Abstract
Candida albicans is a major invasive pathogen, and the development of strains resistant to conventional antifungal agents has been reported in recent years. We evaluated the antifungal activity of 44 compounds against Candida strains. Magnoflorine showed the highest growth inhibitory activity of the tested Candida strains, with a minimum inhibitory concentration (MIC) of 50 μg/mL based on microdilution antifungal susceptibility testing. Disk diffusion assay confirmed the antifungal activity of magnoflorine and revealed that this activity was stable over 3 days compared to those of berberine and cinnamaldehyde. Cytotoxicity testing showed that magnoflorine could potentially be used in a clinical setting because it didn’t have any toxicity to HaCaT cells even in 200 μg/mL of treatment. Magnoflorine at 50 μg/mL inhibited 55.91 ± 7.17% of alpha-glucosidase activity which is required for normal cell wall composition and virulence of Candida albicans. Magnoflorine also reduced the formation of C. albicans’ biofilm. Combined treatment with magnoflorine and miconazole decreased the amount of miconazole required to kill various Candida albicans. Therefore, magnoflorine is a good candidate lead compound for novel antifungal agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infection by invasive fungal pathogens is on the rise and poses a major human health risk (Cornely et al. 2017) Candida albicans is one of the major invasive fungal pathogens encountered (Shao et al. 2016). Infection by this pathogen causes visceral or superficial mycoses on the mouth, neck, digestive tract, and vagina (Bramono et al. 1995; Sato et al. 2017). Immunocompromised patients in particular are susceptible to infection by this pathogen (Haque et al. 2016). Although various compounds, including azole, are currently used to treat Candida infection, the mortality of patients with Candida infection is 15–25% (Pal 2017; Chandra et al. 2018). The occurrence of azole-resistant Candida strains has also been reported and currently used drugs have limitations because of their toxicity (Zida et al. 2017; Whaley et al. 2016; Haque et al. 2016). There is therefore an urgent need for new drugs to control Candida infections. Cinnamaldehyde and berberine are examples of novel antifungal agents that have anti-Candida activity (Cornely et al. 2017; Shao et al. 2016; Siddiqua et al. 2015; Zorić et al. 2017).
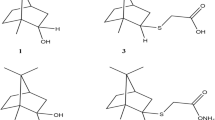
We evaluated the antifungal activity of 44 natural compounds to find new agents that can be used to treat Candida albicans infections. Through the microdilution antifungal susceptibility test and disk diffusion assay, we found one of candidate, magnoflorine (MF) (Chen et al. 2009). MF is classified as an aporphine alkaloid (Supplementary Fig. 1) and has been shown to have antifungal activity against Penicillium avellaneum and Penicillium oryzae (Chen et al. 2009). MF has been found in the following plants: Acoruscalamus, Tinospora cordifolia, Celestrus paniculatus, Magnolia officinalis and Clematis parviloba has been shown to have antifungal, anticancer, antioxidant, anti-inflammatory, as well as antiviral activity (Singh et al. 2010; Li and Wang 2014; Chen et al. 2009). Therefore, in this study, we tested magnoflorine as a good candidate lead compound for novel antifungal agents by alpha-glucosidase inhibition activity and decreased formation of C. albicans’ biofilm.
Materials and methods
Candida strains preparation
Candida strains used in present study are listed in Table 1. All strains were stored in 20% glycerol at − 70 °C and were cultured in YPD plates [peptone 20 g/L (BD Difco, Belgium), yeast extract 10 g/L (BD Difco, Belgium) and 2% glucose (w/v) (Daejung, Korea)].
Antifungal susceptibility microdilution assay
To obtain the Minimal Inhibitory Concentration (MIC), microdilution assay was performed as described in CLSI document M27-A (Balouiri et al. 2016; CCLS 2008). Stock compounds that were supplied as pure standard compounds (from Sigma-Aldrich, USA) were prepared in dimethyl sulfoxide (DMSO) at a final concentration of 10 mg/mL.
100 μL of MOPS (morpholine propane sulfonic acid)-buffered RPMI 1640 medium containing each compound was added to the wells of 96-well flat-bottomed plates (SPL, Korea). The final compound concentrations ranged from 200 to 1.5625 μg/mL.
A colony of each strain from 24 h cultured YPD agar plates was inoculated into 3 mL of YPD broth that was incubated at 30 °C overnight, and the medium was changed to YPD broth to adjust the cell number to 5 × 104 CFU/mL. 100 μL of the inoculum suspension was added to each well. Plates were incubated at 30 °C for 24 h, 48 h, and 72 h.
To obtain the Minimal Fungicidal Concentration (MFC), 10 µL of each serial dilution was taken from each well and spread on sabouraud dextrose agar. Plates were incubated at 30 °C for 48 h. The MFC was defined as the lowest drug concentration that yielded three or fewer colonies (i.e. 99 % of the inoculum was killed). Growth control and sterilized medium control wells were included in each experiment and miconazole was used as the positive control (Shin and Kim 2016).
Antifungal susceptibility testing by disk diffusion assay
Disk diffusion susceptibility testing of 44 compounds was performed as described in CLSI (formerly NCCLS) document M44-A (Balouiri et al. 2016; Lozano-Chiu et al. 1999). YPD agar plates were visually examined before use, and medium containing Candida strains was poured to uniform depth. The inoculum was adjusted to a density of a McFarland 0.5 standard (EUCAST 2017). Antibiotic test disks with a diameter of 6-mm containing 100 μg of each compound were placed on the agar surface with sterile forceps. Plates were incubated at 30 °C, and the zone of inhibition was measured at 24, 48, and 72 h.
Cell growth test
Inoculation and culture of a colony of C. albicans were followed as Antifungal susceptibility microdilution assay. Then the final compound concentrations ranged from 300 to 18.75 μM. Plates were incubated at 30 °C and growth rate was measured at OD600 using a microplate reader (BioTek Instruments, Korea) at 0, 3, 6, 9, 12 and 24 h (Mumma et al. 2008).
Crude alpha-glucosidase inhibition assay
Using a slightly modified alpha-glucosidase inhibition assay in vitro, C. albicans (KCTC7965) was cultured overnight in 0.6% maltose medium, washed with PBS (pH 6.8), and then disrupted using glass beads (0.4–0.6 mm diameter, DAIHAN-Scientific, Korea) (Patel and Mishra 2012). The suspension was centrifuged at 13,500×g for 10 min. 800 μL of washed suspension was put in a 1.5 mL tube.
To measure alpha-glucosidase inhibition activity, 96-well plates were used. Each well contained 80 μL PBS buffer (pH 6.8), 9 μL crude enzyme, and 1 μL of compound or vehicle control. The mix of compound and enzyme was pre-incubated for 20 min, and then the substrate, p-nitrophenyl-alpha-D-glucopyranoside (PNPG) (Sigma Aldrich), was added. Reaction was stopped by adding 100 μL 0.1 M cold Na2CO3 after 30 min. Three blanks were included: blank 1 with 90 μL PBS (pH 6.8) and 10 μL PNPG; blank 2 with 9 μL crude enzyme and 91 μL PBS (pH 6.8), blank 3 with 9 μL crude enzyme, 81 μL PBS pH 6.8, and 10 μL PNPG. Tests were performed in quadruplicate on the same plate, and absorbance was measured using a microplate reader (BioTek Instruments, Korea) at a wavelength of 400 nm.
Cytotoxicity assays
The cytotoxicity of MF against HaCaT cells was tested using a slightly modified cell-based MTT assay (Shin and Kim 2016). Briefly, HaCaT cells in Dulbecco’s modified eagle’s medium (DMEM) containing various concentrations of MF (0–600 µM) were added to the wells of a 96-well plate at a density of 104 cells per well. After incubation for 48 h, MTT (3-(4,5-dimethyl-thiazol-2-yl)-2,5-diphenyltetrazolium bromide, Sigma) in PBS was added to a final concentration of 0.5 mg/mL, followed by incubation for 3 h at 37 °C. The medium was then removed, and cells were suspended in 100 μL of 100% DMSO for 10 min. Cell viability was calculated from optical density (OD540) values measured using a microplate reader (BioTek Instruments, Korea) and are reported as percentage of the vehicle control.
Antifungal synergy testing
Antifungal synergy between miconazole and MF against C. albicans (KCTC7965) was tested using the broth microdilution assay with a checkerboard design (Shin and Kim 2016; Drogari-Apiranthitou et al. 2012). After miconazole and MF were serially two-fold diluted, 100 µL of compound in MOPS-buffered RPMI 1640 was transferred into each well of a 96-well plate. 100 μL of C. albicans at a concentration of 104 CFU/mL was added per well. Final concentrations of both miconazole and MF ranged from 100 to 1.562 μg/mL. MIC values of individual compounds were determined on the same plate. Tests were performed in triplicate. The fractional inhibitory concentration index (FICI) was used to investigate if the two compounds had synergistic effects (Shin and Kim 2016; Patel and Mishra 2012).
Detection of C. albicans biofilm formation
Detection of the biofilm formation was measured following crystal violet assay method (Dhale et al. 2014). Following the method of Antifungal susceptibility microdilution assay, 5 × 105 CFU/mL of C. albicans was added to the wells of 96-well flat-bottomed plates (SPL, Korea) and MF was added together. The final compound concentrations ranged from 300 to 2.343 μM. Plates were incubated at 30 °C for 24 h. Growth control and sterilized medium control wells were included in each experiment. The plate was washed with 200 μL distilled water three times. After washing, the plate was stained with 200 μL of 0.4% aqueous crystal violet solution for 45 min. After staining, each well was washed four times with 200 μL distilled water and instantly destained with 200 μL of absolute ethanol for 45 min. The plate was measured at 595 nm with a microplate reader (BioTek Instruments, Korea). The biofilm formation was normalized to control using the following formula [(1 − (OD595DMSO − OD595Compound)/OD595DMSO) × 100%] (Nikolić et al. 2014).
Statistical analysis
All tests were performed in triplicate of independent experiments. All statistical calculations were analyzed on Graphpad Prism software (San Diego, CA, USA) by one-way analysis of variance (ANOVA) with appropriate correction for multiple comparison (significance level, α = 0.05).
Results
In vitro antifungal activity
The growth inhibitory activity against Candida strains of the 44 compounds was evaluated using broth microdilution assays (Table 2 and Supplementary Table 1). The MIC values of miconazole ranged from 0.3906 to 6.25 μg/mL after a 48-h incubation depending on Candida strain. Berberine (BBR) had an MIC value of 100 μg/mL against C. albicans as well C. parapsilosis var. parapsilosis, but weak activity against C. tropicalis and C. glabrata. The MIC value of cinamaldehyde (CNM) against C. albicans was also 100 μg/mL. MF had stronger inhibitory activity than BBR and CNM against C. albicans (MIC of 50–100 μg/mL) and the same MIC as BBR and CNM against C. parapsilosis var. parapsilosis after 48 h. 100 μg/mL of MF inhibited the growth of C. glabrata after 24 h, but not 48 h. The MFC value of MF against C. albicans is 200 µg/mL.
To determine the stability of the compounds, MIC values were measured every day for 3 days. CNM and BBR had the highest inhibitory activity against C. albicans at 24 h and 48 h, but this decreased after 72 h. In contrast, the growth inhibitory activity of MF against C. albicans did not decrease over 3 days (Table 3).
Disk diffusion assay
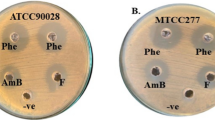
Zones of inhibition of miconazole, BBR, CNM, and MF against 5 Candida strains were reported in Supplementary Table 2. The inhibition zone size of miconazole ranged from 13 to 18 mm after 24 h, then decreased slightly in diameter after 48 h and 72 h. Miconazole inhibition zone diameters were fairly constant for C. glabrata, C. tropicalis var. tropicalis, and C. parapsilosis var. parapsilosis. BBR showed strong activity against C. albicans up to 24 h, reduced activity after 48 h, and no activity after 72 h, but showed the strongest activity against Candida tropicalis var. tropicalis among the tested compounds. CNM had the broadest activity against the tested strains after 24 h, but this activity was reduced after 72 h. MF had a similar-sized zone of inhibition to BBR against the tested strains, but a smaller zone of inhibition than CNM. Only MF showed anti-C. albicans activity after 72 h of incubation (Fig. 1).
Cell growth test
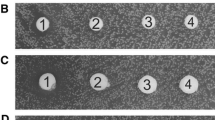
With our results, Cell growth test showed the differences in C. albicans growth of various concentrations of MF over time (Fig. 2). Regardless of time, MF at 150 and 300 µM inhibited cell growth strongly. MF at 75 µM also decreased C. albicans’ growth, but under 37.5 µM of its concentration MF did not disturb cell growth as time went on.
Crude alpha-glucosidase inhibition assay
To identify the antifungal mechanism related with MF, alpha-glucosidase activity was assessed. Pre-assessment indicated that the optimal conditions were 2 mM substrate, 20 min pre-incubation with the substrate, and a 30 min activation. MF at 150 μM inhibited alpha-glucosidase activity by 60.08% (Fig. 3a). However, BBR and CNM didn’t show any inhibitory effect to alpha-glucosidase activity even at 300 μM treatment (data not shown).
a Inhibition of alpha-glucosidase activity of C.albicans by magnoflorine. b Cell Cytotoxicity of magnoflorine to human HaCaT cells. c Magnoflorine-dependent inhibition of biofilm formation of C. albicans. Data represent mean ± S.D from at least three independent experiments. *p < 0.05. Data represent mean ± S.D from at least three independent experiments. ***p < 0.01
Cytotoxicity assays
Cytotoxicity of MF against HaCaT cells was tested to evaluate whether this compound is cytotoxic to human cells (Fig. 3b). MF didn’t have any toxicity to HaCaT cells even in 600 μM of treatment.
Anti-candida synergy testing
To determine if miconazole and MF had synergistic effects, C. albicans (KCTC7965) was treated with various concentrations of both compounds, and a weak synergistic effect was observed (FICI = 0.75 and 1). Interestingly, the MIC value of miconazole decreased from 3.125 μg/mL to 1.5625 μg/mL when applied in combination with 6.25 μg/mL MF.
Detection of C. albicans biofilm formation
After treatment of each concentration of MF, biofilm formation of C. albicans was detected. MF dose-dependently reduced the biofilm formation of C. albicans and 150 μM of MF treatment completely inhibited the biofilm formation (Fig. 3c).
Discussion
Aporphine alkaloids from plants have shown a variety of pharmacological and biological effects, including antioxidation (Hisatomi et al. 2000) and anti-inflammation (Küpeli et al. 2002). Even though antifungal activities of magnoflorine against only Penicillium avellaneum and Penicillium oryzae were reported (Chen et al. 2009), our study showed the anti-candida activity by inhibition of alpha-glucosidase and also biofilm formation.
MF, CNM, and BBR showed antifungal activity against C. albicans and some other Candida strains based on MIC values, consistent with previous studies (Whaley et al. 2016; Siddiqua et al. 2015; Shai et al. 2010).
MIC of BBR measured in this study (100 µg/mL) was higher than that reported previously (16 µg/mL). This might be due to differences in inoculum preparation between the two studies. Shao et al. used 103 CFU/mL of C. albicans rather than 0.5–2.5 × 105 CFU/mL (Shao et al. 2016; Pootong 2017).
The MIC of CNM, which was 100 µg/mL at 0.5 × 105 CFU/mL, is concordant with that reported in a previous study (125 µg/mL for C. albicans ATCC10231 at 1–5 × 106 CFU/mL) (Shai et al. 2010).
Interestingly, MF had the highest stable antifungal activity against C. albicans KTCC7965 (ATCC 10231) (Tables 2, 3), with MICMF = 50 μg/mL. This result explains the anti-Candida activity of Zanthoxylum rhoifolium, which contains MF (Alastruey-Izquierdo et al. 2015).
Disk diffusion results confirmed the antifungal effectiveness of BBR, CNM, and MF against Candida strains, including C. albicans. Although the inhibition zones of BBR and CNM were larger than that of MF, the zones decreased in size after 48 h and 72 h of incubation, whereas that of MF remained the same (Supplementary Table 2).
Understanding the mode of action of a compound can lead to the development of novel drugs with low cytotoxicity (Tavares et al. 2014). Alpha-glucosidase (EC 3.2.1.20) is a glucosidase located in the brush border of the small intestine that acts upon α (1 → 4) bonds. This inhibition lowers the rate of glucose absorption through delayed carbohydrate digestion and extended digestion time. Therefore, alpha-glucosidase inhibitors have been widely used as the anti-diabetic drugs for diabetes mellitus type 2 (Bischoff 1995). Magnoflorine possessed the potential activity as alpha-glucosidase inhibitor in vitro and in vivo (Patel and Mishra 2012).
The cell wall of C. albicans is the immediate point of contact between the fungus and host and therefore plays a key role in the host-fungus interaction. The outer layer of cell wall is enriched with highly glycosylated mannoproteins (Klis 2001). The mannoproteins, which processed by alpha-glycosidase have important roles in adhesion, antigenicity, modulation of the host immune response, and recognition of this fungus by innate immune cells (Patel and Mishra 2012; Bates et al. 2006; Ngan et al. 2012). Previously, Ora et al. demonstrated the importance of alpha-glycosidase in C. albicans as an enzyme for cell wall assembly as well as the negative consequences when cells lacked alpha-glucosidase. Therefore, N-oligosaccharide processing by ER alpha-glycosidase was required for cell wall integrity and for host-fungus interactions (Ora-Montes et al. 2007). MF dose-dependently inhibited alpha-glucosidase activity (Table 4), suggesting that the MF-induced reduction in growth of Candida is correlated to its ability to inhibit alpha-glucosidase activity (Bramono et al. 1995).
In addition, MF was not cytotoxic against human HaCaT cells, suggesting that MF might not have side-effects in humans (Dhale et al. 2014; Taff et al. 2012; Shin et al. 2002). Dhale et al. explained that C. albicans is most commonly associated with biofilm formation. MF decreases biofilm formation and this shows that toxicity of C. albicans can be reduced with MF treatment. MF therefore holds promise as a lead compound for the development of novel and effective antifungal agents.
Although there was no apparent synergism between MF and miconazole, the amount of miconazole required to kill Candida was two-fold reduced in the presence of MF. This is an obvious benefit to the use of MF, as a smaller amount of miconazole is required for pathogen control.
In conclusion, MF has a stable antifungal activity to some Candida strains by inhibiting alpha-glucosidase. MF is also shown less cytotoxicity against human cells. Depending on this study, magnoflorine is a good leading compound for novel antifungal agents.
References
Alastruey-Izquierdo A, Melhem MS, Bonfietti LX, Rodriguez-Tudela JL (2015) Susceptibility test for fungi: clinical and laboratorial correlations in medical mycology. Rev Inst Med Trop Sao Paulo 57:57–64
Balouiri M, Sadiki M, Ibnsouda SK (2016) Methods for in vitro evaluating antimicrobial activity: a review. J Pharm Anal 6:71–79
Bates S, Hughes HB, Munro CA, Thomas WP, MacCallum DM, Bertram G, Atrih A, Ferguson MA, Brown AJ, Odds FC, Gow NA (2006) Outer chain N-glycans are required for cell wall integrity and virulence of Candida albicans. J Biol Chem 281:90–98
Bischoff H (1995) The mechanism of alpha-glucosidase inhibition in the management of diabetes. Clin Invest Med 18:303–311
Bramono K, Tsuboi R, Ogawa H (1995) A carbohydrate-degrading enzyme from Candida albicans: correlation between a-glucosidase activity and fungal growth. Mycose 38:349–353
CCLS document M27-A3 (2008) National Committee for Clinical Laboratory Standards, reference method for broth dilution antifungal susceptibility testing of yeasts. Pennsylvania, USA
Chandra J, Long L, Isham N, Mukherjee PK, DiSciullo G, Appelt K, Ghannoum MA (2018) In vitro and in vivo activity of a novel catheter lock solution against bacterial and fungal biofilms. Antimicrob Agents Chemother 4:AAC.00722 – 18
Chen JH, Du ZZ, Shen YM, Yang YP (2009) Aporphine alkaloids from Clematis parviloba and their antifungal activity. Arch Pharm Res 32:3–5
Cornely OA, Lass-Florl C, Lagrou K, Valentina AA (2017) Improving outcome of fungal diseases—guiding experts and patients towards excellence. Mycoses 60:420–425
Dhale RP, Ghorpade MV, Dharmadhikari CA (2014) Comparison of various methods used to detect biofilm production of Candida species. J Clin Diagn Res 8:DC18–DC20
Drogari-Apiranthitou M, Mantopoulou FD, Skiada A, Kanioura L, Grammatikou M, Vrioni G, Mitroussia-Ziouva A, Tsakris A, Petrikkos G (2012) In vitro antifungal susceptibility of filamentous fungi causing rare infections: synergy testing of amphotericin B, posaconazole and anidulafungin in pairs. J Antimicrob Chemother 67:1937–1940
EUCAST (2017) Antimicrobial susceptibility testing EUCAST disk diffusion method. ESCMID Manual v 6:0
Haque F, Alfatah M, Ganesan K, Bhattacharyya MS (2016) Inhibitory effect of sophorolipid on Candida albicans biofilm formation and hyphal growth. Sci Rep 6:23575
Hisatomi E, Matsui M, Kubota K, Kobayashi A (2000) Antioxidative activity in the pericarp and seed of Japanese pepper (Xanthoxylum piperitum DC). J Agric Food Chem 48:4924–4928
Klis FM, Groot PD, Hellungwerf K (2001) Molecular organization of the cell wall of Candida albicans. Med Mycol 39:1–8
Küpeli E, Koşar M, Yeşilada E, Hüsnü K, Başer C (2002) A comparative study on the anti-inflammatory, antinociceptive and antipyretic effects of isoquinoline alkaloids from the roots of Turkish Berberis species. Life Sci 72:645–657
Li C, Wang M-H (2014) Potential biological activities of magnoflorine: a compound from Aristolochia debilis Sieb. et Zucc. Korean J Plant Resour 27:223–228
Lozano-Chiu M, Nelson PW, Paetznick VL, Rex JH (1999) Disk diffusion method for determining susceptibilities of Candida spp. to MK-0991. J Clin Microbiol 37:1625–1627
Mumma JO, Chhay JS, Ross KL, Eaton JS, Newell-Litwa KA, Fridovich-Keil JL (2008) Distinct roles of galactose-1P in galactose-mediated growth arrest of yeast deficient in galactose-1P uridylyltransferase (GALT) and UDP-galactose 4′-epimerase (GALE). Mol Genet Metab 93:160–171
Ngan LTM, Moon JK, Shibamoto T, Ahn YJ (2012) Growth-inhibiting, bactericidal, and urease inhibitory effects of Paeonia lactiflora root constituents and related compounds on antibiotic-susceptible and -resistant strains of Helicobacter pylori. J Agric Food Chem 60:9062–9073
Nikolić M, Vasić S, Đurđević J, Stefanović O, Čomić L (2014) Antibacterial and anti-biofilm activity of ginger (Zingiber officinale (Roscoe)) ethanolic extract. Kragujevac J Sci 36:129–136
Ora-Montes HM, Bates S, Netea MG et al (2007) Endoplasmic reticulum alpha-glycosidases of Candida albicans are required for N glycosylation, cell wall integrity, and normal host-fungus interaction. Eukaryot Cell 6:2184–2193
Pal M (2017) Morbidity and mortality due to fungal infections. J Appl Microbiol Biochem 1:1–3
Patel MB, Mishra SM (2012) Magnoflorine from Tinospora cordifolia stem inhibits α-glucosidase and is antiglycemic in rats. J Funct Foods 4:79–86
Pootong A, Norrapong B, Cowawintaweewat S (2017) Antifungal activity of cinnamaldehyde against Candida albicans. Southeast Asian J Trop Med 48:150–158
Sato T, Kishi M, Suda M et al (2017) Prevalence of Candida albicans and non-albicans on the tongue dorsa of elderly people living in a post-disaster area: a cross-sectional survey. BMC Oral Health 17:51
Shai LJ, Masoko P, Mokgotho MP, Magano SR, Mogale AM, Boaduo N, Eloff JN (2010) Yeast alpha glucosidase inhibitory and antioxidant activities of six medicinal plants collected in Phalaborwa, South Africa. S Afr J Bot 76:465–470
Shao J, Shi G, Wang TM, Wu DQ, Wang CZ (2016) Antiproliferation of berberine in combination with fluconazole from the perspectives of reactive oxygen species, ergosterol and drug efflux in a fluconazole-resistant Candida tropicalis isolate. Front Microbiol 7:15–16
Shin YK, Kim KY (2016) Macelignan inhibits bee pathogenic fungi Ascophaera apis growth through HOG1 pathway. Braz J Med Biol Res 49:5313
Shin JH, Kee SJ, Shin MG, Kim SH, Shin DH, Lee SK, Suh SP, Ryang DW (2002) Biofilm production by isolates of Candida species recovered from nonneutropenic patients: comparison of bloodstream isolates with isolates from other sources. J Clin Microbiol 30:1244–1248
Siddiqua S, Anusha BA, Ashwini LS, Negi PS (2015) Antibacterial activity of cinnamaldehyde and clove oil: effect on selected foodborne pathogens in model food systems and watermelon juice. J Food Sci Technol 52:5834–5841
Singh S, Srivastava R, Choudhary S (2010) Antifungal and HPLC analysis of the crude extracts of Acorus calamus, Tinospora cordifolia and Celestrus paniculatus. Int J Agric Technol 6:149–158
Taff HT, Nett JE, Andes DR (2012) Comparative analysis of Candida biofilm quantitation assays. Med Mycol 50:214–218
Tavares LdC, Zanon G, Weber AD et al (2014) Structure-activity relationship of benzophenanthridine alkaloids from Zanthoxylum rhoifolium having antimicrobial activity. PLoS ONE 9:97000
Whaley SG, Berkow EL, Rybak JM, Nishimoto AT, Barker KS, Rogers PD (2016) Azole antifungal resistance in Candida albicans and emerging non-albicans Candida species. Front Microbiol 7:02173
Zida A, Bamba S, Yacouba A, Ouedraogo-Traore R, Guiguemdé RT (2017) Anti-Candida albicans natural products, sources of new antifungal drugs: a review. J Mycol Med 27:01–19
Zorić N, Kosalec I, Tomić S, Bobnjarić I, Jug M, Vlainić T, Vlainić J (2017) Membrane of Candida albicans as a target of berberine. BMC Complement Altern Med 17:268
Acknowledgements
This research was supported by the Basic Science Research Program through grants from the National Research Foundation of Korea (NRF) funded by the Ministry of Education (NRF-2015R1D1A1A01061225) and IPET (116094-03-1-SB010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, J., Ha Quang Bao, T., Shin, YK. et al. Antifungal activity of magnoflorine against Candida strains. World J Microbiol Biotechnol 34, 167 (2018). https://doi.org/10.1007/s11274-018-2549-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11274-018-2549-x