Abstract
Background
A high incidence of hypervolemic hypernatremia has been described in patients recovering from acute kidney injury (AKI) in intensive care units. However, this has been limited to only a few cases.
Methods
One hundred fifty adult patients recovering from AKI in the intensive care unit of a single institution during a 6-year period, who developed hypernatremia during the course of their illness, were investigated. Serum and urine electrolytes, osmolality, urea nitrogen and creatinine were measured. The weights of these patients at the time of hypernatremia development and at presentation to the hospital were also measured.
Results
Even though the hypernatremia was mild in most patients (146–160 mEq/L), the average rise in serum sodium concentration was 14.5 ± 7.1 mEq/L. Of the 34 patients who had all urinary studies available, the average urine osmolality was 436 ± 128 mmol/kg of which 172 ± 54 mmol/L was contributed by sodium, potassium and their accompanying anion. Another 204 ± 96 mmol/L was accounted for by urea and creatinine (mainly urea). Almost all the patients had hypervolemia as evidenced by the presence of edema and an average weight gain of more than 9 ± 11 kg between the time of presentation and the onset of hypernatremia despite likely having lost muscle mass from being in the intensive care unit for several days. The weight data were available in 54 patients, and only eight of these patients had lost weight at the time of the development of hypernatremia.
Conclusion
Hypervolemic hypernatremia is by far the most common cause of hypernatremia in patients in the intensive care unit. Even though the patients are in negative fluid balance at the time of the development of the hypernatremia, earlier saline administration has caused massive volume overload despite the ongoing losses. Post-AKI diuresis in the face of inability to maximally concentrate the urine because of renal failure often leads to mainly mild elevations in serum sodium concentration. The urine solute is mainly urea because of the often high serum urea concentrations with little electrolytes being present in the urine.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypernatremia is often thought to be hypovolemic as it is associated with large water losses. Of course hypernatremia only happens if there is a defect in water intake. Until recently, hypervolemic hypernatremia even though well described has been thought to occur often in the setting of hypertonic saline or hypertonic bicarbonate administration.
Post-AKI diuresis leading to hypernatremia has received little attention although it was first described many years ago by Luestscher and Blakman [1]. The condition is thought to occur whenever urinary water loss is either not replaced or is replaced by relatively hypertonic saline solutions [2]. Thus, the hypernatremia has been thought to be associated with hypovolemia and low total body sodium content. The existing description states patients usually develop intravascular volume depletion along with a delayed recovery of renal function because of the induction of pre-renal azotemia.
More recently, hypervolemic hypernatremia in patients recovering from acute tubular necrosis in the intensive care unit has been described [3]. However, the data obtained have been limited and the number of patients described has been few. Here, we add to the recent literature by describing another different cohort of adult patients in the ICU who developed hypernatremia with normouria or polyuria, during the recovery phase of AKI. These patients were not hypovolemic; instead, they were hypervolemic with massive retention of total body sodium and total body water. It is believed that in patients recovering from AKI, hypervolemic hypernatremia may actually be the most frequent cause of hypernatremia. Early recognition and appropriate treatment of these patients may enhance renal and patient recovery.
Methods
Study design and subjects
The electronic records of 150 patients recovering from AKI from 2009 to 2013 at the San Francisco General Hospital were reviewed. All patients were in the intensive care unit at the time when renal function was recovering. Laboratory findings including serum level of sodium, urea nitrogen and creatinine were followed serially. All 150 patients had hypernatremia as defined by a serum sodium concentration of >145 mEq/L. Fifty-four patients had weight data available at the time of hypernatremia and on admission to the hospital. Thirty-four patients had complete urinary studies (urine levels of osmolality, electrolytes, urea nitrogen and creatinine). Collected data were analyzed using Microsoft Excel statistical-use software (Microsoft Corporation, Redmond, Washington, USA) and expressed as average ± standard deviation of the mean.
Results
Patient characteristics
Of the 150 patients who recovered from AKI from acute tubular necrosis (pre-renal and post-renal acute renal failure patients were not included), 99 were men and 51 women (Table 1). The patients’ ages ranged from 25 to 93 years old, with a mean of 60 ± 16. All the patients were in the intensive care unit during the development of hypernatremia, and all had some degree of kidney failure.
Serum laboratory values
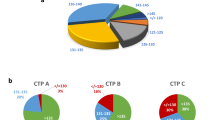
The average maximum serum sodium concentration of the 150 patients was 154 ± 6 mEq/L, with a range spanning from 146 to 189 mEq/L. The median highest serum sodium concentration was 153 mEq/L. The average rise in serum sodium concentration was 14.5 ± 7 mEq/L. We had serum osmolality measurement within 24 h of the highest serum sodium concentration in 57 of the patients, and the average serum osmolality was 339 ± 27 mmol/kg. The average maximum serum creatinine concentration was 4.6 ± 4.7 mg/dL in the entire group.
Urine laboratory values
Urine osmolality was measured in 81 (54 %) of the 150 patients within 48 h of the development of the highest serum sodium concentration to determine the ability of the kidneys to concentrate urine. The average urine osmolality during this period of renal recovery was 417 ± 130 mmol/kg, indicating a defect in maximally concentrating the urine in these hypernatremic hyperosmolar patients with kidney dysfunction. Forty-two patients had concomitant urine and serum osmolality measurements; the urine osmolality on average was found to be 74 ± 102 mmol/kg higher than the serum osmolality. The median difference between urine and serum osmolality values was 44 mmol/kg. Thus, this is consistent with the fact that for the most part in renal failure, the urine is close to being iso-osmolal with the serum.
Thirty-four patients had urine values of osmolality, electrolytes, urea nitrogen and creatinine measured on the same urine sample, thus enabling one to determine the constituents of the urine (Table 2). In these patients, the average urine osmolality was 436 ± 128 mmol/kg out of which 133 ± 55 mmol/L (31 %) was contributed to by sodium, potassium and chloride. Another 204 ± 96 mmol/L (47 %) comprised of urea nitrogen and creatinine, leaving only 99 ± 95 mmol/L for all other osmols present in the urine. If one more correctly uses 2× (urine Na + urine K) instead, then 172 ± 54 mol/L (39 %) are Na, K and their accompanying anions, leaving only 60 mmol/L for all other osmols (excluding urea and creatinine). This shows that urea contributes the most to the urine osmolality in these patients who often have a urine osmolality similar to serum osmolality (unable to concentrate urine maximally). High urea nitrogen levels in the blood thus will likely worsen the hypernatremia in these patients by increasing urea excretion [4].
Volume status
In order to evaluate the volume status of the patients, the admission weight was compared to the weight observed at the time of hypernatremia. Data were available in 54 (36 %) of the 150 patients (Fig. 1). The average weight gain at the time of occurrence of hypernatremia was 9.3 ± 10.6 kg higher than the admission weight in these patients who often already had been in the intensive care unit for weeks and had lost significant amount of body tissues such as muscle mass. Only eight out of the 54 patients (5.6 %) had actually lost weight at the time of hypernatremia development. Thus, clearly the patients with mild hypernatremia with kidney failure in the intensive care unit are almost universally hypervolemic.
Discussion
The human body is normally able to avoid hypernatremia (serum sodium concentration of >145 mEq/L) as a mild increase (1 %) in serum osmolality will lead to an increase in thirst. However, patients in the intensive care unit often are unable to depend on this mechanism to avoid hypernatremia as they are unable to drink water.
On a qualitative basis, we take in fluids with lower sodium concentration than human serum and also excrete fluids with lower sodium concentration than serum, while maintaining a relatively stable serum sodium concentration [3, 5]. The fluids that we excrete include stool with a sodium concentration of <50 mEq/L, sweat 36–56 mEq/L and saliva 15 mEq/L. Urine also usually has a sodium plus potassium concentration less than the corresponding serum sodium concentration. In the face of large losses of these low sodium containing bodily fluids and in the absence of replenishment by low sodium fluid intake, hypernatremia invariably develops. Large fluid losses happen in the intensive care unit patients often when they start recovering from their acute kidney injury but at times from other causes such as diarrhea.
Patients in intensive care unit often develop acute kidney injury as a result of sepsis, shock, surgery or use of nephrotoxic agents among other causes. Initially, when sepsis and/or hypotension develop, large volumes of saline with a sodium level that is close to that of serum are given. Because of the renal failure, not much urine is being produced and the administration of isotonic saline does not result in hypernatremia [3, 5]. When renal function begins to recover, an increasing volume of urine with an osmolality not too distant from that of serum is often excreted (as the kidneys are unable to concentrate the urine because of the renal failure). Another equally valid conclusion would be that the urine osmolality would not be high because of osmotic diuresis from urea excretion. However, we would rather attribute this to inability to maximally concentrate the urine because at times the patients develop increasing serum sodium concentrations despite making only 1–2 L of urine per day (not consistent with osmotic diuresis). This urine contains less sodium/potassium and more urea than serum [as urine osmolality is often mostly comprised of urea especially in these patients who have high serum urea nitrogen (BUN) concentrations]. Hypernatremia occurs because the ratio between sodium/potassium and water in the blood has changed due to the loss of water in excess of that of sodium/potassium.
In this larger cohort of patients than the cohort in our previous study, as a result of the loss of water in excess of that of sodium/potassium, serum sodium concentration rose by 14.5 ± 7 mEq/L in a matter of often less than 48 h. In our 34 patients with complete results, the combination of urea and creatinine accounted for 47 % of all urinary osmols, leaving little room for sodium and potassium as well as their attendant anions to contribute to the osmolality of the urine.
Even though at the time of development of hypernatremia, the patients were often in a negative fluid balance, overall they were still massively fluid-overloaded because of previous administration of saline containing fluids at the beginning of their illness. In fact on average the patients weighed more than 9 kg over the weight with which they had presented to the hospital despite the fact that often these patients were hospitalized for many days and had lost significant muscle mass [6]. Thus, the development of hypernatremia correlated with urinary loss of water in excess of those of sodium and potassium in the face of a smaller but still large total body volume.
Conclusion
We have reported that hypervolemic hypernatremia is common in AKI patients in intensive care units. Because of shock or hypotension, these patients are often given large quantities of physiological saline during the oliguric/anuric phase of their AKI, leading to the retention of much sodium and water as evidenced by the presence of edema and substantial weight gain. However, at this time they are not hypernatremic as their output is low and input has the same sodium concentration as serum. Hypernatremia occurs during the recovery of renal function phase on account of the loss of water in excess of sodium and potassium. This occurs because of combination of several factors [5]: (1) inability to normally concentrate the urine from acute and less commonly chronic kidney dysfunction, (2) high urine or stool output, (3) large urea output from the high serum urea concentration and (4) inability to drink water. Even though, at the time of development of hypernatremia, many patients are losing weight, they are actually still severely volume-overloaded because of the earlier administration of a large amount of saline. Prevention by paying close attention to water and sodium balance throughout a patient’s hospital stay, especially when there is large urine or stool output is crucial to minimize the increase in serum sodium concentration.
References
Luetscher JA, Blackman SS (1943) Severe kidney and brain injury following sulfathiazole. Ann Intern Med 15:741
Brady HR, Brenner BM (2001) Acute renal failure. In: Braunwald E, Fauci AS, Kaper DL, Hause SL, Longo DL, Jameson JL (eds) Harrison’s principles of internal medicine, 15th edn. McGraw-Hill, New York, pp 1541–1551
Sam R, Hart P, Haghighat R, Ing TS (2012) Hypervolemic hypernatremia in patients recovering from acute kidney injury in the intensive care unit. Clin Exp Nephrol 16(1):136–146
Popli S, Tzamaloukos AH, Ing TS (2014) Osmotic diuresis induced hypernatremia: better explained by solute-free water clearance or electrolyte free water clearance? Int Urol Nephrol 46:207–210
Sam R, Feizi I (2012) Understanding hypernatremia. Am J Nephrol 36:97–104
Prowle JR, Kolic I, Purdell-Lewis J, Talylor R, Pearse RM, Kirwan CJ (2014) Serum creatinine changes associated with critical illness and detection of persistent renal dysfunction after AKI. Clin J Am Soc Nephrol 9(6):1015–1023
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have declared that no conflict of interest exists.
Rights and permissions
About this article
Cite this article
Sarahian, S., Pouria, M.M., Ing, T.S. et al. Hypervolemic hypernatremia is the most common type of hypernatremia in the intensive care unit. Int Urol Nephrol 47, 1817–1821 (2015). https://doi.org/10.1007/s11255-015-1103-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1103-0