Abstract
Purpose
Detrusor underactivity (DU) is frequently encountered in elderly patients. Part of patients with DU might have bladder function recovery after treatment. This study investigated urinary proteins in these DU patients with and without bladder function recovery.
Methods
A total of 37 patients with chronic urinary retention and urodynamically proven DU were enrolled. After treatment, 24 DU patients had bladder function recovery whereas 13 had not, after 1-year follow-up. Urine collection at baseline was performed, and the urinary protein including nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF) and prostaglandin E2 (PGE2) were measured by ELISA. Twenty urodynamically normal, 34 detrusor overactivity (DO) and 15 detrusor hyperactivity and inadequate contractility (DHIC) patients served as comparative groups.
Results
Urinary NGF levels were significantly higher than normal in patients with DU (9.2 ± 20.3 vs 1.85 ± 2.9 pg/ml, p = 0.037). Urinary BDNF level was only significantly higher in patients with DU than that of the control group (153 ± 199 vs 77.4 ± 47.7 pg/ml, p = 0.033) but not in patients with DHIC or DO. Compared with the control group, the urinary BDNF level was significantly higher in DU patients with bladder function recovery (190 ± 239 pg/ml, p = 0.033) but not in patients without recovery (85.8 ± 43.7 pg/ml, p = 0.612). The PGE2 level was significantly higher than the control group in DU patients with bladder function recovery (1290 ± 836 pg/ml, p < 0.0001) but not in patients without recovery (383 ± 237 pg/ml, p = 0.130).
Conclusion
Patients with DU and higher urinary PGE2 and BDNF levels might have a chance to recover bladder function than those with a lower protein level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic urinary retention is a debilitating bladder disorder that causes great negative impact of the quality of life (QoL) as well as healthy threatening. The pathophysiology of chronic urinary retention may involve neurogenic, myogenic and bladder outlet pathologies [1]. There are many unexplored pathophysiology in the research needs for detrusor underactivity (DU).
Patients with DU usually void with abdominal straining, and intermittent flow pattern is noted. The bladder sensation may be normal or reduced in sensing first sensation or urge sensation [2]. Part of the patients with DU may have both detrusor hyperactivity and inadequate contractility (DHIC) [3]. DU is a common urological problem in the elderly patients presenting with urinary retention and lower urinary tract symptoms (LUTS) [4]. DU usually occurs in patients with spinal cord injury (SCI), multiple system atrophy, multiple sclerosis, cervical/thoracic tumors, lumbar spondylosis and ischemic stroke [5, 6]. DU is also common in patients with old age, general weakness and with medical diseases such as diabetes mellitus, debilitating disease, cancer patients at terminal stage or post-major surgery [7].
Although DU is highly prevalent in the elderly patients, in clinical practice, we have observed DU patients who regained spontaneous voiding after indwelling catheter for a period of time or after transurethral resection of the prostate (TURP) within 1–3 months. However, some patients might develop chronic DU and spontaneous voiding may not return in short-term. There must have been some underlying pathogenesis for the development of transient DU, such as detrusor muscle damage or neurological inhibition which interfere the integration of musculo-mucosal mechanoreceptors, mucosal mechanoreceptors and chemoreceptors [8, 9].
The pathogenesis of DU is likely to be multifactorial1. DU may be classified as myogenic or neurogenic mechanism [10]. The causes of DU include DM, BOO, aging, neurological diseases, spinal cord lesions, pelvic plexus and infectious neurologic problems [9]. Underactive bladder can result from damage of the bladder afferent pathways, bladder efferent pathways, lumbosacral spinal cord or pure detrusor failure [11]. There is a need to develop screening tools for the longitudinal change in bladder function in DU patients.
Urinary nerve growth factor (NGF), brain-derived neurotrophic factor (BDNF) and prostaglandin E2 (PGF2) have been widely investigated in patients with overactive bladder (OAB) [12,13,14,15,16]. Although the results are still controversial, the tendency that these three proteins in the urine are closely associated with the severity of OAB and urodynamic detrusor overactivity (DO) in both idiopathic and neurogenic OAB [17, 18]. Because these proteins are secreted by the urothelium and detrusor, they might also have changes in patients with DU. Therefore, we might be able to predict the recovery of bladder function in patients with clinical DU by the change in some proteins in the urine. This study investigated the urinary NGF, BDNF and PGE2 in patients with DU with and without bladder function recovery and attempted to find out possible biomarker that provided prognostic value for the bladder function recovery.
Materials and methods
Urine samples were collected from patients with urodynamically proven DU, DO, DHIC and normal tracing. All patients underwent videourodynamic study for lower urinary tract symptoms. The procedure and terminology of urodynamic study was in accordance with the recommendations of International Continence Society [19]. Patients with DU were diagnosed based on the urodynamic findings of reduced bladder sensation, low Pdet, unsustained detrusor contraction, low Qmax and large PVR. After the study, they were invited to participate in this study. The study was approved by the Institutional Review Board and Ethics Committee of Buddhist Tzu Chi General Hospital (IRB: 105-142-B). Each patient was informed about the study rationale and procedures, and written informed consent was obtained before enrolling into the study. The experimental methods were carried out in accordance with the relevant guidelines and regulations.
The etiology of patients with DO, DHIC and DU varied. Among patients with DO, 17 (50%) had bladder outlet obstruction, the others were idiopathic DO. Patients with DU and DHIC had multiple medical diseases including diabetes mellitus, chronic renal failure, congestive heart failure, chronic debilitating diseases and previous TURP. Patients with overt neuropathy causing detrusor acontractile (including cerebrovascular accident, spinal cord injury, multiple sclerosis, and Parkinson disease), BOO with chronic urinary retention or acute urinary tract infection were not included in this study. All DU patients were admitted for treatment of the chronic urinary retention or large PVR, including urethral onabotulinumtoxinA injection, transurethral incision of the bladder neck or prostate. Urine sample was obtained for this study.
Patients were requested to provide a 30 ml urine sample at a full bladder in the morning. Voided urine was put on ice immediately and transferred to the laboratory for preparation. The samples were centrifuged at 3000 rpm for 10 min at 4 °C. The supernatant is separated into aliquots in 1.5 ml tubes and preserved in a freezer at −80 °C. At the same time, 3 mL of urine is taken to measure the urinary creatinine level
NGF and BDNF concentrations were determined using the immunoassay system for NGF (Wuhan EIAab Science Co., Ltd, Wuhan, China) and BDNF (BioVision, CA, USA) with a specific and highly sensitive ELISA kit, which had a minimum sensitivity of 7.8 pg/ml. Assays were performed according to the manufacturer’s instructions. Briefly, NGF or BDNF levels were detected using an antibody sandwich format in 96-well plates. Each well was initially coated with 100 μl of anti-NGF or anti-BDNF polyclonal antibody and incubated overnight at 4 °C, followed by a 1-h incubation with blocking buffer to prevent nonspecific binding. Either 100 μl of urine or 100 μl of NGF or BDNF standards (0–250 pg/ml) was added to each well followed by incubation for 6 h at room temperature with shaking. Then, the plate was washed, anti-NGF or anti-BDNF monoclonal antibody was added, and the plate was incubated at 4 °C for 14–18 h. After the plate had been washed, the amount of bound monoclonal antibody was detected using IgG horseradish peroxidase-conjugated antibody as a tertiary reactant. The unbound conjugate was removed by washing, and the plate was then incubated with 100 μl TMB (3,3′5,5′ tetramethylbenzydine) substrate solution for 10 min at room temperature. Hydrochloric acid (1 N 100 μl) was added to terminate the reactions. Color change was measured with a Synergy HT microplate reader (Bio-Tek Instruments) at 450 nm. The amount of NGF or BDNF in each urine sample was determined from a standard curve. All samples were run in triplicate, and the values were averaged.
Urinary PGE2 was measured using a high-sensitivity ELISA kit (Cayman, MI, USA), according to manufacturer’s instructions. Briefly, calibrator diluent buffer was added to antibody precoated plates at the zero standard (B0, 100 μl) and nonspecific binding (150 μl) wells. Then, 100 μl of high-sensitivity PGE2 standards (19.6–1250 pg/ml) and three-times diluted urine samples were pipetted into the remaining wells. Standards and all samples were assayed as a triple repeat. The concentration of PGE2 was determined by measuring the absorbance with a microplate reader (SynergyTM, HT Bio-Tek Instruments, Vermont, USA) at 450 and 540 nm.
The data were presented primarily as the means and standard deviation (SD) of the values. Group differences were tested by nonparametric Mann–Whitney U test. Differences of urodynamic parameters and urinary NGF, BDNF and PGE2 levels among normal, DO, DHIC and DU groups were compared. The urodynamic parameters and urinary protein levels were further compared between DU patients with and without bladder function recovery. All analyses were conducted using SPSS for Windows (version 12, SPSS, Chicago, IL). Two-sided p value of <0.05 was taken as significant.
Results
A total of 106 patients were enrolled in this study, including 37 with DU, 34 with DO, 15 DHIC and 20 normal tracing. The age and gender distribution are listed in Table 1. The age of patients with DHIC was significantly older than the other groups. Among patients with DU, 17 had chronic urinary retention and the others had large PVR requiring indwelling Foley catheter or clean intermittent catheterization.
As expected, patients with DO had earlier perception of bladder fullness, urgency sensation and bladder capacity, higher Pdet and smaller PVR than patients with DHIC and DU. Patients with DHIC and DU had similar volume of bladder sensation and capacity, Qmax, voided volume and PVR; however, Pdet was significantly lower in patients with DU than DHIC (Table 1). When we divided patients with DU into bladder function recovery and non-recovery group, there was no significant difference in the baseline urodynamic parameters between groups (Table 2).
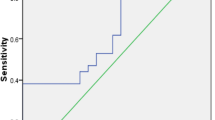
Urinary NGF levels were significantly higher than normal in patients with DU (9.2 ± 20.3 vs 1.85 ± 2.9 pg/ml, p = 0.037) and DHIC (10.3 ± 16.1 vs 1.85 ± 2.9 pg/ml, p = 0.028), but not reached a significant level in patients with DO (6.1 ± 13.5 vs 1.85 ± 2.9 pg/ml, p = 0.086) (Table 1). The NGF level was not significantly higher in patients with and without bladder function recovery, compare with that in the control group (7.85 ± 14.57 and 11.7 ± 28.5 vs 1.85 ± 2.9 pg/ml, p = 0.06 and 0.239, respectively). However, there was also no significant difference between these two DU groups (p = 0.589) or compared with patients with DHIC or DO (p = 0.738) (Fig. 1; Table 3).
Urinary BDNF level was only significantly higher in patients with DU than that of the control group (153 ± 199 vs 77.4 ± 47.7 pg/ml, p = 0.033) but not in patients with DHIC (99.1 ± 109 vs 77.4 ± 47.7 pg/ml, p = 0.432) or DO (97.7 ± 88.6 vs 77.4 ± 47.7 pg/ml, p = 0.348) (Table 1). The urinary BDNF level was significantly higher in DU patients with bladder function recovery (190 ± 239 pg/ml, p = 0.033) but not in patients without recovery (85.8 ± 43.7 pg/ml, p = 0.612) compared with that in the control group. BDNF level was also significantly higher in DU patients with bladder function recovery than patients without recovery (p = 0.048) (Fig. 2). The BDNF levels were not significantly different among patients with DHIC, DO and DU with and without bladder function recovery (p = 0.072) (Table 3).
Urinary brain-derived neurotrophic factor (BDNF) levels in patients with detrusor overactivity (DO), detrusor hyperactivity and inadequate contractility (DHIC), detrusor underactivity (DU) with bladder function recovery and DU with non-recovery, and controls. The data are expressed as mean ± standard error
Compared with that in the control group, the urinary PGE2 levels were significantly higher in patients with DU (971 ± 811 vs 525 ± 269 pg/ml, p = 0.004) and DHIC (992 ± 607 vs 525 ± 269 pg/ml, p = 0.004), but not in patients with DO (741 ± 597 vs 525 ± 269 pg/ml, p = 0.076) (Table 1). The PGE2 level was significantly higher than the control group in DU patients with bladder function recovery (1290 ± 836 pg/ml, p < 0.001) but not in patients without recovery (383 ± 237 pg/ml, p = 0.130). The PGE2 level was also significantly higher in DU patients with bladder function recovery than DO patients (p = 0.020) but not than DHIC patients (p = 0.575) (Fig. 3; Table 3).
Discussion
Evidence have shown that urinary proteins such as NGF, BDNF and PGE2 levels increase in patients with OAB and might serve as prognostic biomarkers of severity of disease or prognostic biomarkers for treatment outcome [18, 21, 22]. This study revealed that the baseline urinary PGE2 and BDNF levels, but not NGF level, were significantly higher in patients with DU and bladder function recovery after treatment, but remained low in patients without bladder function recovery. To our knowledge, this is the first study to investigate the urinary protein levels in patients with DU with and without bladder function recovery.
Because the pathophysiology of DU is multifactorial, it is possible that the bladder urothelial dysfunction, sensory nerve dysfunction, detrusor myogenic dysfunction, as well as the impaired central nervous system control are involved, in part or totally, in the development of DU [1]. Searching for the changes of urinary proteins might provide understanding the pathophysiology of DU in individual patient and will be the mainstay of appropriate management especially as prognostic biomarkers for the potential recoverability of bladder function.
Urinary NGF and BDNF have been considered as surrogate biomarkers for the diagnostic or treatment outcome of OAB [22]. However, recent researches did not consistently find the same results in OAB patients with refractory urgency urinary incontinence and brain lesion [18, 23]. The wide variability of urinary protein concentrations might result from different investigating test agents, methodology, urine collection, and most likely, the heterogeneity of the disease. Nevertheless, NGF and BDNF are believed to represent master modulation of neural plasticity in systemic or lower urinary tract dysfunction causing sensory pathway remodeling, resulting in excessive sensory activation of the micturition circuit [24].
In this study, we found urinary NGF levels were significantly increased in patients with DU and DHIC and marginally elevated in patients with DO. However, no significant difference of urinary NGF level was noted between DU patients with and without bladder function recovery. Nerve growth factor is important for the development and maintenance of the sympathetic and sensory nervous systems. NGF stimulates division and differentiation of sympathetic and embryonic sensory neurons and may increase secretion in different disease conditions through different mechanism. Therefore, although urinary NGF level can increase in DO, it will also increase when there is a need for nerve regeneration such as in DHIC or DU. However, because in human study, the subjects are rather heterogeneous and the urinary NGF levels are not consistently elevated.
Although NGF is associated with nerve regeneration, this protein might not act as a biomarker to predict bladder function recovery in DU bladders. Interestingly, we found urinary BDNF level was significantly elevated in patients with DU but not in DHIC and DO. The urinary BDNF level in DU patients with bladder function recovery was significantly higher than that in the control group and patients without recovery. These results suggest that urinary BDNF might be a better biomarker to predict bladder function recovery in patients with DU. Urinary NGF and BDNF have been found closely associated with the severity of OAB and urodynamic DO [17]. Increase in urinary BDNF levels not only reflects the increase in protein secretion under pathological conditions, but also is seen in part of DU patients with bladder function recovery, suggesting a process of nerve regeneration is undergoing.
PGE2 is well known to play an important role in detrusor contractility [25]. PGE2 intravesical infusion induced bladder overactivity in mice, which was abolished in EP3 receptor knockout mice [26]. Increased PGE2 production was found in bladders with urothelial injury, bladder outlet obstruction and overactive bladder in men and women [13, 27,28,29]. Antimuscarinic therapy can suppress the increase in PGE2 secretion from the urothelium induced by distention of rat bladders [30]. Intravesical application of PGE2 in rat bladders induced overactivity through activation of a certain population of A-delta fibers responsible for high-pressure (>15 cm H2O) detrusor contractions, suggesting PGE2 can modulate afferent nerve activity of the bladder [31]. PGE2 increased basal tone and spontaneous contractions of guinea pig bladders [32]. Among the therapeutic medication for DU, PGE2 had been considered as a potentially effective agent to improve spontaneous voiding [33]. However, preliminary clinical trial did not prove the effectiveness.
The results of this study revealed that urinary PGE2 was significantly elevated in patients with DU and DHIC and marginally elevated in those with DO. Patients with DU and bladder function recovery had significantly higher urinary PGE2 level than patients without recovery and DO, suggesting the factors contributing to detrusor contractility are not completely lost in these bladders. The highly secreted PGE2 in DU bladders might reflect a compensatory response to certain bladder pathological conditions causing temporary low detrusor contractility. Through increase in PGE2 secretion from the urothelium or detrusor, patients with DU may regain detrusor contractility gradually. Measurement of baseline urinary PGE2 level might predict the recovery of bladder function in patients with DU.
Urothelium is not only a barrier to the urine solutes but also expresses various receptors and ion channels responsible for mechanical or thermal changes in the bladder [34]. The urothelium also exerts sensory function in the bladder filling and noxious stimuli [35]. The urothelium might influence the contractile state of detrusor smooth muscle, both through modifying its contractility and the extent of spontaneous activity [34]. Stimulation of these sensory receptors from mechanical trauma, hydrostatic pressure change and chronic inflammation can release chemicals such as adenosine triphosphate, PGE2, NGF, acetylcholine and nitric oxide which may have excitatory or inhibitory effects on the afferent nerves or detrusor contractility [36, 37].
An intact bladder mucosa is demonstrated to associate with an increase in spontaneous contractile activity in whole bladder preparation [38]. The urothelium exerts an excitatory effect on the underlying muscle, while the suburothelial tissue causes an inhibitory effect [34]. Patients with DU usually have a diminished bladder fullness or urgency sensation and cannot contract the detrusor sufficiently to complete bladder emptying. We have previously investigated the urothelial dysfunction in patients with DU and revealed that junction protein E-cadherin was significantly lower in patients with DU, suburothelial inflammation was significantly higher and the urothelial cell apoptosis was significantly higher in patients with DU [39]. These results indicate that urothelial dysfunction, increased suburothelial inflammation and altered sensory protein expressions in bladder mucosa were prominent in patients with DU, indicating urothelial signaling and sensory transduction pathways are impaired in DU bladders.
Like OAB, underactive bladder is also a dynamic disorder and the symptoms may change with time. The bladder function varies from acontractile to impaired contractility and low voiding efficiency. The underlying pathophysiology for different severity of DU might be different and attribute to different urothelial dysfunction, neuropathy, detrusor muscle contractility and bladder outlet resistance in individual patient. Therefore, trying to find one biomarker for prognosis of disease is not likely to be successful. However, it might be possible if we can search for a group of urinary proteins and precisely define the etiology and provide prognostic outcome of DU [40].
Limitations of this study are small case number and heterogeneity of etiologies of bladder conditions. Although DO, DHIC and DU are all urodynamically proven, the underlying etiology might be different. Therefore, the distribution of urinary proteins was not parametric. Nevertheless, the trend that urinary NGF, BDNF and PGE2 levels are elevated in DU patients with bladder function recovery compared with the control group still have clinical relevance and prognostic significance. In this study, we did not use urinary creatinine level to normalize the urinary NGF, BDNG and PGE2 levels because the concentration of these proteins had been calculated by the urine volume. Furthermore, urinary NGF had been found to significantly elevated in OAB and other inflammatory bladder diseases such as urinary tract infection or interstitial cystitis, using the Promega kit. However, recently the Promega kit was found to cross-react to the presence of immunoglobulin G in urine [41]. Several recently published studies did not reproduce the results. In this study, the NGF level was not very significantly higher than controls, possibly because a new kit was used in this study.
Conclusion
Patients with DU had significantly elevated urinary NGF, BDNF and PGE2 levels. DU patients with bladder function recovery had significantly higher urinary PGE2 and BDNF levels. Among the three urinary proteins, PGE2 provides the most prognostic value for bladder function recovery in patients with DU.
References
Andersson KE (2014) The many faces of impaired bladder emptying. Curr Opin Urol 24:363–369
Smith PP (2010) Aging and the underactive detrusor: a failure of activity or activation? Neurourol Urodyn 29:408–412
Kanai A, Andersson KE (2010) Bladder afferent signaling: recent findings. J Urol 183:1288–1295
Resnick NM, Yalla SV, Laurino E (1989) The pathophysiology of urinary incontinence among institutionalized elderly persons. N Engl J Med 320:1–7
Sakakibara R et al (2005) Is lumbar spondylosis a cause of urinary retention in elderly women? J Neurol 252:953–957
Pizzi A et al (2014) Urinary incontinence after ischemic stroke: clinical and urodynamic studies. Neurourol Urodyn 33:420–425
Ueda T, Yoshimura N, Yoshida O (1997) Diabetic cystopathy: relationship to autonomic neuropathy detected by sympathetic skin response. J Urol 157:590–594
Andersson KE (2010) Detrusor underactivity/underactive bladder: new research initiatives needed. J Urol 184:1829–1830
Miyazato M, Yoshimura N, Chancellor MB (2013) The other bladder syndrome: underactive bladder. Rev Urol 15:11–22
Van Koeveringe GA, Vahabi B, Andersson KE, Kirschner-Herrmans R, Oelke M (2011) Detrusor underactivity: a plea for new approaches to a common bladder dysfunction. Neurourol Urodyn 30:723–728
Chancellor MB, Blaivas JG (1995) Classification of neurogenic bladder disease. In: Chancellor MB (ed) Practical Neurourology. Butterworth. Heinemann, Boston, pp 25–32
Steers WD, Tuttle JB (2006) Mechanisms of disease: the role of nerve growth factor in the pathophysiology of bladder disorders. Nat Clin Pract Urol 3:101–110
Kim JC, Park EY, Seo SI, Park YH, Hwang TK (2006) Nerve growth factor and prostaglandins in the urine of female patients with overactive bladder. J Urol 175:1773–1776
Kuo HC (2012) Potential biomarkers utilized to define and manage overactive bladder syndrome. LUTS 1:32–41
Antunes-Lopes T et al (2013) Urinary neurotrophic factors in healthy individuals and patients with overactive bladder. J Urol 189:359–365
Wang LW, Han XM, Chen CH, Ma Y, Hai B (2014) Urinary brain-derived neurotrophic factor: a potential biomarker for objective diagnosis of overactive bladder. Int Urol Nephrol 46:341–347
Cruz CD (2014) neurotrophins in bladder function: what do we know and where do we go from here? Neurourol Urodyn 3:39–45
Richter HE et al (2017) Urinary biomarkers in women with refractory urgency urinary incontinence randomized to sacral neuromodulation versus onabotulinumtoxinA compared to controls. J Urol 197:1487–1495
Abrams P et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol 187:116–126
Alkis O, Zumrutbas AE, Toktas C, Aybek H, Aybek Z (2017) The use of biomarkers in the diagnosis and treatment of overactive bladder: can we predict the patients who will be resistant to treatment? Neurourol Urodyn 36:390–393
Cho KJ, Kim HS, Koh JS, Kim JC (2013) Changes in urinary nerve growth factor and prostaglandin E2 in women with overactive bladder after anticholinergics. Int Urogynecol J 24:325–330
Fry CH, Sahai A, Vahabi B, Kanai AJ, Birder LA (2014) What s the role for biomarkers for lower urinary tract disorders. Neurourol Urodyn 33:602–605
Yamauchi H, Akino H, Ito H, Aoki Y, Nomura T, Yokoyama O (2010) Urinary prostaglandin E2 was increased in patients with suprapontine brain diseases, and associated with overactive bladder syndrome. Urology 76:1267.e13–1267.e19
Ochodnicky P, Cruz CD, Yoshimura N, Cruz F (2012) Neurotrophins as regulators of urinary bladder function. Nat Rev Urol 9:628–637
Andersson KE, Arner A (2004) Urnary bladder contraction and relaxation: physiology and pathophysiology. Physiol Rev 84:935–986
McCafferty GP, Misajet BA, Laping NJ, Edwards RM, Thorneloe KS (2008) Enhanced bladder capacity and reduced prostaglandin E2-mediated bladder hyperactivity in EP3 receptor knockout mice. Am J Physiol Renal Physiol 295:F507–514
Shioyama R et al (2008) Long-lasting breaches in the bladder epithelium lead to storage dysfunction with increase in bladder PGE2 levels in the rat. Am J Physiol Regul Integr Comp Physiol 295:R714–718
Aoki K et al (2009) A higher level of prostaglandin E2 in the urinary bladder in young boys and boys with lower urinary tract obstruction. Biomed Res 30:343–347
Kim JC et al (2005) Changes of urinary nerve growth factor and prostaglandins in male patients with overactive bladder syndrome. Int J Urol 12:875–880
Yokoyama O et al (2011) Antimuscarinics suppress adenosine triphosphate and prostaglandin E2 release from urthelium with potential improvement in detrusor overactivity in rats with cerebral infarction. J Urol 185:2392–2397
Kuga N, Tanioka A, Hagihara K, Kawai T (2016) Moulation of afferent nerve activity by prostaglandin E2 upon urinary bladder distension in rats. Exp Physiol 10:577–587
Guan NN, Nilsson KF, Wiklund PN, Gustafsson LE (2014) Release and inhibitory effects of prostaglandin D2 in guinea pig urinary bladder and the role of urothelium. Biochim Biophys Acta 1840:3443–3451
Hindley R, Brierly RD, Thomas PJ (2004) Prostaglandin E2 and bethanechol in combination for treating detrusor underactivity. BJU Int 93:89–92
Birder LA et al (2012) How does the urothelium affect bladder function in health and diseases? ICI-RS 2011. Neurourol Urodyn 31:293–299
Birder LA et al (2001) Vanilloid receptor expression suggests a sensory role for urinary bladder epithelial cells. Proc Natl Acad Sci USA 98:13396–13401
Downie JW, Karmazny M (1984) Mechanical trauma to bladder epithelium liberates prostanoids which modulate neurotransmission in rabbit detrusor muscle. J Pharmacol Exp Ther 230:445–449
Andersson KE (2002) Bladder activation: afferent mechanisms. Urology 59:43–50
Sui GP, Wu C, Roosen A, Ikeda Y, Kanai AJ, Fry CH (2008) Modulation of bladder myofibroblast activity: implications for bladder function. Am J Physiol 295:F688–697
Jiang YH, Wang CC, Kuo HC (2017) Urothelial barrier deficits, suburothelial inflammation and altered sensory protein expression in detrusor underactivity. J Urol 197:197–203
Cartwright R, Afshan I, Derpapas A, Vijaya G, Khullar V (2011) Novel biomarkers for overactive bladder. Nat Rev Urol 8:139–145
Gamper M, Moser R, Viereck V (2017) Have we been led astray by the NGF biomarker data? Neurourol Urodyn 36:203–204
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Institutional Review Board and Ethics Committee of Buddhist Tzu Chi General Hospital (IRB: 105-142-B).
Informed consent
Informed consent was obtained from all individuals.
Rights and permissions
About this article
Cite this article
Chen, SF., Jiang, YH. & Kuo, HC. Urinary biomarkers in patients with detrusor underactivity with and without bladder function recovery. Int Urol Nephrol 49, 1763–1770 (2017). https://doi.org/10.1007/s11255-017-1666-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-017-1666-z