Abstract
Objective
Maxillary sinus anterior wall depression (AWD) has been associated with patterns such as the presence of panoramic innominate line and silent sinus syndrome. The aim of this study was to evaluate the relationship between AWD of maxillary sinus and both maxillary sinus opacity and the presence of innominate line using computed tomography (CT) and panoramic radiography (PR).
Materials and methods
250 CT and PR images (122 female, 128male) which had been taken for various reasons were randomly selected from the radiology archive of the our department. Innominate line visibility in PR is divided into three as invisible, obscure and clear. On CT images, the distance between guide line and the deepest point of the maxillary sinus anterior wall was calculated as AWD. The presence of maxillary sinus opacity and maxillary sinus AWD were evaluated on CT images. Demographic information such as age, gender and localization of the findings were noted in all measurements.
Results
In 143 (57.2%) patients, the innominate line (clear and obscure patterns) was seen on the PR images. AWD was observed in 104 (41.6%) CT images. The presence of maxillary sinus opacity was observed in 117 (46.8%) images. The mean right anterior wall depth was 5.69 and 4.88 in males and females, respectively, while the mean left anterior wall depth was 5.64 and 4.94 in males and females, respectively. Right wall depth was significantly higher in males (p < 0.05).There was no statistically significant difference in left wall depth (p > 0.05).
Conclusions
Anterior wall depression was found to be associated with both maxillary sinus opacity and the visibility of the innominate line. Patients with AWD should be considered as susceptible to maxillary sinus diseases.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The development of minimally invasive surgical techniques has made it necessary to have a better understanding of the anatomy of the paranasal sinus. Lack of information about this anatomic region can cause serious complications, such as the leakage of cerebrospinal fluid, meningitis, or blindness, at the time of operation [1]. Anatomic variations in sinonasal structures are also responsible for the etiology of chronic and recurrent sinusitis [2].
Panoramic radiography (PR) and computed tomography (CT) are routinely used for radiographic examination of sinonasal region [3]. However, most anatomical structures cannot be distinguished due to the superposition of direct radiographs. CT is the superior imaging method because it provides detailed anatomical information about the region. In addition, cross-sectional images without bone superposition allow a more accurate examination [4].
The maxillary sinus is adjacent to the oral cavity, nasal cavity, pterygopalatine fossa, infratemporal fossa, and orbit. The maxillary sinus, as the largest of the paranasal sinuses, is the most common location for oral complications of dental origin [5]. In PR images, the structures around the maxillary sinus are complex and difficult to see. In this area, various lines, such as orbital and sinus base lines, medial and posterior wall lines, and innominate lines, are available on PR [6]. The panoramic innominate line crosses the outer third of the maxillary sinus vertically and consists of the posterior surface of the zygomatic process of the maxillary bone [7]. This diagonal line can be seen from the lower part of the panoramic innominate line to the middle part of the orbital baseline and is considered a characteristic feature after Caudwell–Luc surgery [6].
Maxillary sinus anterior wall depression (AWD) has been associated with certain patterns, such as the presence of the innominate line and silent sinus syndrome [6]. The latter is characterized by painless facial asymmetry, which is caused by chronic maxillary sinus atelectasis, enophthalmos, and maxillary sinus AWD [8].
Inflammatory disease is the major cause of maxillary sinus opacity. In the literature, inflammatory etiologies (chronic rhino sinusitis, either with or without nasal polyposis, antrochoanal polyp, and fungal sinusitis) were responsible for 46–70% of cases of maxillary sinus opacification [9,10,11]. However, the relationship between maxillary AWD and maxillary sinus opacities has not been investigated in any published studies.
The aim of this study was to evaluate the relationship between AWD of the maxillary sinus for both maxillary sinus opacity and visibility of the innominate line via CT and PR.
Materials and methods
This retrospective study was approved by the Local Clinical Research Ethics Committee of Hatay Mustafa Kemal University (Decision date: 10/31/2019, decision number: 08), and the study protocol was conducted following the principles of the Declaration of Helsinki.
In total, 250 patients who had both CT and PR images (122 females, 128 males), which had been taken for various reasons (temporomandibular joint problems, orthodontic treatment, mandibular cysts or tumors, etc.), were randomly selected from the archive of the Dentomaxillofacial Radiology Department. Excluded images included those of patients who either had a pathological fracture, had undergone surgery in the head and neck region, had suffered trauma that affected the integrity of the maxillary sinus, or had a cleft lip and/or palate. Moreover, poor diagnostic quality CT and PR images as well as images with motion artifacts or technical errors were also excluded. For standardization, all included panoramic radiographs were obtained on the same devices with the same exposure modalities and were taken by the same technician.
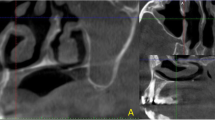
Based on a study by Yoshida et al. [6], innominate line visibility in PR was divided into three categories: invisible (no line is visible), obscured (a partially visualized or very thin feature of the line is evident), and clear (a continuous line is clearly observable from the lower edge of the panoramic innominate line to the middle of the orbital floor line) (Fig. 1).
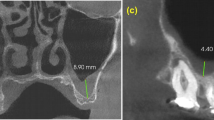
On CT images, after a guide line was drawn between the anterior nasal spina and the anterior line of the maxillary zygomatic process, the distance between this guide line and the deepest point of the maxillary sinus anterior wall was calculated as the AWD (Fig. 2). All measurements were performed using an image analysis program (Image J, 1.4 v, National Institutes of Health, Bethesda, MD, USA).
The presence of maxillary sinus opacity was evaluated on CT images with maxillary sinus AWD. Demographic information, such as age, gender, and localization of the findings, were noted in all measurements, which were performed by two dentomaxillofacial radiologists who had 6 years (G.S.) and 5 years (C.A.B.) of clinical experience. Both observers had previously been calibrated with all measurements, and all analyses were performed at the same time.
Statistical analyses were performed using SPSS 21.0software (SPSS Inc., Chicago, IL, USA). The conformity of the parameters to the normal distribution was investigated by the Kolmogorov–Smirnov test. All data were distributed paranormally; therefore, the relationship between the parameters and age was evaluated with the Kruskal–Wallis H test, and the relationship with the genders was evaluated using the chi-square test. The relationship between AWD depth and gender was evaluated by the Mann–Whitney U test due to the paranormal data distribution. p values < 0.05 were considered statistically significant.
Results
The inter-observer agreement for all measurements was quite high and meaningful (ICC at 0.7 and above indicates good agreement).
The images of 250 patients (128 males; 122 females) were evaluated for this study. The mean ages (range 15–84 years) were 43.4 years (males) and 42.9 years (females). In 143 (57.2%) patients, the innominate line (clear and obscure patterns) was seen on the PR image (Table 1).Innominate line invisibility was significantly higher in females (p < 0.05), while the presence of a clear innominate line was significantly higher in males (p < 0.05). Although there was no statistically significant difference, the presence of an obscure innominate line was higher in males (Table 1). There was no significant difference between the innominate line visualization pattern and age (p > 0.05) (Table 2).
Anterior wall depression was observed on 104 (41.6%) CT images, including 22, 18, and 64 images in the right, left, and bilateral localizations, respectively (Table 1). Age values were found to be higher in the right AWD group than in the other groups, but they were lower in the non-anterior wall depression group than they were in the left and bilateral AWD groups (p < 0.05) (Table 2).There was a significant difference between the genders and AWD (p < 0.05). Although the right wall depth was significantly higher in males (p < 0.05), there was no statistically significant difference between the left wall depth and gender (p > 0.05) (Table 3).
The presence of maxillary sinus opacity was observed on 117 (46.8%) images (Table 1). Unilateral and bilateral maxillary sinus opacity were statistically significantly higher in males (p < 0.05 for both opacities). Age values were higher in patients with right opacity compared to the other groups (p < 0.05) (Table 3).
A positive correlation was found between anterior sinus depression and maxillary sinus opacity (p < 0.05) and AWD and innominate line visualization (p < 0.05).
Discussion
In this study, we aimed to evaluate the relationship between AWD and the opacity of maxillary sinus and visibility of the innominate line and found a correlation between both. Similar to a study by Ohba et al. [3], the present study found that AWD and panoramic innominate line visibility have a positive correlation; we found that 107 (42.8%) images were invisible, and 32 (12.8%) images had a clear innominate line. In contrast to Ohba et al. [3], the literature states that this line can be seen in clinical images without any surgical history [6]. Therefore, we preferred to evaluate patients who had not surgical operation in the area of interest.
Yoshida et al. [6] compared the relationship between innominate line visibility and AWD. They calculated that, in 408 (12.1%) sinuses, the diagonal line (clear and obscure patterns) was seen on the panoramic image. In our study, a higher result (57.2%) was found. They also stated that the incidences of the obscure and clear patterns increased with increasing age groups. The mean wall depths were 2.91, 4.80, and 7.28 mm for the invisible, obscure, and clear patterns, respectively. Their study emphasized that the decrease in age-related sinus volume may be partially due to AWD and that there is a relationship between the innominate line and AWD. In our study, the anterior wall depth was calculated as 5.40 mm on the right and 5.44 mm on the left. Similar to Yoshida et al. [6], our study found that AWD and panoramic innominate line visibility have a positive correlation.
Silent sinus syndrome is characterized by painless enophthalmos associated with chronic maxillary sinus atelectasis [12]. The cause of this atelectasis is thought to be chronic maxillary sinus obstruction with hypoventilation, which is a state that eventually causes negative pressure to develop within the sinus [12, 13]. Radiologically, the sinus is usually opacified, the maxillary infundibulum is occluded, and there is inward retraction of the sinus walls due to a decrease in sinus volume [13,14,15]. An opacified hypoplastic maxillary sinus may represent a less severe form of silent sinus syndrome with a smaller sinus volume and shorter, thicker sinus walls, which afford the sinus protection against osteolysis and negative pressure effects [8]. Another cause of maxillary sinus atelectasis is thought to be maxillary sinus AWD [6].
In the literature, no articles were found that had evaluated the relationship between maxillary sinus opacity and AWD. In our study, a significant relationship was found between maxillary sinus opacity and AWD. This may be the cause of negative air pressure because wall depression in the maxillary sinus disrupts sinus ventilation and makes it susceptible to infection. By increasing the number of samples or evaluating samples from different races, variations in anatomical structures, such as AWD depth and innominate line visibility, can be examined. Changes in opacities according to parameters in patients with different maxillary sinus diseases can be examined in future studies.
Conclusion
In conclusion, AWD was found to be associated with both maxillary sinus opacity and the visibility of the innominate line. Patients with AWD should be considered susceptible to maxillary sinus diseases. When this variation is detected in radiographic examinations, measurements may be performed to describe the depression depth and the decreased volume of the maxillary sinus to prevent the development of disease. Patients with AWD should avoid periapical infections of the maxilla posterior teeth, which may affect the sinus, and early intervention of dental problems should be used without affecting the tooth apex to avoid viral upper respiratory infections and allergic diseases, such as asthma. Further studies are needed on this subject to clearly understand the relationship between maxillary sinus AWD and maxillary sinus opacity.
References
Keast A, Sofie Y, Dawes P, Lyons B. Anatomical variations of the paranasal sinuses in Polynesian and New Zealand European computerized tomography scans. Otolaryngol Head Neck Surg. 2008;139(2):216–21.
Li L, Yang J, Chu Y, Wu W, Xue J, Liang P, et al. A novel augmented reality navigation system for endoscopic sinus and skull base surgery: a feasibility study. PLoS ONE. 2016;11(1):1–17.
Ohba T, Morimoto Y, Nagata Y, Tanaka T, Kito S. Comparison of the panoramic radiographic and CT features of post-Caudwell Luc maxillary sinuses. Dentomaxillofac Radiol. 2000;29:280–5.
Ariji Y, Ariji E, Yoshiura K, Kanda S. Computed tomographic indices for maxillary sinus size in comparison with sinus volume. Dentomaxillofac Radiol. 1996;25:19–24.
Favato MN, Vidigal BC, Cosso MG, Manzi FR, Shibli JA, Zenóbio EG. Impact of human maxillary sinus volume on grafts dimensional changes used in maxillary sinus augmentation: a multislice tomographic study. Clin Oral Implants Res. 2015;26(12):1450–5.
Yoshida K, Fukuda M, Gotoh K, Ariji E. Depression of the maxillary sinus anterior wall and its influence on panoramic radiography appearance. Dentomaxillofac Radiol. 2017;46(6):20170126.
Katayama H, Ohba T, Ogawa Y. Panoramic innominate line and related roentgen anatomy of the facial bones. Oral Surg Oral Med Oral Pathol. 1974;37(1):131–7.
Illner A, Davidson HC, Harnsberger HR, Hoffman J. The silent sinus syndrome: clinical and radiographic findings. AJR Am J Roentgenol. 2002;178:503–6.
Ahsan F, El-Hakim H, Ah-See KW. Unilateral opacification of paranasal sinus CT scans. Otolaryngol Head Neck Surg. 2005;133(2):178–80.
Rudralingam M, Jones K, Woolford TJ. The unilateral opaque maxillary sinus on computed tomography. Br J Oral Maxillofac Surg. 2002;40:504–7.
Kaplan BA, Kountakis SE. Diagnosis and pathology of unilateral maxillary sinus opacification with or without evidence of contralateral disease. Laryngoscope. 2004;114:981–5.
Montgomery WW. Mucocele of the maxillary sinus causing enophthalmos. Eye Ear Nose Throat Mon. 1964;43:41–4.
Kass ES, Salman S, Rubin PAD, Weber AL, Montgomery WW. Chronic maxillary atelectasis. Ann Otol Rhinol Laryngol. 1997;106:109–16.
Gillman GS, Schaitkin BM, May M. Asymptomatic enophthalmos: the silent sinus syndrome. Am J Rhinol. 1999;13(6):459–62.
Wan MK, Francis IC, Carter PR, Griffits R, vanRooljen ML, Coroneo MT. The spectrum of presentation of silent sinus syndrome. J Neuroophthalmol. 2000;20(3):207–12.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Gozde Serindere and Ceren Aktuna Belgin declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Serindere, G., Aktuna Belgin, C. An evaluation of the relationship between maxillary sinus anterior wall depression and maxillary sinus opacity by computed tomography and panoramic radiography. Oral Radiol 36, 383–388 (2020). https://doi.org/10.1007/s11282-020-00436-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11282-020-00436-z