Abstract
Background
Although methicillin-resistant Staphylococcus aureus (MRSA) nasal colonization is common among end-stage kidney disease patients undergoing haemodialysis, few studies were focused on MRSA nasal carriers among haemodialysis patients with central venous catheters (CVCs). The aim of this study is to evaluate the risk factors, various clinical outcomes and effect of decolonization for MRSA nasal colonization among patients on haemodialysis via CVCs.
Methods
This was a single-centre non-concurrent cohort study of 676 patients who had new haemodialysis CVCs inserted. They were all screened for MRSA colonization via nasal swabs and were categorized into two groups: MRSA carriers and MRSA noncarriers. Potential risk factors and clinical outcomes were analysed in both groups. All MRSA carriers were given decolonization therapy and the effect of decolonization on subsequent MRSA infection was also performed.
Results
Eighty-two patients (12.1%) were MRSA carriers. Multivariate analysis showed that MRSA carrier (OR 5.44; 95% CI 3.02–9.79), long-term care facility resident (OR 4.08; 95% CI 2.07–8.05), history of Staphylococcus aureus infection (OR 3.20; 95% CI 1.42–7.20) and CVC in situ > 21 days (OR 2.12; 95% CI 1.15–3.93) were independent risk factors for MRSA infection. There was no significant difference in all-cause mortality between MRSA carriers and noncarriers. The MRSA infection rates were similar between MRSA carriers with successful decolonization and those who had failed/incomplete decolonization in our subgroup analysis.
Conclusion
MRSA nasal colonization is an important cause of MRSA infection among haemodialysis patients with CVCs. However, decolonization therapy may not be effective in reducing MRSA infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among patients with end-stage kidney disease (ESKD), Staphylococcus aureus (S. aureus) infections often lead to multiple complications associated with high costs and prolonged hospitalization [1]. S. aureus has become increasingly resistant to antibiotics, such as methicillin-resistant S. aureus (MRSA), which is a prevalent nosocomial pathogen nowadays. There is an increased risk of MRSA infection and/or colonization in patients with ESKD due to frequent attendance in healthcare settings, immunocompromised status, and exposure to prolonged antibiotics [2, 3]. Among dialysis patients in the USA, the incidence of invasive MRSA infection was found to be 100 times higher than in the general population [4].
MRSA nasal carriage is a predominant risk factor for subsequent MRSA infection [5]. In chronic haemodialysis patients, nasal carriage of MRSA has been associated with a 2.46-fold increase in all-cause mortality [6]. In view of the high prevalence of MRSA and the heavy burden on the healthcare system, there have been recommendations for active surveillance for MRSA colonization, though the effectiveness is still controversial [7].
Patients who have a central venous catheter (CVC) are at higher risk for bloodstream infections than those with other forms of access. In the North American cohort, the bloodstream infection rate for patients with permanent CVCs was 4.2 per 100 patient months, compared with 0.9 and 0.5 per 100 patient months, respectively, for arteriovenous grafts and fistulas [8]. Although there were studies of MRSA nasal colonization in patients with ESKD [9,10,11], the majority of these patients used arteriovenous grafts or fistulas as their vascular access for haemodialysis. There have been no similar studies that solely focus on CVCs. A better understanding of MRSA epidemiology and the associated risk factors is important for planning strategies to improve patients’ outcomes in this vulnerable population.
We hypothesized that a higher MRSA-related infection risk will be found in MRSA nasal carriers compared with MRSA noncarriers among haemodialysis patients with CVCs. The aim of our study is to examine whether active surveillance of MRSA nasal carriage in haemodialysis patients with CVCs could predict higher MRSA-related infection risks. Moreover, the MRSA nasal carriage rates among haemodialysis patients with CVCs, risk factors of MRSA infection and the effectiveness of decolonization therapy are also studied.
Materials and methods
This non-concurrent cohort study was conducted in Queen Elizabeth Hospital (QEH), one of the largest acute hospitals in Hong Kong SAR with approximately 2000 beds, serving approximately 15% of our 7.5 million population. All patients, aged 18 or above, who had a new haemodialysis CVC inserted in QEH between 1st January 2016 and 31st December 2018 were recruited. Those receiving haemodialysis via arteriovenous fistulas or grafts were excluded. All patients were identified by the Clinical Data Analysis and Reporting System (CDARS) of the Hospital Authority, Hong Kong. The baseline demographic and clinical data were collected from patient’s medical records. Potential risk factors for MRSA infection [3, 12,13,14] were analysed in all patients.
Care of the vascular access and catheter site was based on our local guideline [15]. Patients were followed-up for any MRSA-related infection within one year from the date of CVC insertion or until death, whichever was earlier. For purpose of studying mortality, patients were censored on 31st December 2020. The primary outcome was MRSA-related infection in 1 year. The secondary outcome included all-cause mortality and the effect of decolonization therapy. The event rate of MRSA-related infection and all-cause mortality were compared between MRSA carriers and noncarriers. The rate of MRSA-related infection was also analysed between MRSA carriers who had successful decolonization versus incomplete or failed decolonization.
MRSA screening
All patients receiving haemodialysis for any reason had nasal swab for MRSA screening performed on the day of CVC insertion. Nasal swab was obtained from both anterior nares using sterile saline moistened swab and sent to the microbiology laboratory for MRSA culture. The results would be available approximately 5 days later. For those who had more than one CVC insertion during the period, only the data on the first CVC were analysed. Patients were categorized into MRSA carriers or MRSA noncarriers. MRSA carriers were defined as any patients with nasal swab done at first screening growing MRSA. All the others were defined as MRSA noncarriers.
Decolonization therapy
After confirmation of MRSA nasal colonization, patients were given a routine course of decolonization therapy. Our decolonization regime included 2% mupirocin to nasal cavities three times a day for 5 days, and body and hair wash with 2% chlorhexidine for 5 days [16]. Instruction sheets with illustrative pictures were given. After decolonization, nasal swab culture was repeated twice on different dates and at least 48 h apart to confirm effectiveness. Successful decolonization was defined as two consecutive MRSA-negative nasal swabs. If initial decolonization failed, a second course of decolonization was performed with a nasal swab to be repeated as above afterwards. No further decolonization was necessary if the nasal swab still remained positive for MRSA after the second course of decolonization therapy.
Statistical analysis
The statistical analyses were performed by SPSS (SPSS 27, Inc., Chicago, IL USA). Categorical data were expressed as percentages and continuous data were expressed as mean ± standard deviation (SD) or median (25th, 75th percentile). Categorical data were compared with chi-square or Fisher’s exact tests while continuous data were compared with t test or Mann–Whitney U test. Kaplan–Meier estimates and log-rank test were used to demonstrate event rate during follow-up and all-cause mortality. Cox proportional hazard model was used to assess the effect of MRSA carriage on the study end points. All tests were 2-tailed, and differences for p values of less than 0.05 were considered significant. Potential risk factors were first assessed in univariate analysis. The multivariable model was developed in a forward, stepwise fashion. Candidate variables were those with p < 0.1 in univariate analysis.
Results
Total of 676 patients were recruited into this study. The mean age was 63.4 ± 14.4 (range 18–94) years. There were 402 men (59.5%) and 347 diabetic patients (51.3%). Fifty-five patients (8.1%) were long-term care facilities (LTCF) residents, and 100 patients (14.8%) had ICU admission in the previous three months. Five hundred and seventy-two patients (84.6%) were dialyzed through a temporary uncuffed CVC, while the remaining 104 patients (15.4%) were dialyzed through a tunnelled cuffed CVC. Five hundred and twenty-four (77.5%) of the CVCs were at the jugular region, while the rest of 152 (22.5%) CVCs were at the femoral site. There were 431 (63.8%) incident haemodialysis patients, with indications including acute kidney injury and uraemia or fluid overload in ESKD; 170 (25.1%) patients were previously on peritoneal dialysis and then started on haemodialysis due to failed peritoneal dialysis, such as refractory peritonitis requiring removal of peritoneal dialysis catheters, leakage of peritoneal fluid through pleuro-peritoneal fistula or hernias, or intra-abdominal surgeries; 67 (9.9%) patients received a new CVC insertion as their previous haemodialysis access failed, such as thrombosed or stenotic arteriovenous fistulas or grafts requiring intervention; the remaining 8 (1.2%) patients had a new CVC inserted for both plasmapheresis and haemodialysis.
MRSA carriers and decolonization rates
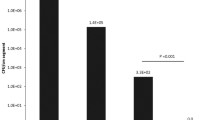
Among the 676 patients, 82 (12.1%) were MRSA carriers. Baseline characteristics of the MRSA carriers and MRSA noncarriers were shown in Table 1. There were significantly more male patients in MRSA carriers, more MRSA carriers being LTCF residents compared with noncarriers, and more MRSA carriers having recent ICU admission in the last three months than noncarriers. Seventy-five MRSA carriers (91.5%) received their first course of decolonization therapy; while 7 carriers did not receive any decolonization therapy, as they were either transferred to another hospital where the protocol for MRSA decolonization was not implemented, or they died before screening results or decolonization therapy was available. These 7 patients were classified as having incomplete decolonization. Out of the 75 carriers who received the first course of decolonization therapy, 60 of them had MRSA cleared afterwards, while 15 patients still had a positive MRSA nasal swab. These 15 patients then underwent a second course of decolonization therapy—12 had MRSA cleared, while 3 still had persistent positive MRSA nasal carriage and were defined as failed decolonization. Thus the successful decolonization rate in our cohort is 96% (72/75) (Fig. 1).
MRSA infection
MRSA infection occurred in 69 patients (Table 2). MRSA carriers had a significantly higher rate of MRSA infection when compared with noncarriers (31.7% vs 7.2%, p < 0.01). There was a significantly higher rate of MRSA bloodstream infections among MRSA carriers than noncarriers (11% vs 3.2%, p < 0.01). The median number of days to first MRSA infection was shorter in MRSA carriers (64 days; 25th percentile 18 days, 75th percentile 115 days) than in noncarriers (95 days; 25th percentile 29 days, 75th percentile 169 days, p = 0.15). Other types of MRSA infection including haemodialysis CVC exit site, soft tissue, peritoneal dialysis catheter exit site, lung, peritonitis or urinary tract occurred more frequently in MRSA carriers but were not statistically significant.
The significant risk factors for MRSA infection include MRSA carrier (odds ratio [OR] 5.95; 95% confidence interval [CI] 3.40–10.41), residing in LTCF (OR 5.44; 95% CI 2.89–10.23), history of S. aureus infection (either methicillin-sensitive or resistant) within the previous year (OR 2.86; 95% CI 1.34–6.07), CVC in situ > 21 days (OR 2.30; 95% CI 1.29–4.12) and cuffed haemodialysis catheters (OR 2.14; 95% CI 1.19–3.83) (Table 3). Multivariate logistic regression analysis showed that MRSA carrier (OR 5.44; 95% CI 3.02–9.97, p < 0.01), LTCF resident (OR 4.08; 95% CI 2.07–8.05, p < 0.01), history of S. aureus infection in the previous year (OR 3.20; 95% CI 1.42–7.20, p < 0.01) and CVC in situ > 21 days (OR 2.12; 95% CI 1.15–3.93, p = 0.02) were the four independent risk factors for MRSA infection (Table 4).
Since there was a significantly higher portion of LTCF in the MRSA carrier group, this group might already have more MRSA infection by its nature and the results would be skewed. If LTCF residents were excluded and the results were re-analyzed, MRSA carrier was still a significant risk factor for MRSA infection (OR 8.17, 95% CI 4.33–15.42, p < 0.01).
All-cause mortality
Total of 346 (51.2%) patients died during the study period. Among them, 46 were MRSA carriers, whereas 300 were MRSA noncarriers. There was no statistically significant difference in all-cause mortality between MRSA carriers and noncarriers (p = 0.13).
Subgroup analysis between successfully decolonized MRSA carriers and carriers who had failed or incomplete decolonization
Further subgroup analysis was performed to compare the outcome of MRSA infection between MRSA carriers who were successfully decolonized and those who had failed or incomplete decolonization (Table 5). Twenty-three out of 72 (31.9%) successfully decolonized MRSA carriers had MRSA infection within one year, which is similar to 3 out of 10 (30%) MRSA carriers who had failed or incomplete decolonization. Regarding haemodialysis CVC exit site MRSA infections, there were 2 (2.7%) among the successfully decolonized group but there were none among the other group. There were 6 (8.3%) successfully decolonized MRSA carriers who had MRSA bloodstream infection, compared with 3 (30%) of the failed or incompletely decolonized group. All these findings were not statistically significant.
Discussion
Patients with ESKD have an increased risk for MRSA colonization and infection, especially those undergoing dialysis [3, 13, 17]. A study in Singapore reported the prevalence of MRSA colonization in hospitalized chronic haemodialysis patients at 15.1%, which is threefold higher than the prevalence of MRSA colonization among all inpatients (5.8%) [18]. Johnson et al. found an MRSA colonization rate of 21.7% among dialysis patients, compared with 8.3% among the general population [19]. The MRSA nasal colonization rate in our cohort was 12.1%, which was similar to the reported rates of 10% in the United Kingdom and 15.1% in Singapore; but lower than 27.3% among an American Indian population [18, 20, 21]. The variation in rates of colonization could be due to geographical and ethnic differences which was described by Ray et al. [22]. A possible reason behind the lower rate of MRSA nasal colonization in our cohort, when compared to other countries, could be that more than half of our patients were new to dialysis, whereas the majority of the population in other studies were on chronic haemodialysis, who might have more frequent hospital attendances with increased risk of MRSA exposure.
In our study, MRSA nasal colonization was an independent risk factor for subsequent MRSA infection for patients on haemodialysis with CVC. Neilsen J et al. reported S. aureus nasal carriage was a sensitive method to predict S. aureus septicaemia among haemodialysis patients on CVC, with a negative predictive value (NPV) of 90%, which was just second to positive S. aureus culture from the insertion site (NPV 98%) [23]. MRSA nasal carriers were 5.4 times more likely to develop MRSA infection than noncarriers within one year of screening. Our finding is in concordance with the literature, which reported a higher S. aureus infection rate in nasal carriers on haemodialysis than noncarriers, with relative risks ranging from 1.8 to 4.7 [9,10,11]. It has been proposed that the nose acts as a reservoir for S. aureus, which then propagates to the skin and causes subsequent infection in patients with impaired skin sites, such as patients on haemodialysis with CVCs.
Another independent risk factor for MRSA infection from our study was LTCF residents. They were 4 times more likely to have MRSA infection within one year in our study. In fact, other studies in Hong Kong reported that LTCF residents contributed to half of the MRSA carriers among hospitalized patients older than 65 [24]. A study in Germany observed that staying in LTCF for more than 6 months was a risk factor for MRSA colonization [25]. Reasons behind the high MRSA colonization rates in LTCF residents were host-related: advanced age, poor functional status, multiple co-morbidities, indwelling invasive devices, decubitus ulcers, prior hospitalizations and antibiotic therapy; and environment-related: size and density of LTCF and location of LTCF in a deprived area.
Similar to other studies [14, 26], patients with a history of S. aureus infection were also an independent risk factor for MRSA infections in our cohort. This could be due to patient’s previous exposure to S. aureus which led to increased risks of colonization and thus subsequent infection; also patients might have been hospitalized for previous S. aureus infection which increased the chances of colonization. Our study observed a higher risk of MRSA infection with the use of cuffed tunnelled haemodialysis catheters compared with temporary uncuffed haemodialysis catheters. Possible reasons could be that our patients who received temporary uncuffed haemodialysis catheters might have switched to peritoneal dialysis afterwards, or that they have renal recovery, thus there was a reduced need to return to the hospital regularly and this minimised the risk of MRSA exposure.
Among dialysis patients, mupirocin is highly effective in the eradication of S. aureus nasal carriage [27,28,29]. A systematic review and meta-analysis found an MRSA decolonization success rate of 0.88 (95% CI 0.75–0.95) among haemodialysis patients [30]. Boelaert et al. reported a nasal S. aureus eradication rate of 96.3% by nasal mupirocin among surveillance cultures done on haemodialysis patients [31]. This was similar to our successful decolonization rate of 96%. On the contrary, evidence on the effect of eradication of MRSA nasal carriage by intranasal mupirocin on the reduction of infection rate among haemodialysis patients has been controversial. Despite a high successful decolonization rate, there were still significantly higher rates of MRSA infection and bloodstream infections among our MRSA carriers, who, in fact, had been decolonized after being screened positive. Possible reasons behind this include that MRSA screening and decolonization were only performed once during the insertion of CVC with no interval follow-up screening after successful decolonization, so intermittent MRSA carriers could not be identified in our study, as patients might have been colonized again afterward which was not detected by our protocol; the culprit MRSA strain causing the infection might be of a different strain from that found in the nose, so nasal decolonization could not have prevented such an MRSA infection; our overall MRSA carrier cohort had included those who had failed or incomplete decolonization albeit a small population only. Further in our subgroup analysis between MRSA carriers who had been decolonized successfully and those who had failed or incomplete decolonization, there were no significant differences in MRSA infection of any sites, CVC exit site infections or bloodstream infections. This could be attributed to the inadequate power because there were only 10 MRSA carriers who had failed or incomplete decolonization. In fact, among patients other than those on dialysis, evidence of the effect of MRSA nasal eradication with mupirocin has also been inconclusive. A double-blind, randomized, placebo-controlled study recruited 614 patients receiving an orthopaedic surgical intervention who were then randomized to receive mupirocin or placebo. The mupirocin group had a significantly more effective eradication of nasal carriage (83.5%) compared with the placebo group (27.8%), but S. aureus surgical site infection rates were not reduced significantly (3.8% in the mupirocin group versus 4.7% in the placebo group) [32].
To our knowledge, this is the first study analysing the risk factors and clinical outcomes of MRSA nasal colonization solely among patients on haemodialysis via CVCs. However, there are several limitations to our study. First, the sample size of MRSA carriers was relatively small, particularly those that had failed or incomplete decolonization. This may not be able to generate adequate power to study the effectiveness of decolonization. This together with the lack of interval MRSA screening, molecular studies and genotyping of MRSA isolates may affect our study of decolonization outcome. In addition, due to the retrospective nature of the study, not all of the potential confounders could be fully adjusted, and the association identified might not imply causality. Furthermore, due to our study design where MRSA screening was performed during the insertion of a new CVC, more than half of our cohort was new to dialysis, which most of them would later be converted to peritoneal dialysis; and less than 10% of our cohort was on long term haemodialysis. Our findings could not be directly translated to the general population of chronic haemodialysis patients. Since only nasal swabs were taken for MRSA screening, the carriage rate might be underestimated. Finally, nearly all of our MRSA carriers received decolonization therapy. Our findings of clinical outcomes and mortality thus might not have reflected the direct impact of MRSA nasal colonization.
Conclusion
MRSA nasal carriage, LTCF residents, history of S. aureus infection in the previous one year and CVC in situ > 21 days were independent risk factors for MRSA infection in haemodialysis patients using CVCs. In view of the doubtful efficacy of intranasal mupirocin decolonization for preventing MRSA infection, the individual renal unit has to develop tailored strategies for active surveillance and mupirocin use. Further studies with larger sample size and the use of control groups with a placebo are necessary to confirm these outcomes and the effectiveness of decolonization.
References
Li Y, Friedman JY, O’Neal BF et al (2009) Outcomes of Staphylococcus aureus infection in haemodialysis-dependent patients. Clin J Am Soc Nephrol 4:428–434
Koziol-Montewka M, Chudnicka A, Ksiasek A, Majdan M (2001) Rate of Staphylococcus aureus nasal carriage in immunocompromised patients receiving haemodialyis treatment. Int J Antimicrob Agents 18:193–196
Lu PL, Tsai JC, Chiu YW et al (2008) Methicillin-resistant Staphylococcus aureus carriage, infection and transmission in dialysis patients, healthcare workers and their family members. Nephrol Dial Transplant 23:1659–1665
Centers for Disease Control and Prevention (2020) Healthcare-Associated Infections – Community Interface Surveillance Report, Emerging Infections Program Network, Methicillin-Resistant Staphylococcus aureus, 2017
Davis KA, Steward JJ, Crouch HK, Florez CE, Hospenthal DR (2004) Methicillin-resistant Staphylococcus aureus (MRSA) nares colonization at hospital admission and its effect on subsequent MRSA infection. Clin Infect Dis 39:776–782
Lai CF, Liao CH, Pai MF et al (2011) Nasal carriage of methicillin-resistant Staphylococcus aureus is associated with higher all-cause mortality in haemodialysis patient. Clin J Am Soc Nephrol 6:167–174
McGinigle KL, Gourlay ML, Buchanan IB (2008) The use of active surveillance cultures in adult intensive care units to reduce methicillin-resistant Staphylococcus aureus-related morbidity, mortality, and costs: a systematic review. Clin Infect Dis 46:1717–1725
Klevens RM, Edwards JR, Andrus ML, Peterson KD, Dudeck TC, Horan TC (2008) Dialysis surveillance report: National Healthcare Safety Network – Data summary for 2006. Semin Dial 21:24–28
Kluytmans JA, van Belkum A, Verbrugh H (1997) Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbio Rev 10:505–520
Yu VL, Goetz A, Wagener M et al (1986) Staphylococcus aureus nasal carriage and infection in patients on haemodialysis. Efficacy of antibiotic prophylaxis. N Engl J Med 315:91–96
Kaplowitz LG, Comstock JA, Landwehr DM, Dalton HP, Mayhall CG (1988) Prospective study of microbial colonization of the nose and skin and infection of the vascular access site in haemodialysis patients. J Clin Microbiol 26:1257–1262
Daeschlein G, Assadian O, Rangous I, Kramer A (2006) Risk factors for Staphylococcus aureus nasal carriage in residents of three nursing homes in Germany. J Hosp Infect 63:216–220
Lederer SR, Riedelsdorf G, Schiffl H (2007) Nasal carriage of meticillin resistant Staphylococcus aureus: the prevalence, patients at risk and the effect of elimination on outcomes among outclinic haemodialysis patients. Eur J Med Res 12:284–288
Hadley AC, Karchmer TB, Russell GB, McBride DG, Freedman BI (2007) The prevalence of resistant bacterial colonization in chronic hemodialysis patients. Am J Nephrol 27:352–359
Department of Health and Central Renal Committee, Hospital Authority. Infection Control Guidelines on Nephrology Services in Hong Kong 2018 (3rd edn, version 3.2). https://www.chp.gov.hk/files/pdf/ic_gu_nephrology_services_in_hk.pdf. Accessed 4 Jan 2021
Coia JE, Duckworth GJ, Edwards DI, Joint Working Party of the British Society of Antimicrobial Chemotherapy; Hospital Infection Society; Infection Control Nurses Association et al (2006) Guidelines for the control and prevention of meticillin-resistant Staphylococcus aureus (MRSA) in healthcare facilities. J Hosp Infect 63(Suppl 1):S1–S44
Centers for Disease Control (2007) Invasive methicillin-resistant Staphylococcus aureus infections among dialysis patients, United States, 2005. MMWR Morb Mortal Wkly Rep 56:197–199
Yeoh LY, Tan FL, Willis GC, Ooi ST (2014) Methicillin-resistant Staphylococcus aureus carriage in hospitalized chronic haemodialysis patients and its predisposing factors. Hemodial Int 18:142–147
Johnson LB, Jose J, Yousif F, Pawlak J, Saravolatz LD (2009) Prevalence of colonization with community-associated methicillin-resistant Staphylococcus aureus among end-stage renal disease patients and healthcare workers. Infect Control Hosp Epidemiol 30:4–8
Price A, Sarween N, Gupta I, Baharani J (2015) Meticillin-resistant Staphylococcus aureus and meticillin-susceptible Staphylococcus aureus screening in a cohort of haemodialysis patients: carriage, demographics and outcomes. Journal of Hosp Infect 90:22–27
Leman R, Alvarado-Ramy F, Pocock S et al (2004) Nasal carriage of methicillin-resistant Staphylococcus aureus in an American Indian population. Infect Control Hosp Epidemiol 25:121–125
Ray GT, Suaya JA, Baxter R (2012) Trends and characteristics of culture-confirmed Staphylococcus aureus infections in a large U.S. integrated health care organization. J Clin Microbiol 50:1950–1957
Nielsen J, Ladefoged SD, Kolmos HJ (1998) Dialysis catheter-related septicaemia – focus on Staphylococcus aureus septicaemia. Nephrol Dial Transplant 13:2847–2852
Chuang VW, Tsang IH, Keung JP et al (2015) Infection control intervention on meticillin resistant Staphylococcus aureus transmission in residential care homes for the elderly. J Infect Prev 16:58–66
Wendt C, Svodoba D, Schmidt C, Bock-Hensley O, von Baum H (2005) Characteristics that promote transmission of Staphylococcus aureus in German nursing homes. Infect Control Hosp Epidemiol 26:816–821
Patel G, Jenkins SG, Mediavilla JR et al (2011) Clinical and molecular epidemiology of methicillin-resistant Staphylococcus aureus among patients in an ambulatory hemodialysis center. Infect Control Hosp Epidemiol 32:881–888
Kluytmans JA, Wertheim HF (2005) Nasal carriage of Staphylococcus aureus and prevention of nosocomial infections. Infection 33:3–8
Herwaldt LA (1998) Reduction of Staphylococcus aureus nasal carriage and infection in dialysis patients. J Hosp Infect 40(Suppl B):S13–S23
Laupland KB, Conly JM (2003) Treatment of Staphylococcus aureus colonization and prophylaxis for infection with topical intranasal mupirocin: an evidence-based review. Clin Infect Dis 37:933–938
Gebreselassie HM, Lo Priore E, Marschall J (2015) Effectiveness of meticillin-resistant Staphylococcus aureus decolonization in long-term haemodialysis patients: a systematic review and meta-analysis. J Hosp Infect 91:250–256
Boelaert JR, Van Landuyt HW, Godard CA et al (1993) Nasal mupirocin ointment decreases the incidence of Staphylococcus aureus bacteraemias in haemodialysis patients. Nephrol Dial Transplant 8:235–239
Kalmeijer MD, Coertjens H, van Nieuwland-Bollen E, deBaere G, Kluytmans J (2002) Surgical site infections in orthopedic surgery: the effect of mupirocin nasal ointment in a double-blind, randomized, placebo-controlled study. Clin Infect Dis 35:353–358
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the local Research Ethics Committee [REC (KC/KE)-20-0158/ER-3].
Informed consent
The requirement to obtain informed consent was waived based on the observational design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, Y.T., Yeung, C.S., Chak, W.L. et al. Methicillin-resistant Staphylococcus aureus nasal carriage among patients on haemodialysis with newly inserted central venous catheters. Int Urol Nephrol 55, 2059–2066 (2023). https://doi.org/10.1007/s11255-023-03521-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03521-4