17, 12.6 ± 12.6, and 1.08 ± 0.99 s, respectively, which were significantly different than those seen before TNP-ATP injection (p < 0.01, p < 0.01, p < 0.01; Fig. 3a). Injection of TNP-ATP had no effect on rat hindpaw withdrawal behavior. To quantify the effect of ATP, we repeated the experiments using three additional concentrations of ATP and constructed dose–response curves for the nocifensive responses in the three rat groups; the ATP doses producing 50% of the maximum paw lifting duration, EC50, were 624.9 ± 105.9 μmol in the sham rats (n = 8), 265.4 ± 40.7 μmol in the OVX rats (n = 8), and 450.1 ± 15.4 μmol in estrogen-treated rats (n = 8, Fig. 3b).
a ATP (100 μmol/L in 50 μL) induced a significantly longer hindpaw lifting duration in the OVX group (n = 8) compared with that seen in the sham group (n = 8). The responses were reduced significantly when TNP-ATP (200 nmol in 50 μL) was co-injected with ATP. b Dose–response curves for ATP-induced nocifensive responses were obtained from sham, OVX, and estrogen-treated (OVX+E2) rats (n = 8 for each group). The data are expressed as the total hindpaw lifting time. The EC50 was 624.9 ± 105.9 μmol in the sham rats, 265.4 ± 40.7 μmol in the OVX rats, and 450.1 ± 15.4 μmol in estrogen-treated (OVX + E2) rats. *p < 0.05, **p < 0.01, ##p < 0.01 compared with ATP injection alone in each group
Upregulation of P2X3 receptor expression in DRG after ovariectomy
In our study, P2X3 mRNA expression significantly increased after surgical ovariectomy, which is consistent with a previous report [30]. A representative example of the mRNA products for the P2X3 receptor subunit was normalized by the corresponding β-actin mRNA for each of the three treatment groups. We found that the relative level of P2X3 mRNA expression in rat DRG increased by threefold after surgical ovariectomy (OVX; 5.98 ± 0.17 vs. 1.52 ± 0.14, n = 8 for each group, p < 0.01; Fig. 4a). P2X3 expression in rat DRG from the estrogen-treated group differed significantly from OVX animals (5.98 ± 0.17 vs. 3.83 ± 0.19, n = 8, p < 0.05; Fig.4a). In male rats, P2X3 mRNA expression did not change significantly after surgical orchiectomy (1.73 ± 0.14 vs. 1.99 ± 0.24, n = 8 for each group, p > 0.05; Fig. 4b).
a P2X3 mRNA expression in dorsal root ganglia (DRG) from sham, OVX, and estrogen-treated (OVX+E2) female rats 6 weeks after surgery. P2X3 mRNA expression in OVX rats was significantly higher than that either in sham or estrogen-treated (OVX+E2) rats (n = 8 for each group). b P2X3 mRNA expression in DRG from GDX male rats 6 weeks after surgery did not change significantly from that in sham male rats (n = 8 for each group). The expression of P2X3 mRNA was normalized to the β-actin expression in its respective group. c Western blot of total P2X3 receptor protein obtained from dorsal root ganglia (DRG) isolated from sham, OVX, and estrogen-treated (OVX+E2) rat groups 6 weeks after surgery. The total expression of P2X3 receptors, expressed as blot density relative to sham rats (n = 6), was increased significantly in OVX group (n = 6) and differ in estrogen-treated (OVX+E2) group (n = 6). The expression of P2X3 receptors was normalized to the β-actin in its respective group. **p < 0.01, *p < 0.05
Western blot analysis was then used to detect P2X3 receptor protein levels in the intact DRGs from sham, OVX, and estrogen-treated rats. Using the P2X3 antibody, a single band of approximately 57 kDa was recognized in the DRGs (Fig. 4c); the P2X3 receptor protein levels in DRG from OVX rats was increased by 63% after OVX (sham, 0.81 ± 0.13, n = 6; OVX, 1.32 ± 0.29, n = 6, p < 0.01) and reversed to 0.78 ± 0.26 in the estrogen-treated group (n = 6, p < 0.05; Fig. 4c).
Expression of P2X3 receptors in DRG cultured neurons were inhibited by estradiol via estrogen receptors
In order to explore a direct effect of estrogen on P2X3 receptor expression, we determined the P2X3 receptor expression in cultured DRG neurons after treatment with estradiol by QT-RT-PCR and Western blot methods. In these experiments, after the cells were incubated with SFM for 1 day, different concentrations of estradiol were applied. In the cultured DRG neurons, P2X3 mRNA was not changed after a 12-h treatment with 17β-estrodiol (0.1 μmol/L, n = 8 rats, p > 0.05; Fig. 5a), but significantly decreased at 24 h (n = 8 rats, p <0.05; Fig. 5a), and this was maintained until at least 48 h (n = 8 rats, p < 0.05; Fig. 5a). We then found that 17β-estradiol at the lower concentration (0.001–0.01 μmol) also decreased P2X3 mRNA expression significantly (n = 8 rats in each concentration, p < 0.05, with each concentration compared with control; Fig. 5b).
a Time dependence of inhibition by 17β-estradiol on P2X3 mRNA in cultured DRG neurons (n = 8 rats for each column). The expression of P2X3 mRNA was normalized to the β-actin in its respective group. b 17β-estradiol in different concentration (1–100 nmol/L) inhibited P2X3 mRNA expression in cultured DRG neurons (n = 8 rats for each column). The expression of P2X3 mRNA was normalized to the control. c Western blot of total P2X3 receptor protein obtained from cultured dorsal root ganglion neurons. The total expression of P2X3 receptors, expressed as blot density relative to control group (n = 6), was decreased significantly in the estrogen-treated (E2) group (n = 6) and differed in the estrogen- and ICI182780-treated (E2+ICI) group (n = 6). The expression of P2X3 receptors was normalized to the β-actin in its respective group. **p < 0.01, *p < 0.05
Western blot analysis was then used to detect the changes in P2X3 receptor protein levels in the cultured DRG neurons. Using the P2X3 antibody as above, P2X3 receptor protein levels in DRG neurons 24 h after estrogen treatment were decreased by 65% of the control (cont, 1.19 ± 0.22, n = 6; E2, 0. 77 ± 0.13, n = 6, p < 0.05; Fig. 5c). An estrogen receptor antagonist, ICI 182,780 [38], which was applied 30 min before estradiol blocked the estrogen effect on the P2X3 expression to 1.13 ± 0.13 of control (n = 6, p < 0.05 compared with applying estrogen alone; Fig. 5c).
Discussion
Our results showed that the mechanical pain threshold was significantly decreased in OVX female rats. From 2 weeks after ovariectomy, mechanical hyperalgesia developed and persisted for at least 6 weeks after surgery. The hyperalgesia that appeared in OVX rats could be reversed by replacement of estrogen. In contrast, the PWL to thermal stimulation did not differ significantly between sham and OVX rats. These results suggest a role of estrogen in mechanical nociception. Previous reports have found that OVX mice developed a robust mechanical hyperalgesia and allodynia in the abdomen, hind limbs, and proximal tail [8]. The OVX-induced hyperalgesic state of slow onset and long duration could be reversed by estrogen [9]. Administration of estradiol induced a reduction of nociceptive responses in OVX rats [10] and an increase of latencies to response to heat stimuli [11]. Gaumond [39, 40] observed an anti-hyperalgesic effect of 17β-estradiol implanted pellets on the interphase between phase 1 and phase 2 of the formalin test in OVX rats, which was then confirmed and extended in another laboratory [41]. It cannot be concluded that estrogens worsen or alleviate pain per se; rather, estrogens may do either, perhaps depending on the type and chronicity of pain, as well as estrogen level and stability. Insofar as animal and human studies of relatively short-lived pain are concerned, the data suggest that estradiol primarily attenuates pain, or has no effect [3]. The results in this study further support the inhibitory effect by estrogen on the nociceptive sensitivity of the skin.
Some evidence has shown a possible relation between male gonadal hormones and chronic pain. It seems that gonadal and adrenal androgen levels are lower in female and male rheumatoid arthritis patients than in control subjects [42, 43]. Androgen administration seems to be protective in chronic inflammatory disease in both animal models and clinical trials [44]. In this study, the mechanical pain threshold in male rats from 2 to 6 weeks after orchiectomy did not change significantly, and the PWL to thermal stimulation did not change 4 weeks after orchiectomy, suggesting that the effect of androgens may not appear in the physiological condition. Other possibilities could be the different effects of testosterone and 5-alpha dihydrotestosterone, or the possible regulation of secretion of sex hormones that occurs in the pituitary gland or hypothalamus. Since some effects of androgens are mediated by their conversion to estradiol [20, 45], further work will be required to determine their actual pain modulation by using aromatase inhibitors to prevent the conversion of testosterone to estradiol.
Evidence has shown that estradiol administration to OVX rats increases μ-opioid receptor protein in the hypothalamus [46–48] and enkephalin mRNA expression [49], indicating that estrogen can induce an increase in endogenous antinociception and thus reduce pain sensitivity. The P2X3 receptor subtype has been found to be involved in peripheral pain signal transduction [26, 50–53]. To date, changes in the expression and function of P2X3 receptors from DRG neurons in the varied gonadal hormone levels have not been well documented. Though it has been reported that there is a threefold increase in mean P2X3 receptor subunit levels in the urinary bladder after ovariectomy [30], little is known about the alteration of P2X3 expression and function in peripheral pain signal transduction after ovariectomy. In this study, examining the ATP-induced flinch responses, we found that a much lower concentration of ATP was required to produce a similar PWD in OVX rats than in sham rats. Since ATP is a ligand at both P2X and P2Y receptors, experiments using selective P2 receptor antagonists were then carried out to determine which P2 receptor subtype is essential for generating the hyperalgesia after ovariectomy. The large reduction of ATP-induced nociceptive responses and the reversed PWT in OVX rats by TNP-ATP suggests that peripheral P2X1, P2X2/3, P2X3, and P2X7, but not P2X4 and P2X5 receptor subtypes, are likely to be involved in the von Frey hair filament responses. Furthermore, A-317491, a more potent and selective antagonist of P2X3/P2X2/3 receptor [32], significantly reversed the mechanical hyperalgesia of OVX rats. Since the expression of P2X1, P2X4, and P2X7 are low in DRG neurons [24, 53, 54], these observations suggest that P2X3 and P2X2/3 are likely to be the receptor subtypes that are enhanced after ovariectomy. The ovariectomized state might alter peripheral pain via P2X3 subunit-contained receptors located on the peripheral terminals of DRG neurons.
The large increase in P2X3 receptor expression from DRG after ovariectomy in female rats, but not orchiectomy in male rats, in this study further suggests that the increase in P2X3 receptor function is the underlying mechanism for the observed abnormal nociceptive responses in OVX groups. Studying mechanical hyperalgesia in OVX rats, we have shown that estrogen can potentially alter the nociceptive process at the primary afferent level. We then found that estrogen replacement reversed the increase of P2X3 expression in DRG in both mRNA and protein levels. Moreover, applying estrogen directly to the cultured DRG neurons resulted in a decrease of P2X3 receptor expression in both mRNA and protein levels, which could be blocked by an estrogen receptor antagonist. Though this study cannot exclude the possible effects by progesterone or the other components in the gonadal hormones secreted from the ovary, it does suggest that post-transcriptional changes could account for the changes in protein and mRNA expression of P2X3 receptors by estrogen.
One of the mechanisms contributing to the inhibition by estrogen on P2X3 receptors at the transcriptional level could be the genomic pathway via intracellular estrogen receptors (ERs). Li et al. [55] recently reported that the sex difference in basal mechanical pain threshold and inflammatory hypersensitivity is eliminated in mice lacking either the estrogen α receptors or β receptors, suggesting that both of these receptors are involved in the estrogen modulation of pain perception. Furthermore, estrogens acting primarily through the activation of estrogen receptor β (ERβ) may also have a developmental role that affects spinal cord structures important for the transmission of nociceptive information [56]. As we have reported previously, estrogen rapidly inhibited the P2X3 receptor-mediated currents in cultured DRG neurons [29], which could be blocked by an ER antagonist, ICI, 182,780. In this study, ICI 182,780 blocked the estrogen inhibitory effect on P2X3 expression in DRG neurons. These results suggest a role of estrogen on P2X3 function via both non-genomic and genomic pathways. Other factors, e.g., changes in the modulation of the receptor by protein kinases [57] or changes in channel properties [58], may also contribute to the increase in P2X3 receptor function.
Other factors that we cannot exclude could be possible changes in the ATP levels in various estrogen states or the regulation of secretion of sex hormones that occurs in the pituitary gland or hypothalamus. There may be supraspinal modulation and, potentially, hormonal effects may be mediated directly by the hormones themselves or by the processes which control the release of the hormones.
Although the mechanisms underlying the altered P2X3 receptor-mediated nociceptive responses in the OVX rats remain unclear, our studies have shown that estrogen inhibited P2X3 receptor expression through a genomic mechanism and the upregulation of P2X3 receptors in DRG neurons from the OVX groups may play a central role in mediating the abnormal nociceptive responses after ovariectomy in female rats. Therefore, this study establishes the potential of the P2X3 receptor as a target for pain therapy, especially in females.
References
Fillingim RB (2000) Sex, gender, and pain: women and men really are different. Curr Rev Pain 4(1):24–30
Greenspan JD, Craft RM, LeResche L, Arendt-Nielsen L, Berkley KJ, Fillingim RB, Gold MS, Holdcroft A, Lautenbacher S, Mayer EA, Mogil JS, Murphy AZ, Traub RJ (2007) Consensus Working Group of the Sex, Gender, and Pain SIG of the IASP. Pain 132(Suppl 1):S26–S45
Craft RM (2007) Modulation of pain by estrogens. Pain 132:S3–S12
Butcher RL, Collins WE, Fugo NW (1974) Plasma concentration of LH, FSH, prolactin, progesterone, and estradiol-17beta throughout the 4-day estrous cycle of the rat. Endocrinology 94:1704–1708
Frye CA, Bock BC, Kanarek RB (1992) Hormonal milieu affects tailflick latency in female rats and may be attenuated by access to sucrose. Physiol Behav 52:699–706
Frye CA, Cuevas CA, Kanarek RB (1993) Diet and estrous cycle influence pain sensitivity in rats. Pharmacol Biochem Behav 45:255–260
Fischer L, Torres-Chávez KE, Clemente-Napimoga JT, Jorge D, Arsati F, de Arruda Veiga MC, Tambeli CH (2008) The influence of sex and ovarian hormones on temporomandibular joint nociception in rats. J Pain 9(7):630–638
Sanoja R, Cervero F (2005) Estrogen-dependent abdominal hyperalgesia induced by ovariectomy in adult mice: a model of functional abdominal pain. Pain 118(1–2):243–253
Sanoja R, Cervero F (2008) Estrogen modulation of ovariectomy-induced hyperalgesia in adult mice. Eur J Pain 12:573–581
Stoffel EC, Ulibarri CM, Craft RM (2003) Gonadal steroid hormone modulation of nociception, morphine antinociception and reproductive indices in male and female rats. Pain 103:285–302
Formanl LJ, Tingle V, Estilow S, Cater J (1989) The response to analgesia testing is affected by gonadal steroids in the rat. Life Sci 45(5):447–454
Bradshaw HB, Berkley KJ (2002) Estrogen replacement reverses ovariectomy-induced vaginal hyperalgesia in the rat. Maturitas 41:157–165
Gintzler AR, Bohan MC (1990) Pain thresholds are elevated during pseudopregnancy. Brain Res 507(2):312–316
Dawson-Basoa ME, Gintzler AR (1998) Gestational and ovarian sex steroid antinociception: synergy between spinal and opioid system. Brain Res 757:37–42
Unruh AM (1996) Gender variations in clinical pain experience. Pain 65:123–167
Berkley KJ (1997) Sex differences in pain. Behav Brain Sci 20:371–380
Robbins A, Berkley KJ, Sato Y (1992) Estrous cycle variation of afferent fibers supplying reproductive organs in the female rat. Brain Res 596(1–2):353–356
Sapsed-Byrne S, Ma D, Ridout D, Holdcroft A (1996) Estrous cycle phase variations in visceromotor and cardiovascular responses to colonic distension in the anesthetized rat. Brain Res 742(1–2):10–16
Holdcroft A, Sapsed-Byrne S, Ma D, Hammal D, Forsling ML (2000) Sex and oestrous cycle differences in visceromotor responses and vasopressin release in response to colonic distension in male and female rats anaesthetized with halothane. Br J Anaesth 85(6):907–910
Aloisi AM, Bonifazi M (2006) Sex hormones, central nervous system and pain. Horm Behav 50:1–7
Bettini E, Pollio G, Santagati S, Maggi A (1992) Estrogen receptor in rat brain: presence in the hippocampal formation. Neuroendocrinology 56(4):502–508
Papka RE, Srinivasan B, Miller KE, Hayashi S (1997) Localization of estrogen receptor protein and estrogen receptor messenger RNA in peripheral autonomic and sensory neurons. Neuroscience 79(4):1153–1163
Taleghany N, Sarajari S, DonCarlos LL, Gollapudi L, Oblinger MM (1999) Differential expression of estrogen receptor alpha and beta in rat dorsal root ganglion neurons. J Neurosci Res 57:603–615
Xiang Z, Bo X, Burnstock G (1998) Localization of ATP-gated P2X receptor immunoreactivity in rat sensory and sympathetic ganglia. Neurosci Lett 256(2):105–108
Burnstock G (2007) Physiology and pathophysiology of purinergic neurotransmission. Physiol Rev 87(2):659–797
Cockayne DA, Hamilton SG, Zhu QM, Dunn PM, Zhong Y, Novakovic S, Malmberg AB, Cain G, Berson A, Kassotakis L, Hedley L, Lachnit WG, Burnstock G, McMahon SB, Ford AP (2000) Urinary bladder hyporeflexia and reduced pain-related behaviour in P2X3-deficient mice. Nature 407(6807):1011–1015
Cockayne DA, Dunn PM, Zhong Y, Rong W, Hamilton SG, Knight GE, Ruan HZ, Ma B, Yip P, Nunn P, McMahon SB, Burnstock G, Ford AP (2005) P2X2 knockout mice and P2X2/P2X3 double knockout mice reveal a role for the P2X2 receptor subunit in mediating multiple sensory effects of ATP. J Physiol 567(Pt 2):621–639
Chaban VV, Mayer EA, Ennes HS, Micevych PE (2003) Estradiol inhibits ATP-induced intracellular calcium concentration increase in dorsal root ganglia neurons. Neuroscience 118:941–948
Ma B, Rong W, Dunn PM, Burnstock G (2005) 17β-estradiol attenuates α,β-meATP-induced currents in rat dorsal root ganglion neurons. Life Sci 76(22):2547–2558
Carley ME, Cliby WA, Spelsberg TC (2002) P2X3 receptor subunit messenger RNA expression in the female mouse bladder after oophorectomy with or without estrogen replacement. Am J Obstet Gynecol 187(1):103–106
Papka RE, Hafemeister J, Storey-Workley M (2005) P2X receptors in the rat uterine cervix, lumbosacral dorsal root ganglia, and spinal cord during pregnancy. Cell Tissue Res 321(1):35–44
McGaraughty S, Wismer CT, Zhu CZ, Mikusa J, Honore P, Chu KL, Lee CH, Faltynek CR, Jarvis MF (2003) Effects of A-317491, a novel and selective P2X3/P2X2/3 receptor antagonist, on neuropathic, inflammatory and chemogenic nociception following intrathecal and intraplantar administration. Br J Pharmacol 140(8):1381–1388
Hamilton SG, Wade A, McMahon SB (1999) The effects of inflammation and inflammatory mediators on nociceptive behaviour induced by ATP analogues in the rat. Br J Pharmacol 126(1):326–332
Sawynok J, Reid A (1997) Peripheral adenosine 5′-triphosphate enhances nociception in the formalin test via activation of a purinergic p2X receptor. Eur J Pharmacol 330(2–3):115–121
Gorodeski GI (1998) Estrogen increases the permeability of the cultured human cervical epithelium by modulating cell deformability. Am J Physiol 275:C888–C899
Jarvis MF, Wismer CT, Schweitzer E, Yu H, van Biesen T, Lynch KJ, Burgard EC, Kowaluk EA (2001) Modulation of BzATP and formalin induced nociception: attenuation by the P2X receptor antagonist, TNP-ATP and enhancement by the P2X(3) allosteric modulator, cibacron blue. Br J Pharmacol 132(1):259–269
Tsuda M, Shigemoto-Mogami Y, Koizumi S, Mizokoshi A, Kohsaka S, Salter MW, Inoue K (2003) P2X4 receptors induced in spinal microglia gate tactile allodynia after nerve injury. Nature 424(6950):778–783
Wakeling AE, Dukes M, Bowler JA (1991) A potent specific pure antiestrogen with clinical potential. Cancer Res 51:3867–3873
Gaumond I, Arsenault P, Marchand S (2002) The role of sex hormones on formalin-induced nociceptive responses. Brain Res 958(1):139–145
Gaumond I, Arsenault P, Marchand S (2005) Specificity of female and male sex hormones on excitatory and inhibitory phases of formalin-induced nociceptive responses. Brain Res 1052(1):105–111
Mannino CA, South SM, Quinones-Jenab V, Inturrisi CE (2007) Estradiol replacement in ovariectomized rats is antihyperalagesic in the formalin test. J Pain 8(4):334–342
Cutolo M, Villaggio B, Foppiani L, Briata M, Sulli A, Pizzorni C, Faelli F, Prete C, Felli L, Seriolo B, Giusti M (2000) The hypothalamic–pituitary–adrenocortical and gonadal axis function in rheumatoid arthritis. Z Rheumatol 59(Suppl):S65–S69
Navarro MA, Nolla JM, Machuca MI, González A, Mateo L, Bonnin RM, Roig-Escofet D (1998) Salivary testosterone in postmenopausal women with rheumatoid arthritis. J Rheumatol 25:1059–1062
Green PG, Dahlqvist SR, Isenberg WM, Strausbaugh HJ, Miao FJ, Levine JD (1999) Sex steroid regulation of the inflammatory response: sympathoadrenal dependence in the female rat. J Neurosci 19:4082–4089
Beyenburg S, Stoffel-Wagner B, Bauer J, Watzka M, Blumcke I, Bidlingmaier F, Elger CE (2001) Neuroactive steroids and seizure susceptibility. Epilepsy Res 44:141–153
Hammer RP Jr, Bridges RS (1987) Preoptric area opiods and opiate receptors increase during pregnancy and decrease during lactation. Brain Res 420(1):48–56
Dondi D, Limonta P, Maggi R, Piva F (1992) Effects of ovarian hormones on brain opioid binding sites in castrated female rats. Am J Physiol 263(3 Pt 1):E507–E511
Quinones-Jenab V, Jenab S, Ogawa S, Inturrisi C, Pfaff DW (1997) Estrogen regulation of mu-opioid receptor mRNA in the forebrain of female rats. Brain Res Mol Brain Res 47(1–2):134–138
Amandusson A, Hallbeck M, Hallbeck AL, Hermanson O, Blomqvist A (1999) Estrogen-induced alterations of spinal cord enkephalin gene expression. Pain 83(2):243–248
Burnstock G, Wood JN (1996) Purinergic receptors: their role in nociception and primary afferent neurotransmission. Curr Opin Neurobiol 6(4):526–532
Chen CC, Akopian AN, Sivilotti L, Colquhoun D, Burnstock G, Wood JN (1995) A P2X purinoreceptors expressed by a subset of sensory neurons. Nature 377:428–431
Lewis C, Neidhart S, Holy C, North RA, Buell G, Surprenant A (1995) Coexpression of P2X2 and P2X3 receptor subunits can account for ATP-gated currents in sensory neurons. Nature 377:432–435
North RA (2004) P2X3 receptors and peripheral pain mechanisms. J Physiol 554:301–308
Kobayashi K, Fukuoka T, Yamanaka H, Dai Y, Obata K, Tokunaga A, Noguchi K (2005) Differential expression patterns of mRNAs for P2X receptor subunits in neurochemically characterized dorsal root ganglion neurons in the rat. J Comp Neurol 481:377–390
Li L, Fan X, Warner M, Lili Li XuX-J, Gustafsson J-A, Wiesenfeld-Hallin Z (2009) Ablation of estrogen receptor α or β eliminates sex differences in mechanical pain threshold in normal and inflamed mice. Pain 143:37–40
Fan XT, Kim H-J, Warner M, Gustafsson J (2007) Estrogen receptor β is essential for sprouting of nociceptive primary afferents and for morphogenesis and maintenance of the dorsal horn interneurons. Proc Natl Acad Sci USA 104:13696–13701
Xu GY, Huang LY (2002) Peripheral inflammation sensitizes P2X receptor mediated responses in rat dorsal root ganglion neurons. J Neurosci 22:93–102
Xu GY, Huang LY (2004) Ca2+/calmodulin-dependent protein kinase II potentiates ATP responses by promoting trafficking of P2X receptors. Proc Natl Acad Sci USA 101:11868–11873
Acknowledgment
This study was supported by National Natural Science Foundation of China (NSFC, no. 30570597, B. Ma) and Program of Changjiang Scholar and innovative team. We are deeply grateful to Dr. Gillian E. Knight (from the Autonomic Neuroscience Centre, University College Medical School, UK) for her kind assistance in English writing.
Author information
Authors and Affiliations
Corresponding authors
Additional information
The first two authors contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ma, B., Yu, Lh., Fan, J. et al. Estrogen modulation of peripheral pain signal transduction: involvement of P2X3 receptors. Purinergic Signalling 7, 73–83 (2011). https://doi.org/10.1007/s11302-010-9212-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-010-9212-9