Abstract
Nasal natural killer (NK)/T-cell lymphoma is a peculiar lymphoma with an unique immunophenotype. Etiologically, the authors previously first demonstrated the presence of Epstein–Barr virus (EBV) genomes and their products in this lymphoma (Lancet 1990; 335). It is suggested that some of sequence variations such as a 30-bp deletion and multiple base substitutions and as amino acid changes at HLA-A2 restricted CTL epitopes were associated with an increase in tumorigenicity and with a decrease in immune recognition. In this study, we determined full-length of LMP1 sequence isolated from 7 patients with nasal NK/T-cell lymphoma using polymerase chain reaction (PCR) method and compared the sequences with those referred to previous reports. In the carboxyl-terminal site, all 7 patients showed 4 copies of the 11 amino acids repeat (codon 254–302) and 30-bp deletion corresponding to codon 343–352 of the B95-8 strain. Within the NF-kB-activating domains, all 7 patients showed amino acid changes at codon 189 (Gln to Pro), 192 (Ser to Thr) and 212 (Gly to Ser) on either site of the PXQXT (codon 204–208) motif. In the major HLA-A2 restricted T-cell epitope sequence YLLEMLWRL (codon 125–133), all 7 patients showed amino acid changes at codon 126 (Leu to Phe) and 129 (Met to Ile). In the epitopes ALLVLYSFA (codon 51–59), VLFIFGCLL (codon 110–118) and WLLLFLAIL (codon 173–181), several patients showed novel amino acid changes at codon 59 (Ala to Gly), 110 (Val to Leu) and 174 (Leu to Ile), respectively. Although it is still not clear what the most specific and biologic variation of LMP1 gene in nasal NK/T-cell lymphoma is, the sequence data may be valuable on the study for pathogenesis of nasal NK/T-cell lymphoma and EBV molecular epidemiology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nasal natural killer (NK)/T-cell lymphoma, previously called lethal midline granuloma [1], shows peculiar clinical and histological features characterized by a poor prognosis and progressive necrotic lesions with tumor and inflammatory cell infiltrations in the nasal cavity, nasopharynx, and palate [2–4]. Histologic features of the disease, displayed by angiocentric and polymorphous lymphoreticular infiltrates, have been called polymorphic reticulosis [5]. Recent articles suggest that this lymphoma may be derived from NK- or ϒδT-cell lineage, which express the NK-cell marker, CD56 [3, 6–8]. With regard to etiologic factors, the authors first demonstrated Epstein–Barr virus (EBV) genetic DNA and EBV-oncogenic proteins [9]. After that, a large number of the articles were published for association of EBV with this disease. Clonotypic EBV genome has been detected in this lymphoma, suggesting that EBV may play a role in the lymphomagenesis [3, 10]. Same as nasopharyngeal carcinoma (NPC) and Hodgkin’s disease, the overall pattern of EBV latent gene expression in nasal NK/T cell lymphoma is of latency II with transcription of Qp-initiated EBV nuclear antigen (EBNA)-1, latent membrane protein (LMP)-1, -2A and -2B, untranslated EBV-encoded small RNAs (EBERs) and a transcript containing the BamHI-A rightward open reading frame (BARF0) [3, 10–12].
LMP1 is an integral membrane protein with 6 transmembranous domains that consist of a 63-kDa protein of 386 amino acids and three regions including the amino terminus (codon 1–24), transmembrane region (codon 25–186), and carboxyl terminus (codon 187–386) [13]. It co-localizes in patches in the plasma membranes of EBV-transformed B-lymphoblastoid cell lines [13]. The sequence in the terminus–terminus influences cell growth, differentiation and apoptosis by interacting with the tumor necrosis factor receptor-associated signaling factors and the NF-kB family of transcriptional regulators [14–16]. A number of gene mutation analyses in the terminus–terminus sequence of the LMP1 gene has been performed in several EBV-associated malignancies NPC, Hodgkin’s disease, and gastric carcinoma [17–22]. In isolates from such EBV-associated malignancies, a 30-bp deletion (nt 168, 287–168, 256) corresponding to 10 amino acid deletion (aa 346–355), loss of XhoI site in amino terminus, and multiple base substitutions in the coding region were reported [13, 17–21, 23, 24].
Transmembrane domains of LMP1 contain major HLA-A2 restricted epitopes of cytotoxic T-cells (CTL). Recently, Duraiswamy et al. [25] reported seven LMP1 sequences encoding CTL epitope from healthy virus carriers. They found no difference in the sequence variations between isolates from NPC and spontaneous EBV-transformed lymphoblastoid cell lines (LCLs). On the other hand, Edwards et al. [26] performed sequence analysis of the full-length LMP1 variants from NPC lines and detected amino acid changes in many of the known and computer-predicted HLA-restricted epitopes with changes in key positions in multiple, potential epitopes for the specific HLA of the patients. Lin et al. [20] found amino acid change at 126 (Leu to Phe) in NPC at statistically significant rate 91% (20 of 22 samples) as compared to 67% (12 of 18 samples) of normal nasopharyngeal specimens, and that the 129 (Met to Ile) was observed in all samples regardless of whether they were NPC or control. They also demonstrated that the changes in this epitope sequence (codon 125–133) between NPC and normal nasopharyngeal specimens, including mutation and deletion, were statistically significant. These amino acid substitutions at key positions in the LMP1 epitopes may result in a reduced CTL response in NPC.
There are a number of reports regarding full-length of LMP1 sequence from NPC. Several novel variants of LMP1 sequence are detected in NPC [20, 23, 24]. With regard to nasal NK/T-cell lymphoma, there were several reports of LMP1 sequence regarding 30-bp deletion and pleomorphism within the carboxyl-terminus from Japan, Hong Kong, Taiwan, Korea and Malaysia [11, 27–30], but there was no information regarding full-length of LMP1 sequence. In this study, we determined full-length of LMP1 sequence isolated from 7 patients with nasal NK/T-cell lymphoma and compared the sequences with those referred to previous reports. The purpose of this study was to investigate whether certain sequence variations of LMP1 strains are associated with this lymphoma through reduced immune recognition and also through differences in molecular and biologic properties.
Materials and methods
Patients
The study group consisted of 7 Japanese patients (2 females and 5 males) with nasal NK/T-cell lymphoma. Age of patients ranged from 36 to 74 years with median age of 42 years. All patients fulfilled the diagnosis criteria of nasal NK/T-cell lymphoma following morphological, phenotypical and clinical characteristics described by Jaffe [4]. Histological findings corresponded to that of polymorphic reticulosis or angiocentric lymphoma: diffuse infiltrates of pleomorphic large lymphoid cells and atypical small lymphoid cells with a number of inflammatory cells, ischemic necrosis, and angiocentric and/or angioinvasive lesions. Phenotypically, NK cell marker CD56 with pan-T cell makers CD43 was determined in lymphoma cells from all patients. The primary sites involved nasal and/or midline tissues. EBER-1 was detected in lymphoma cells from all patients by in situ hybridization [3].
Polymerase chain reaction (PCR)
Total DNA extracted from fresh frozen material of diagnostic biopsies from all cases by using QIAamp DNA mini kit (QIAGEN K.K., Tokyo, Japan). DNA samples (1.0 μl) was diluted into 100 μl of a solution containing deoxynucleotides triphosphate (dNTP), 1.5 mM MgCl2, 500 nM each primers, 0.625 U Taq DNA polymerase (Promega, Madison, WI), and PCR reaction buffer provided by the manufacture. The DNA samples were then subjected to 35 cycles of PCR in a thermal cycler. Each cycle consisted of denaturation for 1 min at 94°C, annealing for 45 s at 45°C, and extension for 1 min at 72°C. Full details of the sequences and genome coordinates of primers are given in Table 1. For DNA amplification of LMP1 gene, a pair of primer (1S and 1E) was used. The PCR products were purified by a commercial kit (QIAquick PCR purification kit; QIAGEN K.K.) and then analyzed by electrophoresis through 3% agarose gel.
DNA sequencing
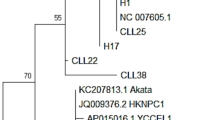
Determination of LMP1 gene sequence was achieved using a fluorescent-based dideoxy sequencing method according to a BigDye Terminator Cycle Sequencing Ready Reaction Kit (Perkin–Elmer) and an automated DNA sequencing system (ABI 310; Applied Biosystems) using four primers, 1S, 1MS, 1ME and 1E (Table 1). The sequences of the PCR-amplified products were compared with the prototype B95-8 strain (EMBL database) [31] and classified based on multiple alignment program CLUSTAL W [32]. All sequence reactions were performed on 2 independent PCR procedures.
Results
General sequence characteristics of the LMP1 gene from nasal NK/T-cell lymphoma
Nucleotide substitutions were determined with reference to B95-8 prototype LMP1 sequence. The results are summarized in Table 2. In total, 52 nucleotide substitutions were identified in 49 codons of LMP1 sequences encoding whole region isolated from 7 patients with nasal NK/T-cell lymphoma, resulting in 32 amino acid changes. Of these 52 nucleotide substitutions, forty were common in all 7 patients, resulting in 22 amino acid changes; 3 amino acid changes (codon 3, 13 and 17) were in N-terminus cytoplasmic domain, 12 (codon 25, 46, 82, 84, 85, 106, 122, 126, 129, 144, 150 and 151) were in transmembrane domains and 7 (codon 189, 192, 212, 309, 334, 338 and 366) were in C-terminal cytoplasmic domain. The remaining 12 nucleotide substitutions were varied among patients, resulted in 10 amino acid changes; 5 amino acid changes were in transmembrane domains (codon 59, 69, 110, 174 and 178) and the other 5 were in C-terminal cytoplasmic domains (codon 322, 326, 328, 329 and 335). Aside from amino acid changes at codon 322, in which 2 and 3 nucleotide substitutions were detected among 7 patients, all were single-nucleotide substitutions. When compared 7 isolates of LMP1 sequences from each patient, two identical sequences (patients 1 and 2, patients 4 and 5) were found, resulting in 5 different strains according to sequence variations.
Sequence alternations in the XhoI polymorphic site
A unique polymorphism in an XhoI restriction site in exon 1 of the LMP-1 coding region of the B95-8 strain was detected previously in EBV isolated from Chinese and Taiwanese NPC [23, 24]. The same change G to T at position 169425 in codon 17, which results in the loss of the XhoI cut site, was present consistently in all 7 patients.
Sequence alternations in the carboxyl-terminus site
In the NF-kB-activating region CTAR-1 (codon 194–232) [33], the amino acid change at codon 212 (Gly to Ser) was observed in all 7 patients. In the NF-kB-activating region CTAR-2 (codon 351–386) [33], a 30-bp deletion at codon 346–355 corresponding to 10 amino acids deletion and amino acid change at codon 366 (Ser to Thr) was detected in all patients. In the CTAR-3 domain (codon 275–330) [34], the deletion of 5 amino acids was observed at codons 275–280, resulting in 4 repeats of 11-amino acids at codons 254–302 in all 7 patients. The amino acid changes at codon 309 (Ser to Asn), 322 (Gln to Asn) and 326 (Glu to Gln), were found in all, 6 (86%) and 3 (43%) of 7 patients, respectively. In addition, the amino acid change at codon 322 (Gln to Thr), 328 (Glu to Asp) and 329 (Asn to His) were detected in each one patient. In the other sites of CTAR regions, the amino acid changes at codon 189 (Gln to Pro), 192 (Ser to Thr) and 335 (Gly to Asp) were found in all and 2 (29%) of 7 patients, respectively.
Sequence alternations in the HLA A2-restricted epitopes
Nucleotide and deduced amino acid sequences of the HLA A2-restricted epitopes (codon 32–181) within LMP1 that were previously reported were compared to those of the B95-8 strain (Table 3) [20, 25, 26, 35]. There was no amino acid change on the epitopes LLLALLFWL (codon 32–40), LLLIALWNL (codon 92–100), ILLIIALYLQQNWWTL (codon 152–167) and LLVDLLWLL (codon 167–175), in all 7 patients. In the epitope YLLEMLWRL (codon 125–133) that was identified as the major HLA-A2 restricted CTL epitope [36], two amino acid changes Leu to Phe and Met to Ile were found at codon 126 and 129, respectively in all 7 patients. Similarly, all 7 patients had amino acid changes Ala to Gly at codon 59 in the epitope VLYSFALML (codon 54–62), Ile to Leu at codon 122, Leu to Phe at 126 and Met to Ile at 129 in the epitopes LVLGIWIYL (codon 118–126) and YLLEMLWRL (codon 125–133). Two patients (patient 1 and 2) had amino acid changes Ala to Gly at codon 59 in the epitope ALLVLYSFA (codon 51–59) and Val to Leu at codon 110 in the epitope VLFIFGCLL (codon 110–118). In the epitope WLLLFLAIL (codon 173–181), four patients (patient 4, 5, 6 and 7) had amino acid changes Leu to Met at codon 178 and only patient 7 had another amino acid change Leu to Ile at codon 174.
Discussion
It is very interesting whether EBV-carrying malignancies are infected with particularly oncogenic EBV strains. Widespread prevalence of LMP-1 sequence variations, particularly the XhoI polymorphism [20, 23, 24] and the 30-bp deletion [18, 37, 38], indicates that they cannot be used as simple markers for oncogenic viruses that are related to particular forms of EBV-associated tumors. It is necessary to analyze sequence variations in other parts of LMP1, especially in regions that are related to its biological function and to CTL epitopes. It is not clear which changes in such regions are associated with the XhoI polymorphism or the 30-bp deletion. Therefore, it is important to analyze the full-length of LMP1 sequence. There is a number of reports regarding full-length of LMP1 sequence from NPC. Several novel variants of LMP1 sequence are detected in NPC [20, 23, 24]. With regard to nasal NK/T-cell lymphoma, there were several reports of LMP1 sequence regarding 30-bp deletion and pleomorphism within the carboxyl-terminus [11, 27–30], but there was no information regarding full-length of LMP1 sequence. This is first report to analyze the full-length of LMP1 sequence in nasal NK/T-cell lymphoma, particularly focusing on known functional domains and the HLA A2-restricted epitopes. The paper presents new information for the variations of LMP1 gene on nasal NK/T-cell lymphoma in Japan.
In the XhoI restriction site, all patients with nasal NK/T-cell lymphoma showed nucleotide change G to T at 169425 resulting in the loss of the XhoI cut site. Such XhoI polymorphism was previously demonstrated in Chinese and Taiwanese NPC [23, 24]. Recently, Lin et al. [20] demonstrated that the loss of the XhoI cut site was detected in 21 (96%) of 22 NPC samples, but was 12 (67%) of 18 normal nasopharyngeal tissues from Taiwan. These data suggest that the LMP1 strain with loss of the XhoI cut site may be selected in nasal NK/T-cell lymphoma as well as NPC.
Previous reports have shown the presence of a varying copy of an 11 amino acids repeat between codon 254 and 302 in the terminal domain of LMP-1. In this study, we found that all patients with nasal NK/T-cell lymphomas showed 4 copies of the repeated sequences. In Chinese population including NPC and normal nasopharyngeal tissues, the number of repeated sequence varies from 3 to 7 and do not correlate with disease status [20]. It is possible that the identical copy number found in nasal NK/T-cell lymphoma may be specific for the disease. Further information regarding the copy number of normal Japanese population and of nasal NK/T-cell lymphoma from the other geographic area will be necessary.
Within the two NF-kB-activating domains, two critical motifs have been identified that bind the tumor necrosis receptor-associated factors TRAF and TRADD. The PXQXT motif at codon 204–208, which directly binds the TRAFs 1, 2, 3, and 5 [14] and induces epidermal growth factor receptor expression [16], was unchanged in all patients with nasal NK/T-cell lymphoma. The PXQXS motif at codon 379–383, which binds the TRADD adapter protein, was conserved also in all patients. The mutations of sequence in these motifs impair both TRAF-binding and NF-kB-activating functions [15]. The conservation of sequence in these motifs suggest that the EBV strains from nasal NK/T-cell lymphoma may have a LMP1 function for TRAF signaling, as similar to isolates from NPC [19, 20]. On the other hand, sequence changes on either site of the PXQXT motif were observed at codon 189 (Gln to Pro), 192 (Ser to Thr) and 212 (Gly to Ser) in all isolates from nasal NK/T-cell lymphoma. These amino acid changes are reported to be more frequently in NPC than in normal pharyngeal tissues [20]. It is possible that amino acid changes around these critical motifs may enhance the LMP1 functions for TRAF-binding and/or NF-kB-activation and may play a role for tumorigenesis in nasal NK/T-cell lymphoma and NPC.
A deletion variant of LMP1 gene (del-LMP1) corresponding to codon 343–352 of the B95-8 strain was detected in lymphoma tissues from all patients with nasal NK/T-cell lymphoma. Suzumiya et al. [27] identified also del-LMP1 strain in all 14 nasal NK/T-cell lymphomas from Japan. Besides from Japan, a high prevalence rate of del-LMP1 strain in nasal NK/T-cell lymphoma was reported also from Hong Kong 91% (21 of 23 patients) [11], Taiwan 86% (19 of 22 patients) [28], Korea 92% (12 of 13 patients) [29] and Malaysia 100% (19 of 19 patients) [30]. Initially, a high prevalence rate of del-LMP1 strain was shown in NPC and lymphomas from eastern Asia [17, 18] and in EBV-related gastric cancer from Japan [22]. In this endemic area including Japan, normal population showed a relative high prevalence of the deletion variant [17, 18, 22, 39]. On the other hand, wild-LMP1 strain was more prominent than del-LMP1 variants in European Hodgkin’s disease and in African and New Guinean Burkitt’s lymphoma [40, 41], corresponding to the relative high prevalence of the wild-LMP1 strain in the normal population. On the basis of these findings, some investigators suggested that the high prevalence of the del-LMP1 strain represents a geographic or race-associated polymorphism rather than disease-associated polymorphism [41, 42]. However, most majority of previous reports regarding LMP1 sequence employed spontaneously established lymphoblastoid cell lines (LCLs) from healthy EBV-carries as a source of normal populations [17, 18, 40–42]. LMP1 variants have been shown to differ among the blood, throat washes and tumor tissue in NPC and Hodgkin’s disease [19, 43, 44]. The use of LCLs may be inherent bias of the assay in selecting for the dominant or more transforming virus strains.
Recently, some studies reported a significantly higher association of the del-LMP1 strain in NPC, Hodgkin’s lymphoma and nasal NK/T-cell lymphoma when compared to normal tissue samples [26, 45–47]. Kim and Peh [45] reported significantly higher prevalence of the del-LMP1 strain in malignant lymphomas (91%) as compared with reactive lymphoid tissue [60%]. Tan et al. [46] reported that the del-LMP1 strain was associated with 84% of NPC, whereas the strain was carried in only 8% of the normal postnasal space biopsies. Recently, using a heteroduplex-tracking assay (HTA) that can distinguish all of the LMP1 variants, Edwards et al. [26] analyzed differences on EBV strains between NPC samples and the matching blood samples of same patients from both southern China where NPC is endemic and northern China where NPC is not endemic. They found that the del-LMP1 strain (Ch1 strain) is most frequently detected in the NPC samples from the both regions and the B95-8 strain is also prevalent in peripheral blood samples from southern China. In the majority of samples from this region, a single different strain was detected in the NPC and peripheral blood samples, whereas multiple LMP1 variants were detected in the peripheral blood samples from northern China [26]. These data suggested that the single del-LMP1 strain (Ch1 strain) was specifically selected within NPC among various LMP1 variants. With regard to nasal NK/T-cell lymphoma, Chiang et al. [47] reported that the del-LMP1 strain was found in 91% of tumor tissues of patients with nasal NK/T-cell lymphomas and 63% in normal nasal tissues from healthy donor in Taiwan. Although we did not analyze LMP1 variants in the normal nasal tissues or peripheral blood from Japanese population, the prevalence of del-LMP1 strain in Japan is reported to be 74% (14 of 19) of healthy and nonmalignant EBV-associated diseases [39] and 84% (15 of 18) of throat washings from healthy adults [22]. In nasal NK/T-cell lymphoma from Japan, it was 100% (all of 7 in our series and all of 14 in series of Suzumiya [27]). It is suggested, on the basis of the data, that the del-LMP1 strain may be selected within tumors and play a role for lymphomagenesis in nasal NK/T-cell lymphoma.
A number of HLA-restricted CTL epitopes has been identified or predicted in LMP1. Recently, several reports showed that several amino acid changes of HLA A2-restricted CTL epitopes within LMP1 sequence were detected in not only NPC specimens but also control samples [20, 25, 26]. Among these epitopes, the sequence YLLEMLWRL (codon 125–133) was the major HLA-A2 restricted CTL epitope sequence divergence. In this study, all isolates from nasal NK/T-cell lymphoma showed amino acid changes at codon 126 (Leu to Phe) and 129 (Met to Ile) in this sequence. Lin et al. [20] found that the same amino acid change at codon 126 (Leu to Phe) was detected in NPC at statistically significant rate 91% (20 of 22 samples) as compared to 67% (12 of 18 samples) of normal nasopharyngeal specimens, and that the amino acid change at codon 129 (Met to Ile) was observed in all samples regardless of whether they were NPC or control. They also demonstrated that the changes in this epitope sequence (codon 125–133) between NPC and normal nasopharyngeal specimens, including mutation and deletion, were statistically significant. Antigenic analysis indicated that this variant sequence (YFLEILWRL) was not only poorly recognized by epitope-specific CTL but also showed significant loss in HLA A2 binding compared to the B95-8 sequence [25]. Pandya and Walling [48] showed that the amino acid change at codon 129 (Met to Ile) increased the LMP1 half-life in epithelial cells. It is likely that the variant sequence at codon 125–133 (YFLEILWRL) may be selected in nasal NK/T-cell lymphoma as well as NPC and may play important roles in reduced recognition of CTL and/or in lymphomagenesis.
Aside from the epitope YLLEMLWRL (codon 125–133), several amino acid changes of HLA A2-restrcted CTL epitopes were observed in several patients. The LMP1 sequences from 4 patients contained amino acid change at 178 (Leu to Met) in the epitope WLLLFLAIL (codon 173–181). Since the same amino acid was observed equally in NPC (59%) and control specimens (50%) [20], the amino acid change at codon 178 (Leu to Met) is not likely selected in nasal NK/T-cell lymphoma. On the other hand, the remaining 3 amino acid changes at codon 59 (Ala to Gly), 110 (Val to Leu) and 174 (Leu to Ile) in the epitope ALLVLYSFA (codon 51–59), VLFIFGCLL (codon 110–118) and WLLLFLAIL (codon 173–181) respectively were not reported previously. It is possible that these novel amino acid changes may be selected in a part of nasal NK/T-cell lymphomas.
In summary, we first reported the full length of LMP1 sequence from nasal NK/T-cell lymphoma. In the XhoI restriction site, all 7 patients showed nucleotide change G to T at 169425 resulting in the loss of the XhoI cut site. In the terminal–terminal site, all 7 patients showed 4 copies of the 11 amino acids repeat (codon 254–302) and 30-bp deletion corresponding to codon 343–352 of the B95-8 strain. Within the NF-kB-activating domains, all 7 patients showed amino acid changes at codon 189 (Gln to Pro), 192 (Ser to Thr) and 212 (Gly to Ser) on either site of the PXQXT (codon 204–208) motif. In the major HLA-A2 restricted T-cell epitope sequence YLLEMLWRL (codon 125–133), all 7 patients showed amino acid changes at codon 126 (Leu to Phe) and 129 (Met to Ile). In the epitopes ALLVLYSFA (codon 51–59), VLFIFGCLL (codon 110–118) and WLLLFLAIL (codon 173–181), several patients showed novel amino acid changes at codon 59 (Ala to Gly), 110 (Val to Leu) and 174 (Leu to Ile), respectively. Since control and biological analyses could not be performed, it is still not clear what the most specific and biologic variation of LMP1 gene in nasal NK/T-cell lymphoma is. However, our present data provide new information for the variations of LMP1 gene on nasal NK/T-cell lymphoma in Japan and may be valuable on the study for pathogenesis of the lymphoma and EBV molecular epidemiology. Further comparative studies including either the healthy tissue of the same patient or from different healthy donors and biological analyses of such LMP1 variants will be necessary.
References
G.S. Spear, W.G. Walker, Bull Johns Hopkins Hosp 99, 313–332 (1956)
N. Yamanaka, A. Kataura, S. Sambe, T. Minase, Y. Ishii, Ann Otol Rhinol Laryngol 94, 207–211 (1985)
Y. Harabuchi, S. Imai, J. Wakashima, M. Hirao, A. Kataura, T. Osato, S. Kon, Cancer 77, 2137–2149 (1996)
E.S. Jaffe, J.K. Chan, I.J. Su, G. Frizzera, S. Mori, A.C. Feller, F.C. Ho, Am J Surg Pathol 20, 103–111 (1996)
B.S. Eichel, E.G. Harrison Jr., K.D. Devine, P.W. Scanlon, H.A. Brown, Am J Surg 112, 597–605 (1966)
A.K. Chiang, A.C. Chan, G. Srivastava, F.C. Ho, Int J Cancer 73, 332–338 (1997)
B. Arnulf, C. Copie-Bergman, M.H. Delfau-Larue, A. Lavergne-Slove, J. Bosq, J. Wechsler, M. Wassef, C. Matuchansky, B. Epardeau, M. Stern, M. Bagot, F. Reyes, P. Gaulard, Blood 91, 1723–1731 (1998)
H. Nagata, A. Konno, N. Kimura, Y. Zhang, M. Kimura, A. Demachi, T. Sekine, K. Yamamoto, N. Shimizu, Blood 97, 708–713 (2001)
Y. Harabuchi, N. Yamanaka, A. Kataura, S. Imai, T. Kinoshita, F. Mizuno, T. Osato, Lancet 335, 128–130 (1990)
J. Minarovits, L.F. Hu, S. Imai, Y. Harabuchi, A. Kataura, S. Minarovits-Kormuta, T. Osato, G. Klein, J Gen Virol 75(Pt 1), 77–84 (1994)
A.K. Chiang, Q. Tao, G. Srivastava, F.C. Ho, Int J Cancer 68, 285–290 (1996)
van J. Gorp, A. Brink, J.J. Oudejans, van den A.J. Brule, van den J.G. Tweel, N.M. Jiwa, de P.C. Bruin, C.J. Meijer, J Clin Pathol 49, 72–76 (1996)
W.E. Miller, R.H. Edwards, D.M. Walling, N. Raab-Traub, J Gen Virol 75, 2729–2740 (1994)
G. Mosialos, M. Birkenbach, R. Yalamanchili, T. Van Arsdale, C. Ware, E. Kieff, Cell 80, 389–399 (1995)
O. Devergne, E. Hatzivassiliou, K.M. Izumi, K.M. Kaye, M.F. Kleijnen, E. Kieff, G. Mosialos, Mol Cell Biol 16, 7098–7108 (1996)
W.E. Miller, G. Mosialos, E. Kieff, N. Raab-Traub, J Virol 71, 586–594 (1997)
H. Knecht, F. Martius, E. Bachmann, T. Hoffman, D.R. Zimmermann, S. Rothenberger, K. Sandvej, W. Wegmann, H. Hurwitz, B.F. Odermatt, et al., Leukemia 9, 458–465 (1995)
C.L. Chen, M.M. Hsu, H.C. Hsu, Intervirology 39, 230–235 (1996)
R.H. Edwards, F. Seillier-Moiseiwitsch, N. Raab-Traub, Virology 261, 79–95 (1999)
J.C. Lin, J.M. Cherng, H.J. Lin, C.W. Tsang, Y.X. Liu, S.P. Lee, J Gen Virol 85, 2023–2034 (2004)
H. Knecht, E. Bachmann, P. Brousset, K. Sandvej, D. Nadal, F. Bachmann, B.F. Odermatt, G. Delsol, G. Pallesen, Blood 82, 2937–2942 (1993)
S. Mori, T. Itoh, M. Tokunaga, Y. Eizuru, J Med Virol 57, 152–158 (1999)
L.F. Hu, E.R. Zabarovsky, F. Chen, S.L. Cao, I. Ernberg, G. Klein, G. Winberg, J Gen Virol 72, 2399–2409 (1991)
M.L. Chen, C.N. Tsai, C.L. Liang, C.H. Shu, C.R. Huang, D. Sulitzeanu, S.T. Liu, Y.S. Chang, Oncogene 7, 2131–2140 (1992)
J. Duraiswamy, J.M. Burrows, M. Bharadwaj, S.R. Burrows, L. Cooper, N. Pimtanothai, R. Khanna, J Virol 77, 7401–7410 (2003)
R.H. Edwards, D. Sitki-Green, D.T. Moore, N. Raab-Traub, J Virol 78, 868–881 (2004)
J. Suzumiya, K. Ohshima, M. Takeshita, M. Kanda, C. Kawasaki, N. Kimura, K. Tamura, M. Kikuchi, Leuk Lymphoma 35, 567–578 (1999)
T.T. Kuo, L.Y. Shih, N.M. Tsang, Int J Surg Pathol 12, 375–387 (2004)
J.E. Kim, Y.A. Kim, Y.K. Jeon, S.S. Park, D.S. Heo, C.W. Kim, Pathol Int 53, 735–743 (2003)
Y.C. Tai, L.H. Kim, S.C. Peh, Pathol Int 54, 158–166 (2004)
R. Baer, A.T. Bankier, M.D. Biggin, P.L. Deininger, P.J. Farrell, T.J. Gibson, G. Hatfull, G.S. Hudson, S.C. Satchwell, C. Seguin, et al., Nature 310, 207–211 (1984)
J.D. Thompson, D.G. Higgins, T.J. Gibson, Nucleic Acids Res 22, 4673–4680 (1994)
D.S. Huen, S.A. Henderson, D. Croom-Carter, M. Rowe, Oncogene 10, 549–560 (1995)
O. Gires, F. Kohlhuber, E. Kilger, M. Baumann, A. Kieser, C. Kaiser, R. Zeidler, B. Scheffer, M. Ueffing, W. Hammerschmidt, Embo J 18, 3064–3073 (1999)
K.C. Parker, M.A. Bednarek, J.E. Coligan, J Immunol 152, 163–175 (1994)
R. Khanna, S.R. Burrows, J. Nicholls, L.M. Poulsen, Eur J Immunol 28, 451–458 (1998)
H. Knecht, E. Bachmann, P. Brousset, S. Rothenberger, H. Einsele, V.S. Lestou, G. Delsol, F. Bachmann, P.F. Ambros, B.F. Odermatt, Oncogene 10, 523–528 (1995)
C. Berger, C. McQuain, J.L. Sullivan, D. Nadal, P.J. Quesenberry, H. Knecht, J Infect Dis 176, 1370–1373 (1997)
O. Itakura, S. Yamada, M. Narita, H. Kikuta, Oncogene 13, 1549–1553 (1996)
F. Khanim, Q.Y. Yao, G. Niedobitek, S. Sihota, A.B. Rickinson, L.S. Young, Blood 88, 3491–3501 (1996)
X.S. Zhang, K.H. Song, H.Q. Mai, W.H. Jia, B.J. Feng, J.C. Xia, R.H. Zhang, L.X. Huang, X.J. Yu, Q.S. Feng, P. Huang, J.J. Chen, Y.X. Zeng, Cancer Lett 176, 65–73 (2002)
M. D’Addario, P. Chauvin, Mutat Res 457, 69–78 (2000)
S. Henry, C. Sacaze, L. Berrajah, H. Karray, M. Drira, A. Hammami, J. Icart, B. Mariame, Int J Cancer 91, 698–704 (2001)
F. Meggetto, P. Brousset, J. Selves, G. Delsol, B. Mariame, J Virol 71, 2547–2549 (1997)
L.H. Kim, S.C. Peh, J Clin Exp Hematopathol 43, 11–19 (2003)
E.L. Tan, S.C. Peh, C.K. Sam, J Med Virol 69, 251–257 (2003)
A.K. Chiang, K.Y. Wong, A.C. Liang, G. Srivastava, Int J Cancer 80, 356–364 (1999)
J. Pandya, D.M. Walling, J Virol 78, 8404–8410 (2004)
Acknowledgement
This work was supported in part by a Grant-in-Aid 1739455 from the Ministry of Education, Science, Sports, Culture and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nagamine, M., Takahara, M., Kishibe, K. et al. Sequence variations of Epstein–Barr virus LMP1 gene in nasal NK/T-cell lymphoma. Virus Genes 34, 47–54 (2007). https://doi.org/10.1007/s11262-006-0008-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11262-006-0008-5