Abstract
The resistance of Candida albicans to azole drugs represents a great global challenge. This study investigates the potential fungicidal effects of atorvastatin (ATO) combinations with fluconazole (FLU), itraconazole (ITR), ketoconazole (KET) and voriconazole (VOR) against thirty-four multidrug-resistant (MDR) C. albicans using checkerboard and time-kill methods. Results showed that 94.12% of these isolates were MDR to ≥ two azole drugs, whereas 5.88% of them were susceptible to azole drugs. The tested isolates exhibited high resistance rates to FLU (58.82%), ITR (52.94%), VOR (47.06%) and KET (35.29%), whereas only three representative (8.82%) isolates were resistant to all tested azoles. Remarkably, the inhibition zones of these isolates were increased at least twofold with the presence of ATO, which interacted in a synergistic (FIC index ≤ 0.5) manner with tested azoles. In silico docking study of ATO and the four azole drugs were performed against the Lanosterol 14-alpha demethylase enzyme (ERG11) of C. albicans. Results showed that the mechanism of action of ATO against C. albicans is similar to that of azole compounds, with a docking score (−4.901) lower than azole drugs (≥5.0) due to the formation a single H-bond with Asp 225 and a pi–pi interaction with Thr 229. Importantly, ATO combinations with ITR, VOR and KET achieved fungicidal effects (≥ 3 Log10 cfu/ml reduction) against the representative isolates, whereas a fungistatic effect (≤ 3 Log10 cfu/ml reduction) was observed with FLU combination. Thus, the combination of ATO with azole drugs could be promising options for treating C. albicans infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fungal diseases kill more than 1.5 million per year and affect over a billion people. However, they are still a neglected topic by public health authorities even though most deaths from fungal diseases are avoidable (Bongomin et al. 2017). Candida genus is one the most important opportunistic fungi responsible for high morbidity and mortality worldwide, especially with immunocompromised hosts. The members of this genus can cause vaginitis, oral candidiasis, cutaneous candidiasis, candidemia, and systemic infection (Matthaiou et al. 2015; Pappas et al. 2015, 2018; Gintjee et al. 2020; Wall and Lopez-Ribot 2020). Approximately, 80% of Candida infections are caused by C. albicans, although there is a progressive shift to Candida non-albicans infections especially C. glabrata, C. tropicalis, C. krusei and C. dubliniensis (Friedman and Schwartz 2019).
Four main antifungal classes are used in the treatment of candidiasis; azoles, polyenes, fluoropyrimidines, and echinocandins (Santos et al. 2018). However, the limited number of antifungal drugs represents a leading cause of morbidity and mortality of fungal infections worldwide. Furthermore, the toxicity of current antifungal drugs and the increasing incidence of Candida infections, associated with the emergence of pathogens that are highly resistant to most antifungal agents, as well as the emergence of drug-resistance by non-albicans strains of Candida, have demanded steady research and development of new antifungal drugs that exert their effects by alternative mechanisms of action and combined with low toxicity (Perlin et al. 2017; Santos et al. 2018; Pristov and Ghannoum 2019; Gintjee et al. 2020). Despite the necessity of the discovery of novel antifungals, the financial resources for this field of research are still restricted and the approval process is already long and expensive (Sanglard 2016; Campoy and Adrio 2017; Wall and Lopez-Ribot 2020). Repurposing of existing drugs represents a promising strategy in developing drug molecules with new therapeutic indications (Wall and Lopez-Ribot 2020; Juárez-López and Schcolnik-Cabrera 2021). Based on this perspective, statin drugs are widely used to reduce cardiovascular event risk by inhibiting the synthesis of cholesterol in the liver. These drugs have exhibited other pleiotropic effects; antioxidant, anticoagulant (Vadivoo et al. 2018), anticancer (Gupta et al. 2019; Di Bello et al. 2020); anti-inflammatory (Koushki et al. 2021) and antibacterial activities (Ko et al. 2017; Vadivoo et al. 2018, however the antifungal activities of these drugs remain poorly studied. Interestingly, atorvastatin is one of statin drugs has shown significant antifungal activity against different Candida species. particularly against C. albicans (Esfahani et al. 2019; Lima et al. 2019). Our study aimed to explore the potential antifungal activity of ATO against multidrug resistant isolates of C. albicans, as well as to evaluate its synergistic potential with some azole drugs against these isolates.
Materials and methods
Candida albicans isolates
Thirty-four C. albicans isolates were obtained from the clinical laboratory at Kasr El-Ainy Hospital, Cairo, Egypt, during the period from 2019 to 2020. These isolates were previously isolated from different clinical specimens (urine, sputum, pus, wound and blood). The isolates were purified by streaking on sterile Chromagar Candida plates (Difco) and incubated at 37 ± 2 °C for 48 h. The metallic green colonies (De Angelis et al. 2020) were picked up and sub-cultured again in Sabouraud dextrose broth medium (SDB, Oxoid) and incubated at 37 ± 2 °C for 24 h and then diluted 1:1 with sterile 50% glycerol and stored at −20 °C until use.
Antifungal susceptibility testing
The susceptibility of thirty-four C. albicans isolates to five different antifungal agents were studied by determination of the minimum inhibitory concentration (MIC) using microdilution method according to the clinical and laboratory standards institute (CLSI) guideline (CLSI 2017). Briefly, the stock solutions of amphotericin B, (AMP, Bristol Myers Squibb Woerden, The Netherlands), fluconazole (FLU, Novartis, Egypt), itraconazole (ITR, Apex pharma, Egypt), ketoconazole (KET, Ramedia, Egypt) and voriconazole (VOR, Pfizer, Egypt) powders were separately prepared to the concentrations 16 mg/l, 128 mg/l, 25.6 mg/l, 16 mg/l and 25.6 mg/l, respectively in 1% dimethyl formamide (Sigma). Following the two-fold serial dilution of each stock solution with sterile SDB in a 96-well microtiter plate. The suspension of each tested isolates was separately prepared in SDB. Aliquots (100 μL) of each isolate suspension was separately added to each antifungal diluent. The final inoculum size of each examined isolate was approximately 1 × 105 cfu/ml. Wells containing 200 μl of un-inoculated and inoculated SDB were considered as negative and positive controls. All experiments were conducted in triplicate. The plates were incubated overnight at 37 ± 2 °C and then the MIC of each tested solution was visually determined. The MIC was considered the lowest concentration of the examined drug capable of inhibiting of the fungal growth (Espinel-Ingroff et al. 2016). Additionally, MIC of atorvastatin calcium trihydrate (ATO, EIPICO, Egypt) was determined by the same above-mentioned method against the representative (the most antifungal resistant) C. albicans isolate at concertation 256 mg/l.
The interaction between ATO and the five different antifungal agents against the representative isolates was initially investigated by the disc diffusion method using Mueller–Hinton agar containing 200 mg/l glucose and 0.005 mg/I methylene blue dye (MHG) (CLSI 2017). The overnight culture of each tested isolates on Sabouraud dextrose agar medium (SDA, Oxoid) was adjusted to a turbidity equivalent to a 0.5 McFarland standard at 520 nm (approximately 1 × 105 cfu/ml). A sterile cotton swab was dipped into each isolate suspension and spread on the surface of sterile MHG plates containing 0.0 (control), 0.5 and 1.0 mg/l ATO. Following the inoculation, the plates allowed to dry before placing the discs [AMP (100 μg), FLO (25 μg), ITA (8 μg), KET (15 μg), and VOR (1 μg)]. Additionally, discs containing 100 µg ATO were made in-house as a part of this study. These discs were placed on control MHG plates. All the plates were incubated for 24 h at 37 ± 2 °C. Following the incubation, the diameter (mm) of inhibition zone around each disc was measured.
Docking study
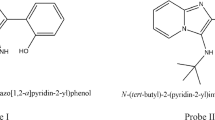
Ligand preparation
ATO, FLU, ITR, KET, and VOR chemical structures were retrieved from the PubChem database (https://pubchem.ncbi.nlm.nih.gov) (Fig. 1). LigPrep 2.4 software was used for ligand energy minimization and preparation. The energy minimization of compounds was carried out using the Macromodel minimization tool of the Maestro Version 12.8.117 Schrodinger software.
Protein preparation
The Protein Data Bank (PDB) database (https://www.rcsb.org/) was used to obtain the complete structure of the Lanosterol 14-alpha demethylase enzyme (ERG11) of Candida albicans based on accession number PDB: 5V5Z Fig. 2 (Keniya et al. 2018).
Homology Model 3D Structure Build
Homology modeling of HMG-CoA reductase sequences was carried out. The Swiss-modeling server (https://swissmodel.expasy.org/) was used to predict the homology 3D structure of HMG-CoA reductase based on target protein sequence alignment using ProMod3 and QMEAN scoring function (Guex et al. 2009; Benkert et al. 2011; Remmert et al. 2012; Bertoni et al. 2017; Waterhouse et al. 2018). The three-dimensional quaternary structure of the templates was used to build models of target proteins with the accession number (pdb: 3cd0) (Sarver et al. 2008).
In silico Molecular modelling
In silico docking was used to determine the inhibitory mode of action of the studied ligands. Maestro 12.8 software was used to conduct inhibitory binding mode of action studies on ligands. The ligands were docked using the Schrodinger Maestro 11.9 software and Glide's standard Precision (SP) (Friesner et al. 2006). The grid box size was set to 20 Å by default for each protein.
Homology model analysis
An analysis of homology models for reductase of HMG-CoA revealed 59.16% identity for coenzyme A reductase (HMG-CoA reductase) of 3-hydroxy-3-methylglutaryl (pdb: 3cd0) (Sarver et al. 2008). The three-dimensional structure of HMG-CoA reductase was depicted in Fig. 3.
In vitro synergy assay
The fractional inhibitory concentration (FIC) of ATO combinations with FLU, ITR, KET and VOR against the representative isolates was evaluated by checkerboard microdilution method (Lima et al. 2018). Briefly, two-fold serial dilutions of ATO (50 μl) and the tested antifungal agent (50 μl) were dispensed in horizontal and vertical orientations, respectively. Next, aliquot (100 μL) of each isolate suspension was separately added to each diluent. The final concentrations of ATO and tested antifungal agents were ranged from 2 × MIC to 1/16 MIC, whereas the final inoculum size of each isolate was approximately 1 × 105 cfu/ml. Tests were conducted in triplicate. The plates were incubated overnight at 37 ± 2 °C and then the FIC index of each combination was calculated as follows: FIC index = FIC ATO + FIC azole drug, where the FIC value is calculated as follows: MIC of drug in combination/ MIC of drug alone. The interpretation of FIC index was defined as synergism (FIC index ≤ 0.5), indifference (0.5 > FIC index < 4), and antagonism (FIC index > 4) (Lee et al. 2012). Based on the FIC index, the synergistic ATO combinations were selected in the subsequent studies.
Time-Kill kinetic Assay
Time-kill experiments were conducted with sterile 50 ml SDB in 200 ml bottles. Time-kill assay of ATO combinations with different antifungal agents against the representative isolates was performed as follows; the suspension of each examined isolate was separately prepared and adjusted to approximately a 0.5 McFarland standard (approximately 1 × 105 cfu/ml) in sterile SDB containing single (ATO, FLU, ITR, KET or VOR) and combination (ATO/FLU, ATO/ITR, ATO/KET or ATO/VOR) drugs, whereas inoculated sterile SDB was used as control. Test and control treatments were incubated overnight at 37 ± 2 °C on rotary shaker (150 rpm). Aliquots of 20 µl were removed at 0 and 24 h, serially diluted ten-fold with sterile distilled water, plated on SDA plates and incubated 48 h at 37 ± 2 °C for colony count determination. Tests were conducted in triplicate and the combined data were presented as mean of bacterial counts (Log10 cfu/ml) at each time point. For judgment of the interaction between ATO and the tested antifungal agents, synergism was defined as a ≥ 2 Log10 decrease in cfu/ml and indifference as a < 2 Log10 decrease in cfu/ml compared to the most active drug, and antagonism as a ≥ 2 Log10 increase in CFU/ml compared to the least active drug (Li et al. 2014). The time-kill curve of control and each treatment was constructed by plotting the cfu/ml surviving at each time point. Fungistatic and fungicidal effects were defined as <3 Log10 and ≥3 Log10 reductions in cfu/ml from the starting inoculum, respectively (Scorneaux et al. 2017).
Results
The susceptibility of thirty-four C. albicans isolates to five different antifungal agents was evaluated through the determination of the MIC using the broth microdilution method. As shown in Table 1, out of the thirty-four isolates, 20 (58.82%) isolates were resistant to FLU, 18 (52.94%) isolates were resistant to ABP and ITR, 16 (47.06%) isolates were resistant to VOR, and 12 (35.29%) isolates were resistant to KET. Notably, the sensitivity to all used antifungal agents was only observed with 2 (5.88%) isolates, whereas the resistance was only observed with 3 (8.82%) isolates. These isolates were selected as representative isolates for the subsequent studies.
The susceptibility results of the representative isolates (CA1, CA2 and CA3) to FLU, ITR, VOR, KET, AMB and ATO are summarized in Table 2. The results showed that FLU and KET exhibited the highest antifungal activities against the examined isolates, with inhibition zones ranging from 30 mm to 40 mm, followed by VOR and ITR, with inhibition zones ranges (30–35 mm) and (17–20 mm), respectively. Whereas AMB and ATO exhibited the lowest antifungal activities against the examined isolates, with inhibition zones ranges (13–17 mm) and (13–20 mm), respectively. It worth noting that adding 0.5 mg/l ATO to HMG was significantly increased the inhibition zones of the first four antifungal agents to the ranges (53–55 mm), (57–60 mm), (57–60 mm) and (28–30 mm), respectively. Moreover, adding 1.0 mg/l ATO to HMG was significantly increased the inhibition zones of the first three antifungal agents to the range (60–65 mm). whereas the antifungal activities of ITR against the three isolates were slightly increased, with inhibition zones ranging from 23 mm to 35 mm. Conversely, adding 1.0 mg/l ATO to HMG was decreased the inhibition zones of AMP against the three isolates from the range (13–17 mm) to (10–14 mm). Thus, this antifungal agent was excluded in the subsequent studies (Fig. 4). The highest MIC values of the tested drugs were observed with ATO followed by FLU, AMP, KET, VOR and ITR, with MIC ranges (16–32 mg/l), (8.0–16 mg/l), (3.2–12.8 mg/l), (2.0–4.0 mg/l), (2.0–4.0 mg/l) and (1.6–3.2 mg/l), respectively (Table 2).
The antifungal activity of four different antifungal agents against representative Candida albicans isolates in the presence and absence of atorvastatin. ATO Atorvastatin, AMP Amphotericin B, FLU Fluconazole, ITR Itraconazole, VOR Voriconazole, KET Ketoconazole, A: Control medium (ATO- free), B: Medium containing 0.5 mg/l ATO, C: Medium containing 1.0 mg/l ATO
An in-silico approach is a complementary strategy to the animal studies used to elucidate molecular mechanisms. While the ERG11 gene in C. albicans encodes lanosterol demethylase, which is the target of azole antifungals, ATO is a synthetic lipid-lowering agent. ATO inhibits hydroxymethyl-glutaryl coenzyme A (HMG-CoA) reductase in a competitive manner (Table 3).
The docking results of the investigated ligands against ERG11 and HMG-CoA) reductase and the H-bond distances in angstrom (A) with the interreacting amino-acid residue(s) are shown in Fig. 5 and 6 and Table 3. ATO's binding affinity for HMG-CoA reductase was high (−5.472 kcal/mol) due to the formation of two H-bonds with Gly (C) 715 (1.84 A) and Ser (c) 720 (1.83 A). KET, VOR, and ITR all had a high binding score of −5.375, −5.325, and −5.256, respectively, with the formation of two hydrogen bonds with Ser (D) 841 (2.14 A) and Asn (D) 813 (2.30 A) in KET, one hydrogen bond with Glu (C) 714 (1.73) in VOR, and one hydrogen bond with Asn (D) 813 (2.33 A) in ITR. FLU, on the other hand, had a lower binding score of −4.794 and formed one H-bond with Glu (C) 714 (1.68 A). (Table 3 and Fig. 5).
Additionally, KET and FLU inhibited the active site in their interactions with ERG11, with docking scores of −6.642 and −6.452, respectively. KET formed three H-bonds with Gln 66 (1.99 A), His 373 (2.44 A), and Ser 378 (1.96 A), whereas FLU formed two H-bonds with Met 508 (2.43 A), and Asp 225 (2.00 A). However, VOR and ITR had docking scores of −5.507 and −5.308, respectively, due to the formation of one H-bond with Asp 225 (1.65 A) in the case of VOR and Two H-bonds with Gln 309 (2 H-bonds) with distance of 2.60 A and 2.77 A in the case of ITR, as well as a pi–pi interaction with His 310 and pi interaction Lys 226. ATO, on the other hand, had a docking score of −4.901 due to the formation of a single H-bond with Asp 225 (1.77 A) and a pi–pi interaction with His 310. (Table 3 and Fig. 6).
The checkerboard results of ATO combinations with FLU, ITR, VOR or KET against the representative isolates are summarized in Table 4. The results demonstrated that all the ATO combinations were able to interact synergistically (FIC index ≤ 0.5) against the tested isolates, with a four-fold reduction in the MICs of these drugs. It worth noting that the MIC values of azole drugs in these combinations were significantly decreased lower than the susceptible breakpoints. In these combinations, MICs of ATO, FLU, ITR, VOR and KET were significantly decreased from the ranges (16–32 mg/l), (8.0–16 mg/l), (1.6–3.2 mg/l), (2.0–4.0 mg/l) and (1.6–12.8 mg/l) to 4.0 mg/l, (1.0–4.0 mg/l), (0.2–0.4 mg/l), (0.25–0.5 mg/l) and (0.4–1.6 mg/l), respectively.
Time-kill results of FLU, ITR, VOR or KET and their respective combinations with ATO against the representative isolates (CA1, CA2 and CA3) are summarized in Table 5. The results demonstrated that none of the examined drugs in monotherapy were able to stop fungal growth completely. Remarkably, ATO (MIC levels) at concentrations 32 mg/l, 16 mg/l and 16 mg/l exhibited bactericidal effects against CA1, CA2 and CA3 after 24 h of exposure, with reductions of 3.0, 3.13 and 4.13 Log10 cfu/ml of the initial inoculum, respectively. Interestingly, the combination of ATO (4 mg/l) with ITR, VOR or KET (sub-MIC level) against different representative isolates produced synergistic and fungicidal effects after 24 h of exposure, with a reduction range (3.0–3.7 Log10 cfu/ml) of the initial inoculum. Whereas, the combination of ATO (4 mg/l) with FLU exhibited synergistic and fungicidal effects after 24 h of exposure, with reduction range (2.34–2.7 Log10 cfu/ml) of the initial inoculum.
Discussion
In recent years, multidrug-resistant fungi have become a serious health problem worldwide. Improper and extensive usage of antifungal drugs results in selective pressure supporting the rise of antifungal-resistant fungi. At present, clinical isolates of Candida spp. are considered to be one of the highly resistant fungi to most traditional antifungal drugs(Costa-de-oliveira and Rodrigues 2020; Tan et al. 2021) Among the different strategies to fight and overcome antifungal resistance, drug repurposing or finding new indications for old drugs represents a promising alternative strategy to drug development and bypass antifungal drug resistance (Vadivoo et al. 2018; Lima et al. 2019; Kim et al. 2020). Considering the scarce number of studies on statin drugs as antifungals against C. albicans, we aimed to further characterize the in vitro activity of ATO alone and in combinations with azole drugs against MDR C. albicans.
In the present study, 94.12% (32/34) of the tested C. albicans isolates were MDR resistant to at least two different azole drugs, whereas 8.82% (3/34) and 5.88% (2/34) of these isolates were resistant and sensitive to all used drugs, respectively. These finding may also highlight the possible impact of the inappropriate antifungal use on the emergence of such massive azole resistance rates in Egypt, the fact that could be attributed to providing treatment for patients without performing antifungal susceptibility testing, which is essentially important to customize an appropriate therapeutic plan for each case individually. The obtained results are consistent with recent studies, which noticed that due to the wide usage of azole drugs and prolonged antifungal therapy, the number of azole-resistant Candida isolates is still increasing (Bhattacharya et al. 2020; Zhang et al. 2020; Tan et al. 2021).
Results of the antibiogram analysis demonstrated that C. albicans isolates exhibited high resistance rates to FLU (58.82%), ITR (52.94%), VOR (47.06%), and KET (35.29%). These findings are partially compatible with those recently reported in Egypt (Hassan et al. 2017; Khairat et al. 2019). (Hassan et al. 2017) revealed that the resistance rates of C. albicans isolates to FLU, KET and ITR reached to 61.2%, 56.7% and 43.3%, receptively. Moreover, these proportions elevated to 93.3%, 87.8% and 100%, respectively (Darma et al. 2020). Another study conducted in Egypt reported that 100% of C. albicans isolates were resistant to FLU and VOR (El-Houssaini et al. 2019). On the contrary, (Khairat et al. 2019) found that the sensitivity of C. albicans isolates to FLU and ITR were 64% and 73%, respectively. Other studies found that the resistance rates of C. albicans to different azole drugs are lower than 20% (Zhang et al. 2014; Nagashima et al. 2016). These variations in azole resistance profiles probably due to the different sources and localities of collections of the clinical specimens in addition to the rational antifungal prescription (El-Houssaini et al. 2019). It is worth noting that the major mechanism responsible for azole resistance is the mutations in ERG11 gene, which encodes the lanosterol 14 α-demethylase enzyme (Henry et al. 2000) or overexpression of drug efflux pumps, which results in a decreased intracellular drug concentration (Paul and Moye-Rowley 2014).
Data of the present study demonstrated that ATO exhibited antifungal activity against various representative isolates of MDR C. albicans. Notably, in silico docking results of ATO and the four azole drugs against the Lanosterol 14-alpha demethylase enzyme (ERG11) of C. albicans demonstrated that the mechanism of action of ATO against C. albicans is similar to that of azole compounds, with docking score (−4.901) lower than azole drugs (≥5.0) due to the formation a single H-bond with Asp 225 and a pi–pi interaction with Thr 229. Additionally, in silico and molecular docking results showed that ATO's binding affinity for HMG-CoA reductase was high (−5.472 kcal/mol) due to the formation of two H-bonds with Gly (C) 715 and Ser (c) 720. These finding are consistent with previous study, which revealed that a research on statin drugs originated with the intention of developing new antimicrobial agents as the inhibition of β-Hydroxy β-methylglutaryl-CoA (HMG-CoA) reductase, results in the death of microorganisms (Liao 2005). Other studies mentioned that the antifungal activates of ATO and other statin drugs can be attributed to the inhibition of ergosterol and isoprenoid-biosynthesis are thought to result in these antifungal properties (Rahal et al. 2015; Rodrigues 2018; Lima et al. 2019) noticed that statin drugs do not act on the fungal membrane or wall, but instead stimulate farnesol-dependent pathogenicity factors such as yeast-to-hyphal transition and biofilm generation.
In this study, ATO exhibited broad-spectrum synergistic interactions with different azole (FLU, ITR, VOR and KET) drugs against the MDR C. albicans isolates. The inhibition zones of azole drugs against these isolates were significantly increased at least two-fold with the presence of ATO, whereas it decreased the inhibition zones of AMP against the same isolates. These synergistic interactions are supported by the results of checkerboard experiments, which demonstrated that the interactions of ATO combinations with different azole drugs were synergism (FICI ≤ 0.5) and MICs of these drugs in these combinations were significantly decreased to the values lower than the susceptible break-points. The synergism between ATO and azole drugs might be attributed to the combined action of these drugs in reducing fungal ergosterol synthesis, which led to increasing cell membrane permeability and increasing the penetration of azoles in the fungal cell (Chamilos et al. 2006; Nyilasi et al. 2010; Cabral et al. 2013; Lima et al. 2019). The obtained results are consistent with previous studies, which mentioned that there were synergistic interactions between statins and azole drugs against Candida spp. Saccharomyces cerevisiae and different filamentous fungi (Lorenz and Parks 1990; Chamilos et al. 2006; Nyilasi et al. 2010). Similarly, the recent studies mentioned that combinations of ATO with azole drugs produced synergistic effects against different Candida sp. (Lima et al. 2019; Eldesouky et al. 2020). Decreasing of inhibition zones of amphotericin B with the presence of ATO is probably due to that ATO reduces the synthesis of the fungal ergosterol, which is the target of amphotericin B, and a decrease in this molecule is one of the mechanisms developed by amphotericin B resistant Candida spp. (Lima et al. 2019).
Herein, the results of time-kill experiments demonstrated that ATO at MIC levels produced fungicidal effects against various representative isolates. Interestingly, the combinations of ATO with ITR, VOR, KET and FLU at sub-MIC levels produced fungicidal effects (≥ 3 Log10 cfu/ml reduction) with the first three drugs and exhibited a fungistatic effect (≤ 3 Log10 cfu/ml reduction) with the fourth drug against these isolates. To our knowledge, this is the first study that has determined the fungicidal interactions between ATO and ITR, VOR, KET or FLU against MDR C. albicans. The same fungicidal effects were associated the combinations of Fluvastatin (Lima et al. 2019) or pitavastatin (Eldesouky et al. 2020) with azole drugs produced fungicidal effects against Candida ssp., especially C. albicans.
Conclusion
Our results suggest new promising combinations of ATO with ITR, VOR, KET or FLU against MDR C. albicans. MICs of azole drugs in these combinations were significantly decreased to the susceptible breakpoints and exhibited fungicidal effects with the first three drugs and a fungistatic effect with the fourth drug. The limitation of this study includes that the number of MDR C. albicans was relatively low and we don’t use reference azoles resistant C. albicans. These limitations were due to the prevalence of COVID-19 in worldwide, especially in Egypt, where all hospitals considered quarantine areas and the imported reference strains were not available during the time of the study. Finally, we agree that further work will be required to confirm these results and to assess the in vivo benefit of these combinations in treatment of MDR C. albicans.
References
Benkert P, Biasini M, Schwede T (2011) Toward the estimation of the absolute quality of individual protein structure models. Bioinformatics 27:343–350. https://doi.org/10.1093/BIOINFORMATICS/BTQ662
Bertoni M, Kiefer F, Biasini M et al (2017) Modeling protein quaternary structure of homo- and hetero-oligomers beyond binary interactions by homology. Sci Rep. https://doi.org/10.1038/S41598-017-09654-8
Bhattacharya S, Sae-Tia S, Fries BC (2020) Candidiasis and mechanisms of antifungal resistance. Antibiotics 9:1–19. https://doi.org/10.3390/antibiotics9060312
Bongomin F, Gago S, Oladele RO, Denning DW (2017) Global and multi-national prevalence of fungal diseases—estimate precision. J Fungi. https://doi.org/10.3390/jof3040057
Cabral ME, Figueroa LIC, Fariña JI (2013) Synergistic antifungal activity of statin-azole associations as witnessed by Saccharomyces cerevisiae- and Candida utilis-bioassays and ergosterol quantification. Rev Iberoam Micol 30:31–38. https://doi.org/10.1016/j.riam.2012.09.006
Campoy S, Adrio JL (2017) Antifungals. Biochem Pharmacol 133:86–96. https://doi.org/10.1016/J.BCP.2016.11.019
Chamilos G, Lewis RE, Kontoyiannis DP (2006) Lovastatin has significant activity against zygomycetes and interacts synergistically with voriconazole. Antimicrob Agents Chemother 50:96–103. https://doi.org/10.1128/AAC.50.1.96-103.2006
CLSI. (2017) Performance Standards for Antimicrobial Susceptibility Testing; Twenty-Seventh Informational Supplement. CLSI Document M100-S27.
Costa-de-oliveira S, Rodrigues AG (2020) Candida albicans antifungal resistance and tolerance in bloodstream infections: the triad yeast-host-antifungal. Microorganisms. https://doi.org/10.3390/microorganisms8020154
Darma S, Ambara A, Aman AT et al (2020) High frequency of azole resistant Candida spp. colonization among presumptive multidrug resistant tuberculosis (MDR-TB) patients. PLoS One 15:1–12. https://doi.org/10.1371/journal.pone.0242542
De Angelis G, Menchinelli G, Torelli R et al (2020) Different detection capabilities by mycological media for Candida isolates from mono- or dual-species cultures. PLoS One 15:1–9. https://doi.org/10.1371/journal.pone.0226467
Di Bello E, Zwergel C, Mai A, Valente S (2020) The innovative potential of statins in cancer: new targets for new therapies. Front Chem. https://doi.org/10.3389/FCHEM.2020.00516
El-Houssaini H, Elkhatib W, Elnabawy O, Nasser H (2019) Antifungal resistance and predominance of virulence determinants among Candida albicans isolated from various clinical specimens. Arch Pharm Sci Ain Shams Univ 3:11–20. https://doi.org/10.21608/aps.2019.20210
Eldesouky HE, Salama EA, Li X et al (2020) Repurposing approach identifies pitavastatin as a potent azole chemosensitizing agent effective against azole-resistant Candida species. Sci Rep 10:1–12. https://doi.org/10.1038/s41598-020-64571-7
Esfahani AN, Golestannejad Z, Khozeimeh F, et al (2019) Antifungal effect of Atorvastatin against Candida species in comparison to Fluconazole and Nystatin. Med Pharm Reports 92:368–373. https://doi.org/10.15386/mpr-1209
Espinel-Ingroff A, Colombo AL, Cordoba S et al (2016) International evaluation of MIC distributions and epidemiological cutoff value (ECV) definitions for Fusarium species identified by molecular methods for the CLSI broth microdilution method. Antimicrob Agents Chemother 60:1079–1084. https://doi.org/10.1128/AAC.02456-15
Friedman DZP, Schwartz IS (2019) Emerging fungal infections: new patients, new patterns, and new pathogens. J Fungi. https://doi.org/10.3390/jof5030067
Friesner RA, Murphy RB, Repasky MP et al (2006) Extra precision glide: docking and scoring incorporating a model of hydrophobic enclosure for protein-ligand complexes. J Med Chem 49:6177–6196. https://doi.org/10.1021/JM051256O
Gintjee TJ, Donnelley MA, Thompson GR (2020) Aspiring antifungals: review of current antifungal pipeline developments. J Fungi 6:28. https://doi.org/10.3390/jof6010028
Guex N, Peitsch M, Electrophoresis TS (2009) undefined (2009) Automated comparative protein structure modeling with SWISS-MODEL and Swiss-PdbViewer: a historical perspective. Wiley Online Libr. https://doi.org/10.1002/elps.200900140
Gupta A, Stokes W, Eguchi M et al (2019) Statin use associated with improved overall and cancer specific survival in patients with head and neck cancer. Oral Oncol 90:54–66. https://doi.org/10.1016/J.ORALONCOLOGY.2019.01.019
Hassan A, Usman J, Kaleem F, et al (2017) Evaluation of different detection methods of biofilm formation in the clinical isolates. Braz J Infect Dis 15:305–11
Henry KW, Nickels JT, Edlind TD (2000) Upregulation of ERG genes in Candida species by azoles and other sterol biosynthesis inhibitors. Antimicrob Agents Chemother 44:2693–2700. https://doi.org/10.1128/AAC.44.10.2693-2700.2000
Juárez-López D, Schcolnik-Cabrera A (2021) Drug repurposing: considerations to surpass while re-directing old compounds for new treatments. Arch Med Res 52:243–251. https://doi.org/10.1016/J.ARCMED.2020.10.021
Keniya MV, Sabherwal M, Wilson RK et al (2018) Crystal structures of full-length lanosterol 14α-demethylases of prominent fungal pathogens candida albicans and candida glabrata provide tools for antifungal discovery. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.01134-18
Khairat SM, Sayed AM, Nabih M et al (2019) Prevalence of Candida blood stream infections among children in tertiary care hospital: detection of species and antifungal susceptibility. Infect Drug Resist 12:2409–2416. https://doi.org/10.2147/IDR.S196972
Kim JH, Cheng LW, Chan KL et al (2020) Antifungal drug repurposing. Antibiotics 9:1–29. https://doi.org/10.3390/antibiotics9110812
Ko HHT, Lareu RR, Dix BR, Hughes JD (2017) Statins: antimicrobial resistance breakers or makers? PeerJ. https://doi.org/10.7717/peerj.3952
Koushki K, Shahbaz SK, Mashayekhi K et al (2021) Anti-inflammatory action of statins in cardiovascular disease: the role of inflammasome and toll-like receptor pathways. Clin Rev Allergy Immunol 60:175–199. https://doi.org/10.1007/s12016-020-08791-9
Lee YS, Jang KA, Cha JD (2012) Synergistic antibacterial effect between silibinin and antibiotics in oral bacteria. J Biomed Biotechnol. https://doi.org/10.1155/2012/618081
Li H, Zhang C, Chen Z et al (2014) A promising approach of overcoming the intrinsic resistance of Candida krusei to fluconazole (FLC) − Combining tacrolimus with FLC. FEMS Yeast Res 14:808–811. https://doi.org/10.1111/1567-1364.12163
Liao JK (2005) Clinical implications for statin pleiotropy. Curr Opin Lipidol 16:624–629. https://doi.org/10.1097/01.mol.0000191913.16321.60
Lima W, Parreira A, … LN-J of, 2018 undefined (2018) Absence of antibacterial, anti-candida, and anti-dengue activities of a surfactin isolated from Bacillus subtilis. researchgate.net. https://doi.org/10.4103/jpnr.JPNR_11_17
Lima WG, Alves-Nascimento LA, Andrade JT, Vieira L, de Azambuja Ribeiro RIM, Thomé RG, dos Santos HB, Ferreira JMS, Soares AC (2019) Are the Statins promising antifungal agents against invasive candidiasis? Biomed Pharmacother 111:270–281. https://doi.org/10.1016/j.biopha.2018.12.076
Lorenz RT, Parks LW (1990) Effects of lovastatin (mevinolin) on sterol levels and on activity of azoles in Saccharomyces cerevisiae. Antimicrob Agents Chemother 34:1660–1665. https://doi.org/10.1128/AAC.34.9.1660
Matthaiou DK, Christodoulopoulou T, Dimopoulos G (2015) How to treat fungal infections in ICU patients. BMC Infectious Diseases 15:1–8. https://doi.org/10.1186/s12879-015-0934-8
Nagashima M, Yamagishi Y, Mikamo H (2016) Antifungal susceptibilities of Candida species isolated from the patients with vaginal candidiasis. J Infect Chemother 22:124–126. https://doi.org/10.1016/j.jiac.2015.08.008
Nyilasi I, Kocsubé S, Krizsán K et al (2010) In vitro synergistic interactions of the effects of various statins and azoles against some clinically important fungi. FEMS Microbiol Lett 307:175–184. https://doi.org/10.1111/j.1574-6968.2010.01972.x
Pappas PG, Kauffman CA, Andes DR et al (2015) Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis 62:e1–e50. https://doi.org/10.1093/cid/civ933
Pappas PG, Lionakis MS, Arendrup MC et al (2018) Invasive candidiasis. Nat Rev Dis Prim 4:1–20. https://doi.org/10.1038/nrdp.2018.26
Paul S, Moye-Rowley WS (2014) Multidrug resistance in fungi: regulation of transporter-encoding gene expression. Front Physiol. https://doi.org/10.3389/FPHYS.2014.00143/FULL
Perlin D, Rautemaa-RichardsonAlastruez-Izquierdo RD (2017) The global problem of antifungal resistance: prevalence, mechanisms, and management. Lancet Infect Dis 17:e383–e392. https://doi.org/10.1016/S1473-3099(17)30316-X
Pristov KE, Ghannoum MA (2019) Resistance of Candida to azoles and echinocandins worldwide. Clin Microbiol Infect 25:792–798. https://doi.org/10.1016/j.cmi.2019.03.028
Rahal EA, Constantin WN, Zeidan N, Abdelnoor AM (2015) Atorvastatin reduces the survival of Candida albicans-infected BALB/c mice. Front Microbiol 6:1–8. https://doi.org/10.3389/fmicb.2015.01474
Remmert M, Biegert A, Hauser A, Söding J (2012) HHblits: lightning-fast iterative protein sequence searching by HMM-HMM alignment. Nat Methods 9:173–175. https://doi.org/10.1038/NMETH.1818
Rodrigues ML (2018) The multifunctional fungal ergosterol. mBio. https://doi.org/10.1128/MBIO.01755-18
Sanglard D (2016) Emerging threats in antifungal-resistant fungal pathogens. Front Med 3:1–10. https://doi.org/10.3389/fmed.2016.00011
Santos M, Rocha F, Silva D et al (2018) Triazole - chalcones : lack of antibacterial, anti - candida, and anti - dengue virus activities. J Pharm Negative Results 9:39–43. https://doi.org/10.4103/jpnr.JPNR
Sarver RW, Bills E, Bolton G et al (2008) Thermodynamic and structure guided design of statin based inhibitors of 3-hydroxy-3-methylglutaryl coenzyme A reductase. J Med Chem 51:3804–3813. https://doi.org/10.1021/JM7015057
Scorneaux B, Angulo D, Borroto-Esoda K et al (2017) SCY-078 is fungicidal against Candida species in time-kill studies. Antimicrob Agents Chemother 61:1–10. https://doi.org/10.1128/AAC.01961-16
Tan J, Jiang S, Tan L et al (2021) Antifungal activity of minocycline and azoles against fluconazole-resistant Candida species. Front Microbiol. https://doi.org/10.3389/fmicb.2021.649026
Vadivoo V, Dhinakar Raj G, Balasubramanian S, Subramanion S (2018) Elucidation of possible antibacterial effects of statins against primary pathogens of mastitis in cows 7:30–33
Wall G, Lopez-Ribot JL (2020) Screening repurposing libraries for identification of drugs with novel antifungal activity. Antimicrob Agents Chemother. https://doi.org/10.1128/AAC.00924-20
Waterhouse A, Bertoni M, Bienert S et al (2018) SWISS-MODEL: homology modelling of protein structures and complexes. Nucleic Acids Res 46:W296–W303. https://doi.org/10.1093/NAR/GKY427
Zhang JY, Liu JH, Di LF et al (2014) Vulvovaginal candidiasis: species distribution, fluconazole resistance and drug efflux pump gene overexpression. Mycoses 57:584–591. https://doi.org/10.1111/myc.12204
Zhang MR, Zhao F, Wang S et al (2020) Molecular mechanism of azoles resistant Candida albicans in a patient with chronic mucocutaneous candidiasis. BMC Infect Dis 20:1–6. https://doi.org/10.1186/s12879-020-4856-8
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mahmoud, D.E., Faraag, A.H.I. & Abu El-Wafa, W.M. In vitro study on the potential fungicidal effects of atorvastatin in combination with some azole drugs against multidrug resistant Candida albicans. World J Microbiol Biotechnol 37, 191 (2021). https://doi.org/10.1007/s11274-021-03158-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11274-021-03158-4