Abstract
The paper proposes a system for an early warning on the prosthesis performance, in particular in terms of micro- displacements of the implant-prostheses connection, enabling actions to prevent fatal damages to the structure. The system includes a sensor for micro-displacement to be inserted in the prosthesis volume, with embedded wireless communications capabilities. Key elements of the system are the system enabling the wireless transmission of the recorded data and the molecular and biochemical approaches to unravel possible metabolic alterations. For these two elements, the paper presents and discusses several solutions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The maturity of Information and Communications Technology (ICT) is pushing forward innovative and multidisciplinary applications that are dramatically improving the penetration of ICT itself in the everyday life of global citizens.
Among the multidisciplinary scenarios, Tele-Health is playing a key-role due to its direct impact in the Quality of Life (QoL) of people at individual and social levels.
Furthermore, the increase in the number and average age of the elderly people in industrialized areas is pointing out some Health areas where the ICT contribution could change dramatically the performance and the cost of the cures for both the public health system and the private patients.
One of these areas is Dentistry, where we are assisting to a significant growth of technology-driven approaches to the cure.
This contribution deals with the above technology-driven trend for Dentistry.
The paper will address a harmonic merging between ICT—in particular integrated wireless and sensing technologies—with advanced fixed implant-supported prosthesis. One of the prerequisites for long-term success in implant rehabilitation is the stability of the restoration. The coupling and the stability between implants and prosthetic structures is usually ensured by connection screws, which are tightened by using torque wrenches. Nevertheless, screw loosening can occur, due to off-axis loading generated during masticatory function. A poor fit as well as mobility between structures introduces harmful tensile, compressive and bending forces, which may be dangerous for the osseointegration process and/or lead to failure of the components (connection screws, prosthetic framework). This could bring about the requirement for new surgical and/or prosthodontic procedures with a consequent increase of treatment time and costs for both patients and clinical-laboratory team.
Therefore, it would be extremely important to be able to record any micro-displacement at least daily and inform the dentist about it. This would require the possibility to wireless transmitting the data recorded by a sensor, which can be put inside the prosthesis, to a device outside the mouth.
In the past two decades several devices (and related patents) have been developed allowing intraoral sensing using different mechanical and electronic sensing principles [1, 2]. However, the invasive nature of wired connections, between the oral cavity and a readout unit placed outside could be uncomfortable for the patient impairing physiological functions. The huge advancement in micromachining techniques has allowed the fabrication of micro-biosensors featuring a wireless transmission. The reduction of the system dimensions reduces the discomfort in the oral cavity and enable easy implantation with no tissue injury while collecting real-time data. Although several intraoral sensing systems have been developed (mainly prototypes) which allow the wireless transmission of data [3–7], the potential opportunities offered by this sector have not been truly exploited yet. In this paper, several possible communication solutions (technologies, architectures) that might be considered (from the mouth to the dentist office) for this specific application are discussed.
Moreover, the presence of the sensors inside the prostheses might cause metabolic alterations (causing inflammation or tissue damage). Therefore, the molecular and biochemical approaches undertaken to unravel possible metabolic alterations (with particular reference to quantification of recognized markers of inflammation or tissue damage), occurring during prosthesis implantation and long-term wearing, will be discussed.
The paper is organized as follows: Sect. 2 explains the specific dentistry application, formulating the problem to which the proposed system should provide a solution, and finally identifying the requirements of the communication part; Sect. 3 presents several possible technology solutions for the wireless transmission of the recorded data; Sect. 4 presents approaches for the epidemiological and clinical study that must be performed; Conclusions are drawn in Sect. 5.
2 Implant-Supported Prostheses
This Section presents the specific dentistry application outlining what it would be important to monitor and when, thus defining the requirements of the wireless communication architecture that is needed.
2.1 Implant-Prosthesis Connection Micro-displacements
A dental implant (fixture) is a biocompatible device, surgically placed into mandibular or maxillary bone, which supports a prosthesis (see Fig. 1) thus allowing the replacement of the teeth loss due to caries, periodontal disease, injuries, or other reasons [8]. The effectiveness of a dental implantation is identified by the proper development of the osseo-integration process at the bone-implant interface, i.e. the bone growth over the implant surface. Osseo-integrated implants may be considered artificial roots, and, like tooth roots, they are secured in the jawbone and are not visible once surgically placed. Once the healing process is completed, an abutment is screwed into the fixture in order to join the implant to a restoration (prosthesis), which replaces the tooth part visible in the mouth. Among different restorative solutions, implants have been successfully used to support single-tooth restorations (crowns), fixed partial dentures (bridgeworks), full arch fixed or removable dentures and restore function and aesthetics in fully and partially edentulous patients [9–12]. Worldwide statistics show that a high success rate of dental implants (over 95 %) occurs if implants are properly designed and manufactured [13], and if they are inserted in a bone segment characterized by good quality and quantity [14, 15]. Nevertheless, success of the prosthetic treatment is widely affected by a number of factors that can change the biomechanical coupling between implant and bone, such as implant location, mechanical and morphological properties of bone, mechanical and geometrical features of implant as well as the prosthesis, and type and magnitude of the load transferred by the implant to the bone, as well as by host factors such as smoking and bacterial environment [16–20]. Regardless of the high success rate of such dental implants, the literature reveals a significant incidence of technical complications, mainly related to unfavorable loading or to high stress concentrations [21, 22].
Common technical failures include abutment and prosthetic screw loosening and fracturing [23], micro displacement of the prosthesis [24, 25] and of the abutment-implant connection, [23–26]. Although these failures usually do not lead to the loss of an implant, they do represent a significant issue for both patients and clinicians and result in additional costs. To mitigate these difficulties, implants and abutments have undergone a number of modifications, and an extensive variety of implant and abutment geometries and connections are available today. The design of an implant system, as characterized by its geometry and type of implant-abutment connection, is an important factor in establishing the performance and maintenance of implant osseo-integration and implant-supported prostheses since design determines load transmission at both the bone-to-implant and implant-to- abutment interfaces [27].
Therefore, the reliability of the implant-prosthesis connection as well as the integrity and the stability of the different structures involved are crucial prerequisites for long-term success in implant rehabilitation. The coupling and the stability between implants and prosthetic structures is usually ensured by connection screws, which are tightened by using torque wrenches.
However, instability at the implant-abutment interface, whether caused by inadequate screw preload, poor accuracy of thread coupling, or very large manufacturing tolerances, can easily lead to prosthetic complications [28–32].
A poor fit as well as mobility between structures introduces harmful tensile, compressive and bending forces, which may be dangerous for the osseointegration process, leading to possible physiologically inadmissible strains that activate bone resorption [33, 34] and/or leading to failure of the components (connection screws, prosthetic framework and veneering material).
When a screw loosening occurs, the clinician should early detect the loose screws and torque them again.
However, the initial screw loosening and the following micro- displacement of the restoration are not perceived by the patient immediately.
This results in:
-
a gap between fixture and prosthesis, which is a favorable environment for bacteria colonization, leading to infection of the peri-implant tissues and bone resorption,
-
the further loosening of the screws, with greater displacement of the prosthesis,
-
the potential breaking of the prosthesis due to misfit between implant platforms and prosthesis,
-
the transmission of the masticatory forces to the screws that will work alone as the real connection between implants and prosthesis, until their fracture, which usually involves the screw under-head.
If a failure of the prosthesis exclusively occurs, depending on the degree of the damage, the clinician may decide to repair the prosthesis or to fabricate a new one.
Instead the removal of a fractured screw from the implant body is not easy and is not always possible, depending on the length of the fractured part. When a screw cannot be removed, new surgical steps (removal of the osseointegrated implant and insertion of a new implant), and/or prosthodontic procedures (fabrication of a new prosthesis) are required, with a consequent increase of treatment time and costs for both patients and clinical-laboratory team.
Therefore, it would be extremely important to be able to record any micro-displacement at least daily and inform the clinician about it. This would require the possibility to wireless transmitting the data recorded by a sensor. The sensor and all the circuits needed for the collection, storing and transmission of data, can be put inside the prostheses (i.e. sensor-supported prosthesis). Therefore, the wireless device should be able to transmit from inside the prostheses (which is made of isolant material) to a device outside the mouth. The transmission can be done once/twice a day so it does not have to transmit continuously but must store some data and then it can transmit it to a device that can be put also close to the mouth (few centimeters). Finally, it should be possible to transmit these data to the dentist as the system is conceived for an early warning on the prosthesis performance and a partial remote management of the related actions from the dentist. Moreover, we aim to carry on an epidemiological and clinical study aimed to pinpoint any metabolic alterations that may occur upon sensor-supported prosthesis delivery. It has to be considered that the overall implanted is expected to be long- term working inside the mouth of the patient: hence, a physio- pathological adaptation of the oral mucosae to the presence of a foreign device as well as a modification of residing microbiota can not be aprioristically ruled out. Therefore, we plan to set up different methodological approaches to address these clinical tasks which will be presented in Sect. 4.
3 The Wireless Communication Sub-system
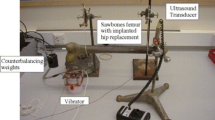
Wireless communication between intraoral devices and the outside world is challenging. As a matter of fact, the oral cavity is a hybrid propagation environment. It is not strictly speaking a communication “inside the body” as a sensor inside the body, depending on its anatomical location, is usually surrounded by a distinct and fairly stable tissue environment. An intraoral device is located in a constantly changing environment depending on the relative positions of the jaws and movements of the tongue, which continuously changes shape when one swallows, breathes, or speaks. On the other, it makes sense to use RF communications as for over-the-air communications as in any case sensors would be very closely located to the “outside part of the body”. Therefore, it could be possible to use all the considerable research conducted on wireless communication inside and around the human body. As intraoral devices are in contact with the gums, the tongue, or the palate, and their associated receivers may be in contact with the human body, Body Channel Communication (BCC) can be considered to be used for these devices [35]. However, when applied to intraoral devices, neither of the BCC methods maintains their desired operating conditions. Therefore, the use of RF-based wireless communications can be considered. As a matter of fact, RF wireless communication has been successfully adopted in implantable devices such as the pacemaker and neurostimulator. However, not much work has been done for the specific case of the intraoral devices. One issue that arises in many possible intraoral sensing applications is where to place the antennas/transceiver and battery and the related problem of miniaturizing those components. In this specific application, this requirement is less stringent as we can place everything inside the prostheses (there is roughly a room of 10 mm to be used). However, this poses challenges to the choice of the communication technology as in this case the wireless transmitter is “inside” the tooth/prosthesis. Therefore, for the considered system, also considering the details study on the use of frequency in [36], a suitable frequency band is 433.9 MHz. Therefore, the transmitter will not transmit directly to a smartphone or tablet (to do so, we should have used the 2.4 GHz and the standard Bluetooth), but we have to foresee another external device specifically designed for collecting the recorded data during 1 day and able to transmit these data via internet connection to the dentist.
However, one of the main challenges limiting the adoption of RF-based intraoral devices is the need to have a battery inside the mouth. Some interesting recently proposed solutions are energy-harvesting systems based on the use of the jaw movement that normally occurs when chewing, eating and speaking [29]. For instance, one can obtain approximately 580 J only from daily chewing, which is equivalent to an average power of approximately 7 mW [37]. However, the challenge related to the battery is not only related to the size or the way to recharge it but also to safety issues. The battery and the TX part must be “anchored” in some way to avoid that they are swallowed. In our case, this would not be a problem as also the battery should be put and anchored inside the prostheses. On the other hand, the disposal of the battery, after sometime, might require another dental operation and this is not desirable. Therefore, a valuable alternative is provided by using a passive approach: the room inside the prosthesis is used for placing the sensor and a small memory which records the data, integrated with an RFID chip. Once a day or more often an external reader device is placed close to the mouth to collect the data. The application of this passive approach for intraoral sensing has been already proposed and successfully implemented [38, 39], in cases where the sensors is located just in the mouth and outside the tooth. However, the use of RFID passive tags to be put inside the tooth has been proposed and experimentals on animals have been performed [40] for identification purposes. Recently, the use of RFID tags also for an intraoral continuous monitoring applications, such as saliva analysis to detect the risk of hearth attack, has been proposed [41] even if not implemented yet. In [41] the RFID reader is implemented as wristband with built in microprocessor. The wristband is used to make the alarm signal in case of a close heart attack. In our case, where no continuous monitoring is needed, we are going to evaluate the possibility to use the NFC technology, already available in many smartphones and develop an application to deliver the data to the dentist smartphone. While NFC sensor-based devices are penetrating the healthcare market, the application to out system is not straightforward. Even if low distance might be involved between the tag and the reader, we are in presence of non-LOS propagation conditions.
4 Epidemiological and Clinical Study
The effect of radiofrequencies exposure on human tissues is a subject of extensive debate in the scientific community and the published studies do not allow to draw unambiguous conclusions yet [41–43].
Even though there is a substantial convergence in ruling out that the exposure to radiofrequencies induces a DNA damage, and thus a genotoxic effect, it does not turn out clear whether their energy cleaves weak chemical bonds interactions and/or they alter the physico-chemical properties of the micro-environment surrounding the cells. With respect to this last point, even small but persisting alteration of the temperature of a biological fluid could hide a more relevant metabolic effect [44].
Moreover, it has to be mentioned that, in most cases, the studies published to date refer to a limited temporal exposure of cells and tissues to radiofrequencies, while the aim of the present project is to realize long-term residing implants that might produce metabolic effects over a prolonged incubation time.
Then, a qualitative and quantitative determination of recognized macromolecules driving flogistic events in human tissues will be carried out at different time points: the expression and secretion of proteolytic enzymes (i.e. Matrix Metalloproteinases MMPs) dealing with human mucosae extracellular matrix (ECM) remodeling and degradation, and the release of the most representative ECM molecules will be examined [45–47]. These macromolecules are commonly observed in biological fluids, like as saliva, and the analysis of their distribution provides a reliable marker of mucosae homeostasis.
In addition, a quantitative and qualitative analysis of soluble mediators of inflammation, like as cytokines, in the saliva will be performed [48]. As previously described for MMPs and ECM macromolecules, such an approach provides a relevant indication of the tissutal dys-homeostasis eventually occurring over time. The overall cytokines panel will further furnish detail on the contribution of the immune system to the adaptative response of the oral mucosae to the device implantation, thus possibly addressing also the eventual therapeutic approach to the problem.
In conclusion, a long-term analysis of the resident microbiota is of the utmost importance. Microbiological cultures will be set up to both identify any alteration in the overall composition of the microbiota and to specifically cast light on some bacteria that might well adhere to the device, colonizing it and leading to major insult to the local mucosae.
Notably, for all experimental procedures above indicated, the biological samples will be harvested both before sensor- supported prosthesis delivery and at specific time-points after the installation in order to get a deeper insight on the link between the device and the putative metabolic alteration onset. Any significant alteration in metabolic profile composition will be then tightly examined and deepened through the appropriate techniques.
5 Conclusions
The paper proposes a system for an early warning on the prosthesis performance, in particular in terms of micro- displacements of the implant-prostheses connection, enabling actions to prevent fatal damages to the structure. The system includes a sensor for micro-displacement to be inserted in the prosthesis volume, with embedded wireless communications capabilities. Two main approaches for the wireless communication device has been discussed, i.e. an active and a passive approach. Initial considerations lead to prefer a passive approach. However, experimental studies need to be performed to better identify the final optimal solution and solve issues related to battery, safety, transmission power levels. The successful implementation of such a system would contribute to the quality of life of patients and the cost reduction of the treatment.
References
Hori, K., Ono, T., Tamine, K., Kondo, J., Hamanaka, S., Maeda, Y., et al. (2009). Newly developed sensor sheet for measuring tongue pressure during swallowing. Journal of Prosthodontic Research, 53, 28–32.
Nishigawa, K., Bando, E., & Nakano, M. (2001). Quantitative study of bite force during sleep associated bruxism. Journal of Oral Rehabilitation, 28, 485–491.
Peng, Q., & Budinger, T. F. (2007) ZigBee-based wireless intra-oral control system for quadriplegic patients. In IEEE transactions on engineering in medicine and biology society (pp. 1647–1650).
Sardini, E., Serpelloni, M., & Fiorentini, R. (2013). Wireless intraoral sensor for the physiological monitoring of tongue pressure. In IEEE transactions on solid-state sensors, actuators and microsystems (pp. 1282–1285).
Park, H., Kim, J., & Ghovanloo, M. (2012). Development and preliminary evaluation of an intraoral tongue drive system. In IEEE transactions on engineering in medicine and biology society (pp. 1157–1160).
Park, H., Kiani, M., Lee, H., Kim, J., Block, J., Gosselin, B., & Ghovanloo, M. (2012). A wireless magnetoresistive sensing system for an intraoral tongue-computer interface. In IEEE transactions on biomedical circuits and systems (pp. 571–585).
Kim, J. H., Jung, J. H., Jeon, A. Y., Yoon, S. H., Son, J. M., Ye, S. Y., & Jeon, G. R. (2007). System development of indwelling wireless pH Telemetry of intraoral acidity. In IEEE transactions on information technology applications in biomedicine (pp. 302–305).
Branemark, P. I., Hansson, B. O., Adell, R., et al. (1977). Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scandinavian Journal of Plastic and Reconstructive Surgery, 16, 1–132.
Taylor, T. D., Belser, U. C., & Mericske-Stern, R. (2000). Prosthodontic considerations. Clinical Oral Implants Research, 11, 101–107.
Baggi, L., Di Girolamo, M., Vairo, G., & Sannino, G. (2013). Comparative evaluation of osseointegrated dental implants based on platform- switching concept: influence of diameter, length, thread shape, and in- bone positioning depth on stress-based performance. Computational and Mathematical Methods in Medicine, 2013, 250929.
Roos-Jansaker, A. M., Lindahl, C., Renvert, H., & Renvert, S. (2006). Nine-to fourteen-year follow-up of implant treatment. Part I: Implant loss and associations to various factors. Journal of Clinical Periodontology, 33, 283–289.
Sannino, G., Pozzi, A., Schiavetti, R., & Barlattani, A. (2012). Stress distribution on a three-unit implant-supported zirconia framework. A 3D finite element analysis and fatigue test. Oral and Implantology (Rome), 5, 11–20.
Sannino, G., & Barlattani, A. (2013). Mechanical evaluation of an implant- abutment self-locking taper connection: finite element analysis and experimental tests. International Journal of Oral and Maxillofacial Implants, 28, 17–26.
Eckert, S. E., & Wollan, P. C. (1998). Retrospective review of 1170 endosseous implants placed in partially edentulous jaws. Journal of Prosthetic Dentistry, 79, 415–421.
Weyant, R. J. (2003). Short-termclinical success of root-form titanium implant systems. Journal of Evidence Based Dental Practice, 3, 127–130.
Brunski, J. B. (1997). Biomechanics of dental implants. In M. Block, J. N. Kent, & L. R. Guerra (Eds.), Implants in dentistry (pp. 63–71). Philadelphia, PA: W.B. Saunders.
Pozzi, A., Sannino, G., & Barlattani, A. (2012). Minimally invasive treatment of the atrophic posterior maxilla: a proof-of-concept prospective study with a follow-up of between 36 and 54 months. Journal of Prosthetic Dentistry, 108, 286–297.
Brunski, J. B., Puleo, D. A., & Nanci, A. (2000). Biomaterials and biomechanics of oral and maxillofacial implants: current status and future developments. International Journal of Oral and Maxillofacial Implants, 15, 15–46.
Sannino, G. (2015). All-on-4 concept: A 3-dimensional finite element analysis. Journal of Oral Implantology, 41, 163–171.
Lemons, J. E. (2004). Biomaterials, biomechanics, tissue healing, and immediate-function dental implants. Journal of Oral Implantology, 30, 318–324.
Sahin, S., Cehreli, M. C., & Yalcin, E. (2002). The influence of functional forces on the biomechanics of implant-supported prostheses: A review. Journal of Dentistry, 30, 271–282.
Cehreli, M. C., Sahin, S., & Akca, K. (2004). Role of mechanical environment and implant design on bone tissue differentiation: Current knowledge and future contexts. Journal of Dentistry, 32, 123–132.
Jemt, T. (1992). Failures and complications in 391 consecutively inserted fixed prostheses supported by Branemark implants in edentulous jaws: a study of treatment from the time of prosthesis placement to the first annual checkup. International Journal of Oral and Maxillofacial Implants, 6, 270–276.
Naert, I., Quirynen, M., van Steenberghe, D., et al. (1992). A study of 589 consecutive implants supporting complete fixed prostheses. Part II: Prosthetic aspects. Journal of Prosthetic Dentistry, 68, 949–956.
Geramy, A., & Morgano, S. M. (2004). Finite element analysis of three designs of an implant-supported molar crown. Journal of Prosthetic Dentistry, 92, 434–440.
Becker, W., & Becker, B. E. (1995). Replacement of maxillary and mandibular molars with single endosseous implant restorations: a retrospective study. Journal of Prosthetic Dentistry, 74, 51–55.
Bozkaya, D., Muftu, S., & Muftu, A. (2004). Evaluation of load transfercharacteristics of five different implants in compact bone atdifferent load levels by finite elements analysis. Journal of Prosthetic Dentistry, 92, 523–550.
Schwarz, M. S. (2000). Mechanical complications of dental implants. Clinical Oral Implants Research, 11, 156–158.
Jung, R. E., Pjetursson, B. E., Glauser, R., Zembic, A., Zwahlen, H., & Lang, N. P. (2008). A systematic review of the 5-year survival and complication rates of implant supported single crowns. Clinical Oral Implants Research, 19, 119–130.
Wannfors, K., & Smedberg, J. L. (1999). A prospective clinical evaluation of different single-tooth restoration designs on osseointegrated implants. Clinical Oral Implants Research, 10, 453–458.
Ekfeldt, A., Carlsson, G. E., & Borjesson, G. (1994). Clinical evaluations of singletooth restorations supported by osseointegrated implants: A retrospective study. International Journal of Oral and Maxillofacial Implants, 9, 179–183.
Al Jabbari, J., Fournelle, R., Ziebert, G., Toth, J., & Iacopino, A. M. (2008). Mechanical behaviour and failure analysis of prosthetic retaining screws after long term use in vivo. Part 1: Characterization of adhesive wear and structure of retaining screws. Journal Prosthodontics, 17, 168–180.
Cowin, S. C. (2001). Bone mechanics handbook. Boca Raton, FL: CRC Press.
Martin, R. B., Burr, D. B., & Sharkey, N. A. (1998). Skeletal tissue mechanics. New York, NY: Springer.
Cho, N., Yoo, J., Song, S., Lee, J., Jeon, S., & Yoo, H. (2007). The human body characteristics as a signal transmission medium for intrabody communication. In IEEE transactions on microwave theory and techniques (pp. 1080–1086).
Park, H., & Ghovanloo, M. (2014). Wireless Communication of Intraoral Devices and Its Optimal Frequency Selection. In IEEE transactions on microwave theory and techniques (pp. 3205–3215).
Delnavaz, A., & Voix, J. (2014). Flexible piezoelectric energy harvesting from jaw movements. Smart Materials and Structures, 23, 1–8.
Mannoor, M. S., Tao, H., Clayton, J. D., Sengupta, A., Kaplan, D. L., Naik, R. R., et al. (2012). Graphene-based wireless bacteria detection on tooth enamel. Nature Communications, 27, 763.
Diaz Lantada, A., González, B. C., Lafont Morgado, P., & Sanz Maudes, J. (2012). Novel system for bite-force sensing and monitoring based on magnetic near field communication. Sensors, 12, 11544–11558.
Ishihata, H., Tomoe, T., Takei, K., Hirano, T., & Yoshida, K. (2007). A radio frequency identification implanted in a tooth can communicate with the outside world. IEEE Transactions on Information Technology in Biomedicine, 11(6), 683–685.
Igor, Z., Dmitry, M., & Andrey, S. (2012). Nano sensors integrated into dental implants for detection of acute myocardial infarction. International Journal of Emerging Trends and Technology in Computer Science (IJETTCS), 1(2), 85–87.
Miyakoshi, J., Takemasa, K., Takashima, Y., Ding, G. R., Hirose, H., & Koyama, S. (2005). Effects of exposure to a 1950 MHz radio frequency field on expression of Hsp70 and Hsp27 in human glioma cells. Bioelectromagnetics, 26, 251–257.
Nora Volkow, D., Tomasi, D., Wang, G. J., Vaska, P., Fowler, J. S., Telang, F., et al. (2011). Effects of cell phone radiofrequency signal exposure on brain glucose metabolism. JAMA., 305, 828–829.
Habauzit, D., Le Quément, C., Zhadobov, M., Martin, C., Aubry, M., Sauleau, R., & Le Dréan, Y. (2014). Transcriptome analysis reveals the contribution of thermal and the specific effects in cellular response to millimeter wave exposure. PLoS ONE, 9, e109435.
Sbardella, D., Fasciglione, G. F., Gioia, M., Ciaccio, C., Tundo, G. R., Marini, S., & Coletta, M. (2012). Human matrix metalloproteinases: an ubiquitarian class of enzymes involved in several pathological processes. Molecular Aspects of Medicine, 33, 119–208.
Sbardella, D., Tundo, G. R., Fasciglione, G. F., Gioia, M., Bisicchia, S., Gasbarra, E., et al. (2014). Role of metalloproteinases in tendon pathophysiology. Mini Reviews in Medicinal Chemistry, 14, 978–987.
Gursoy, U. K., Kononen, E., Pradhan-Palikhe, P., Tervahartiala, T., Pussinen, P. J., Suominen-Taipale, L., & Sorsa, T. (2010). Salivary MMP-8, TIMP-1 and ICTP as markers of advanced periodontitis. Journal of Clinical Periodontology, 37, 487–493.
Willimason, S., Munro, C., Pickler, R., Grap, M. J., & Elswick, R. K. (2012). Comparison of biomarkers in blood and saliva of healthy adults. Nursing Research and Practice, 2012, 1–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
The whole study will be performer upon approval by the local ethic committee.
Rights and permissions
About this article
Cite this article
Sannino, G., Sbardella, D., Cianca, E. et al. Dental and Biological Aspects for the Design of an Integrated Wireless Warning System for Implant Supported Prostheses: A Possible Approach. Wireless Pers Commun 88, 85–96 (2016). https://doi.org/10.1007/s11277-016-3244-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11277-016-3244-6