Abstract
Purpose
Hyperuricemia has been associated with higher mortality in the general population, but less is known about CKD patients. The aim of our study was to determine the impact of elevated serum uric acid on cardiovascular mortality of CKD patients who later progress to hemodialysis.
Methods
In this retrospective study, 120 CKD patients (entire population of patients with ESKD on January 1st, 2012) were observed from their first visit at the Nephrology outpatient clinic, while transitioning to hemodialysis, and until their death or January 1, 2016. After non-cardiovascular death exclusion, 83 CKD patients (33 female, 50 male) were left for further analysis. The average time of observation was 8.8 ± 4.2 years. Serum uric acid was measured regularly (every 3 months). No patients were treated for hyperuricemia. Mean uric acid of 420 µmol/L was set as a cut-off between normouricemic and hyperuricemic patients as per the laboratory’s reference values. Survival rates were analyzed using Kaplan–Meier survival curves. Three Cox regression models were used to assess the influence of uric acid on survival.
Results
Mean uric acid was 379.8 ± 71.6 µmol/L (range 220–574). Sixty-three (75.9%) patients were normouricemic and 20 (24.1%) were hyperuricemic. Cholesterol was the only variable to show statistically significant difference (p = 0.004) between the groups. Bivariate analysis revealed an association between death and age, hyperuricemia, arterial hypertension, and history of cardiovascular disease. Kaplan–Meier survival analysis showed higher risk of cardiovascular death for hyperuricemic patients (log rank test; p < 0.0005). In Cox regression models, hyperuricemia remained a predictor of cardiovascular mortality (SE = 0.500, Exp(B) = 14.120, 95% CI 5.297–37.640) in our patients next to age and arterial hypertension.
Conclusion
The results indicate an association between hyperuricemia and cardiovascular mortality in CKD patients who transition to hemodialysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uric acid or urate is an end product of endogenous purine nucleotide or dietary purine metabolism generated by xanthine dehydrogenase or xanthine oxidase with poor solubility, circulating in plasma [1, 2]. Once created it cannot be metabolized further but must be eliminated by kidney or intestinal excretion. Herein lies the cause why approximately 50% of CKD patients already become hyperuricemic immediately prior to hemodialysis treatment (HD), as healthy kidneys eliminate about 70% of serum uric acid (SUA) [2,3,4].
One of the problems in dealing with hyperuricemia is no universally accepted definition of hyperuricemia. A practical value would seem to be SUA concentration higher than 405 µmol/L (6.8 mg/dL) as this is urate’s solubility point used for measurement in laboratories [5]. Other researchers suggest lower values down to 300 µmol/L (5 mg/dL) for healthy individuals, some suggest different values for men and women due to uricosuric effect of estrogenic compounds, while others suggest values of 360 µmol/L (6 mg/dL) that are targeted when using urate lowering therapy (ULT) [6,7,8].
It is still uncertain whether asymptomatic hyperuricemia is an independent risk factor for cardiovascular (CV) disease. The presence of comorbidities such as CKD contributes to progression of hyperuricemia, which appears to be the main cause of gout that in turn is an independent predictor of premature death. In several epidemiological and observational studies hyperuricemia has been linked to CV events, arterial hypertension (AH), and diabetes mellitus (DM), but Mendelian randomization studies do not seem to show an association [8,9,10,11,12,13]. Studies have shown that hyperuricemia predicts progression of kidney disease in various nephropathies and CKD, and that higher values of SUA and body mass index (BMI) are associated with an estimated glomerular filtration rate (eGFR) decline of ≥ 50% or end-stage kidney disease in patients with arterial/arteriolar nephrosclerosis. Furthermore, increased SUA correlates with increased intima media thickness values as markers of atherosclerosis and suboptimal blood pressure control [5, 14, 15].
In a previous study carried out in our center, we have already shown that hyperuricemia is directly associated with higher all-cause mortality of CKD patients [16]. The aim of our study was to determine the impact of elevated SUA on cardiovascular mortality of CKD patients undergoing HD during long-term follow-up.
Materials and methods
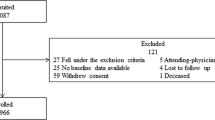
120 CKD patients (entire population of patients with end-stage kidney disease in our center on January 1st, 2012) enrolled in our study. They were observed regularly from their first visit at the patients’ Nephrology outpatient clinic (NOC) in the University Medical Centre Maribor in Slovenia. All patients later started HD and were followed until their death or January 1st, 2016 (on average for 8.8 ± 4.2 years, maximal period of observation was 19.5 years). SUA was measured regularly (every 3 months on average) from venous sampling during NOC visits and HD sessions. All patients who died of other than CV causes or had received HD for less than 3 months were excluded from the data. In the end 83 CKD patients remained for analysis (Fig. 1).
Patients with the mean SUA < 420 µmol/L (7.06 mg/dL) were defined as normouricemic, while patients with the mean SUA ≥ 420 µmol/L (7.06 mg/dL) as hyperuricemic. No patients were treated for hyperuricemia using ULT. AH was defined as an average measured blood pressure ≥ 140 mm Hg systolic or ≥ 90 mm Hg diastolic or as receiving treatment for AH. DM was defined as receiving treatment for DM.
All patients had C-reactive protein (CRP), total cholesterol, triglyceride (TG), and creatinine levels determined from their blood sample on their first NOC visit, had their BMI calculated before their first HD session, and all were questioned whether they are currently smoking or whether they had ever smoked before. Their eGFR was calculated using the Modification of Diet in Renal Disease (MDRD) equation. They were questioned about active treatment with statins, angiotensin converting enzyme inhibitors (ACEIs), or angiotensin receptor blockers (ARBs). Data about the primary CKD etiology and history of CV disease were collected from the medical database. CV disease was defined as history of coronary artery disease, heart failure, or atrial fibrillation.
Normality of data was tested using Shapiro–Wilk’s test. The groups were compared using Chi-squared test for categorical variables, Mann–Whitney U test for non-parametric variables, and T test for parametric variables. Similarly, association between researched variables and death was found using the same tests.
Survival rates were analyzed using Kaplan–Meier survival curves. Three different models were used for Cox regression analysis. First, the unadjusted Cox model using only hyperuricemia. Second, Cox model using hyperuricemia, statistically different variables between groups, and variables with statistically significant association with mortality in our cohort. Last, Cox model using variables in the second model adjusted for age, sex, BMI and eGFR. Statistical analysis was performed using SPSS for Windows, version 19.0.1 (SPSS, Chicago, IL, USA). All data are presented as mean ± SD. A relationship was considered statistically significant at p values less than 0.05.
Results
Mean age of the cohort was 56.5 ± 15.5 years, ranging from 20 to 82 years at first NOC visit. There were 33 (39.8%) women and 50 (60.2%) men. The main causes of CKD in our patients have shown to be DM, AH, and IgA glomerulonephritis (Table 1). Mean SUA was 379.8 ± 71.6 µmol/L, ranging from 220 to 574 µmol/L. Gender specific analysis showed significantly (p = 0.04) lower values of SUA for females (360.3 ± 67.7 µmol/L), as opposed to males (392.6 ± 71.8 µmol/L). Mean SUA before initiating HD was 476.1 ± 136.7 µmol/L. Significantly lower (p < 0.005) values were observed during the HD period when SUA was 352.8 ± 62.7 µmol/L. Basic characteristics of our patients are presented in Table 2. Sixty-three (75.9%) patients were normouricemic and 20 (24.1%) were hyperuricemic, out of which 21 (33.3%) normouricemic and 14 (70.0%) hyperuricemic patients died. Kaplan–Meier survival analysis showed the risk of death being higher for hyperuricemic patients (log rank test; p < 0.0005) compared to normouricemic patients (Fig. 2).
Cholesterol was the only variable to show statistically significant difference (p = 0.004) between the normo- and hyperuricemic group, 5.3 ± 1.5 mmol/l and 4.2 ± 0.9 mmol/l, respectively. Analysis showed statistically significant association with mortality for age (p = 0.001), hyperuricemia (p = 0.004), history of CV disease (p = 0.036), and AH (p = 0.039).
The unadjusted Cox regression using only hyperuricemia showed statistically significant (p < 0.005) difference in mortality between the groups (SE = 0.366, Exp(B) = 4.147, 95% CI 2.025–9.495). Second, we tested the only statistically different variable cholesterol and variables associated to mortality with hyperuricemia. The unadjusted Cox regression showed statistically significant (p < 0.0005) difference in mortality for hyperuricemia, age, and AH (Table 3). And last, with the Cox multivariable regression model following bivariate analysis adjusted for age, sex, BMI, and eGFR, hyperuricemia remained a predictor of mortality in our patients (p < 0.0005) (Table 4).
Discussion
Hyperuricemia has shown to be directly associated with higher CV mortality in our cohort of patients. Other studies show conflicting results. Some researchers have shown that CKD patients with heart failure and higher SUA have a poorer prognosis compared to normouricemic patients and that SUA has a J-shaped relationship with all-cause mortality [17, 18], while others have shown that hyperuricemia and higher SUA were associated with lower risk of all-cause and CV mortality in the hemodialysis population [19, 20]. In patients without CKD, elevated SUA showed an increased risk for development of chronic kidney dysfunction and those who received ULT had potentially better survival than those who did not [21, 22].
The mean BMI of enrolled patients was 27.2 kg/m2 which falls into the pre-obesity category according to the World Health Organization. A former study carried out in our centre showed that about 60% of HD patients are abdominally obese and have higher risk for CV mortality due to microinflammation [23]. This could point towards a possible explanation of raised CV mortality of our hyperuricemic patients, as raised SUA in patients with CKD has been reported to induce oxidative stress and inflammation as well as inducing endothelial disfunction by decreasing nitric oxide bioavailability [3, 5, 6, 24, 25].
As atherosclerosis is one of the main causes of CV morbidity and mortality, and could be associated with hyperuricemia in all patients, future research in this area could also benefit from use of non-invasive tools for cardiovascular assessment such as pulse wave analysis and pulse wave velocity. A study has shown that higher SUA was associated with a greater increase in pulse wave velocity, pointing towards arterial stiffness in patients with SUA ≥ 370 µmol/L (6.2 mg/dL), which is more frequently reached in men [6, 26].
Interestingly, AH showed to be a protective factor in our cohort of patients. We believe this is due to a small number of patients (three patients) that died soon after initialization of HD or were relatively hypotensive during individual HD sessions. A lot of patients were categorized as hypertensive, because the main treatment of CKD is regulation of hypertension and treatment with ACEIs or ARBs. Studies indicate that hypertension mediates the annual decline of eGFR that is larger in patients with hyperuricemia [27].
TG have achieved pathologic values in 57% of our patients. Postorino et al. have observed a reduced all-cause and CV mortality in patients with 0.5 mmol/L (50 mg/dL) of excess TG and waist circumference < 95 cm. Recent studies have also shown that CV risk factors such as weight, blood pressure and cholesterol seem to have a U-shape association with CV mortality in CKD patients undergoing HD [28, 29].
The main strengths of our study are the use of an average of SUA measurements, that were collected regularly through follow-up, the length of follow-up, which was on average almost 9 years per patient, and observing patients who transitioned from NOC visits into HD.
Regardless, our study has some limitations. The group of enrolled patients was small, so our results should be reviewed on a larger group of CKD patients. We have also not considered some medications that could affect SUA levels, such as fibrates, diuretics, or estrogenic compounds. Additionally, we have not searched and tested for mineral and bone disorder parameters related to CKD such as parathyroid hormone, serum calcium, and phosphate levels.
Despite several epidemiological and Mendelian randomization studies that show conflicting results, large randomized placebo-controlled studies should be carried out to assess the benefit of treating asymptomatic hyperuricemia in CKD patients. In the meantime, physicians should consider managing hyperuricemic patients’ therapy to medications known to lower SUA as a secondary effect, such as losartan, atorvastatine, and calcium channel blockers and think about reducing the cut-off value for hyperuricemia to lower values, but stay cautious as some research in patients on chronic HD showed higher risk for all-cause mortality, when SUA is lower than 330 µmol/L (5.5 mg/dL) [6, 11, 30].
Conclusion
The results indicate an association between SUA and CV mortality in CKD patients undergoing HD during long-term follow-up and show that hyperuricemia and age are directly associated with higher CV mortality of our patients.
References
Prasad Sah OS, Qing YX (2015) Associations between hyperuricemia and chronic kidney disease: a review. Nephrourol Mon. 7:e27233
Hyndman D, Liu S, Miner JN (2016) Urate handling in the human body. Curr Rheumatol Rep 18(6):34
Johnson RJ, Nakagawa T, Jalal D, Sánchez-Lozada LG, Kang DH, Ritz E (2013) Uric acid and chronic kidney disease: which is chasing which? Nephrol Dial Transplant 28:2221–2228
Ohno I (2011) Relationship Between Hyperuricemia and Chronic Kidney Disease. Nucleosides Nucleotides Nucleic Acids 30:1039–1044
Mallat SG, Al Kattar S, Tanios BY, Jurjus A (2016) Hyperuricemia, hypertension, and chronic kidney disease: an emerging association. Curr Hypertens Rep 18(10):74
Ferri C (2017) The problem of cardio-renal diseases in patients with gout. Curr Med Res Opin 33(sup3):9–13
Ramirez MEG, Bargman JM (2017) Treatment of asymptomatic hyperuricemia in chronic kidney disease: a new target in an old enemy—a review. J Adv Res. 8(5):551–554
Bardin T, Richette P (2014) Definition of hyperuricemia and gouty conditions. Curr Opin Rheumatol 26(2):186–191
Abeles AM (2015) Hyperuricemia, gout, and cardiovascular disease: an update. Curr Rheumatol Rep 17(3):13
Karis E, Crittenden DB, Pillinger MH (2014) Hyperuricemia, gout, and related comorbidities: cause and effect on a two-way street. South Med J 107(4):235–241
Bardin T, Richette P (2017) Impact of comorbidities on gout and hyperuricemia: an update on prevalence and treatment options. BMC Med. 15:123
Butkovič M (2016) Urate as a potential risk factor of cardiovascular and renal diseases. Acta Med Croatica. 70:233–239
Nashar K, Fried LF (2012) Hyperuricemia and the progression of chronic kidney disease: is uric acid a marker or an independent risk Factor? Adv Chronic Kidney Dis. 19:386–391
Momoki K, Kataoka H, Moriyama T, Mochizuki T, Nitta K (2017) Hyperuricemia as a predictive marker for progression of nephrosclerosis: clinical assessment of prognostic factors in biopsy-proven arterial/arteriolar nephrosclerosis. J Atheroscler Thromb. 24(6):630–642
Buzas R, Tautu OF, Dorobantu M, Ivan V, Lighezan D (2018) Serum uric acid and arterial hypertension-Data from Sephar III survey. PLoS ONE 13(7):e0199865
Petreski T, Bevc S, Ekart R, Hojs R (2017) Hyperuricemia and long-term survival in patients with chronic kidney disease undergoing hemodialysis. Clin Nephrol 88(13):69–72
Okazaki H, Shirakabe A, Kobayashi N, Hata N, Shinada T, Matsushita M et al (2016) The prognostic impact of uric acid in patients with severely decompensated acute heart failure. J Cardiol 68(5):384–391
Srivastava A, Kaze AD, McMullan CJ, Isakova T, Waikar SS (2018) Uric acid and the risks of kidney failure and death in individuals with CKD. Am J Kidney Dis 71(3):362–370
Latif W, Karaboyas A, Tong L, Winchester JF, Arrington CJ, Pisoni RL et al (2011) Uric acid levels and all-cause and cardiovascular mortality in the hemodialysis population. Clin J Am Soc Nephrol 6(10):2470–2477
Kim CS, Jin DC, Yun YC, Bae EH, Ma SK, Kim SW (2017) Relationship between serum uric acid and mortality among hemodialysis patients: retrospective analysis of Korean end-stage renal disease registry data. Kidney Res Clin Pract. 36(4):368–376
Li L, Yang C, Zhao Y, Zeng X, Liu F, Fu P (2014) Is hyperuricemia an independent risk factor for new-onset chronic kidney disease?: a systematic review and meta-analysis based on observational cohort studies. BMC Nephrol. 15:122–134
Chen JH, Lan JL, Cheng CF, Liang WM, Lin HY, Tsay GJ (2015) Effect of urate-lowering therapy on all-cause and cardiovascular mortality in hyperuricemic patients without gout: a case-matched cohort Study. PLoS ONE 10(12):e0145193
Bevc S, Zorman T, Purg D, Ekart R, Hojs R (2013) Cardiovascular mortality and microinflammation in abdominal obese hemodialysis patients. Acta Medico-Biotechnica. 6(2):39–46
Li M, Li X, Liu Y, Liu X, Song Y, Zhao J et al (2018) Relationship between serum bilirubin levels s and the progression of renal function in patients with chronic kidney disease and hyperuricemia. Clin Chim Acta 486:156–161
Sánchez-Lozada LG, Soto V, Tapia E, Avila-Casado C, Sautin YY, Nakagawa T et al (2008) Role of oxidative stress in the renal abnormalities induced by experimental hyperuricemia. Am J Physiol Renal Physiol 295(4):F1134–F1141
Piko N, Ekart R, Bevc S, Hojs R (2017) Atherosclerosis, epigenetic modifications, and arterial stiffness. Acta Medico-Biotechnica. 10(2):10–17
Sedaghat S, Hoorn EJ, van Rooij FJ, Hofman A, Franco OH, Witteman JC et al (2013) Serum uric acid and chronic kidney disease: the role of hypertension. PLoS ONE 8(11):e76827
Postorino M, Marino C, Tripepi G, Zoccali C (2011) Abdominal obesity modifies the risk of hypertriglyceridemia for all-cause and cardiovascular mortality in hemodialysis patients. Kidney Int 79(7):765–772
Gregg LP, Hedavati SS (2018) Management of traditional cardiovascular risk factors in CKD: what are the data? Am J Kidney Dis. https://doi.org/10.1053/j.ajkd.2017.12.007
Bae E, Cho HJ, Shin N, Kim SM, Yang SH, Kim DK (2016) Lower serum uric acid level predicts mortality in dialysis patients. Medicine 95(24):e3701
Acknowledgements
We would like to acknowledge and thank our colleagues at the Dept. of Nephrology and Dept. of Dialysis for their devoted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the Slovenian National Medical Ethics Committee, which approved the protocols in this study (Approval No. 41/12/12), and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Petreski, T., Ekart, R., Hojs, R. et al. Asymptomatic hyperuricemia and cardiovascular mortality in patients with chronic kidney disease who progress to hemodialysis. Int Urol Nephrol 51, 1013–1018 (2019). https://doi.org/10.1007/s11255-019-02154-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02154-w