Abstract
Introduction
Electrocautery, harmonic scalpel tissue dissection and other surgical techniques can generate surgical smoke with high proportion of ‘fine particles’ (PM2.5) <2.5 μm, which is known to have adverse effects on human health. The high-risk zone for PM2.5 during surgeries by time and by distance has not been well evaluated.
Methods
The study included open superficial, open abdominal, open pelvic, laparoscopic and transurethral urology surgeries, five of each. A particle counter was placed at three different distances from the incision site, and the real-time PM2.5 concentration was displayed after each cut. Air Quality Index (AQI) revised by the US Environmental Protection Agency and the calculated inhalation dose were used to evaluate the severity of PM2.5.
Results
In superficial, abdominal and pelvic surgeries, the peak PM2.5 concentration may reach 245.7, 149.4 and 165.1 μg/m3 3–6 s after a single cut 40 cm from the incision site. By the time, AQI usually turns to ‘unhealthy’ or ‘very unhealthy.’ In laparoscopic surgeries, 40 cm from the trocar, the air quality reached ‘hazardous’ in 3 s after opening of the trocar valve with a peak concentration of 517.5 μg/m3. In transurethral surgeries, the AQI 40 cm away from the resectoscope is generally at moderate level. In each surgery, the chief surgeon may inhale most of the PM2.5, while the assistant will inhale less than half the dose, and the scrub nurse may inhale nearly none. The use of wall suction may induce a 48–65 % decrease in fine particle inhalation.
Conclusions
During surgeries, the concentration of PM2.5 could reach a very unhealthy status, especially for the chief surgeon who is the nearest to the incision site. Surgical smoke evacuation in the first few seconds of a cut is essential; however, using smoke evacuators such as a wall suction alone may not be enough.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Electrocautery, harmonic scalpel tissue dissection and other equipments which can generate surgical smoke are widely used in the era of urology. Surgeons are exposed to surgical smoke not only from open surgeries, but also from laparoscopic surgeries [1], transurethral resection of bladder tumors (TURBT) and transurethral resection of the prostate (TURP) [2]. Surgical smoke is usually composed of chemicals, blood and tissue particles, viruses and bacteria, bringing potential harmfulness to the health of operating room personnel [3]. Large amount of carbon monoxide and carcinogenic compounds such as acrylonitrile, hydrogen cyanide, formaldehyde and benzene were found in surgical smoke [4]. It is also said that HPV may be transmitted by surgical plume, making its infectiousness of great concern [5]. However, compositions of surgical smoke vary, and it is hard to evaluate its harmfulness without a unified factor.
Particulate matter <2.5 μm (PM2.5) was mainly demonstrated as one of the main environmental air pollutants [6]. Interestingly, surgical smoke may simply be a wisp of PM2.5. Weld et al. mentioned that surgical smoke is composed of two distinct particle populations caused by the nucleation of vapors as they cool (the small particles) and the entrainment of tissue secondary to mechanical aspects (the large particles). The mean size of small particles was 68.3 nm and of the larger ones was 994 nm [7]. The horrible thing of PM2.5 is that they can directly reach the small airways and alveoli, thus leading to local inflammatory response, activation of prothrombotic factors, development of atherosclerosis and cardiovascular diseases [8]. Meta-analysis showed that PM2.5 is associated with increased hospitalization and mortality due to cardiopulmonary disease [9]. Though the concept of PM2.5 made it easier to estimate the harmfulness of surgical smoke, we still need to know at what time and at what distance should we be most aware of them.
In the current study, we tried to analyze the amount of PM2.5 generated in different urology surgeries by time and by distance.
Methods
Surgery types and patients
We conducted a prospective study to analyze PM2.5 generated through open surgeries, laparoscopic surgeries and transurethral surgeries. Our department is a cancer center, so all of the patients involved are suspected to have malignant tumors. We chose three subtypes of surgeries due to surgery depth for the open surgery group: inguinal lymph node dissection for penile cancer (superficial surgeries), partial nephrectomy (abdominal surgeries) and radical prostatectomy (pelvic surgeries). Laparoscopic partial nephrectomy was chosen for the laparoscopic surgery group. Transurethral surgeries included TURBT. For each types of surgeries mentioned above, five patients were analyzed. All procedures were performed in the same laminar airflow operating room. The study was approved by the institutional review board of our medical institution. All the patients submitted a written informed consent.
Instruments and measurement strategy
Dylos 1700 (Dylos, California, USA): this instrument uses a laser light scattering technique to measure the number of particles. The instrument draws air through an inlet (4 × 6 cm) in the casing of the device using a small fan. Particle counts are expressed as a concentration per 0.01 cu ft of sampled air with the upper limit of the device memory 65,536 particle counts per 0.01 cu ft (0.283 l). The formula used to calculate adjusted measurement of PM2.5 mass (μg/m3) was as follows: y = 1.57 × 10−7 × x 2 + 4.16 × 10−3 × x + 0.65 [10], where x is the number of particles counted by the Dylos 1700 (per 0.01 cu ft) and y is the adjusted measurement of PM2.5 mass (μg/m3). Dylos is able to produce an instant measurement of PM2.5, so we were able to record the amount change of surgery smoke particles generated per second.
Dissection and resection during open and laparoscopic surgeries were carried out using bipolar electrocautery units (FORCE 300, Valleylab, Boulder, CO, USA), and the power setting was 40 W. TURBT was performed using a 22F resectoscope, and a standard tungsten cutting loop, and the electrosurgical generator (AUTOCON, Karl Storz, GmbH) was set to 150 W for cutting and vaporization.
For open surgeries, the inlet of Dylos was placed at three different distances (40, 60 and 120 cm) from the incision site, near the breathing zone of surgical personnel, to imitate the position of the operator (40 cm), the assistant (60 cm) and the scrub nurse (120 cm). Every cut should last for 2–3 s, and the measuring of PM2.5 should be started and continued for 15 s right after the cut. The PM2.5 was measured with and without a wall suction for surgical smoke evacuation [11]. For laparoscopic surgeries, the inlet of Dylos was placed at three different distances (40, 60 and 120 cm) from the trocar outlet at the horizontal level of 170 cm, to imitate the position of the operator, the assistant and the scrub nurse. The valve of the trocar was opened for 3 s to release surgical smoke as long as the smoke impacts the surgeon’s vision of the surgical site. For transurethral surgeries, the inlet of Dylos was placed at 40 cm away from the resectoscope at the horizontal level of 130 cm to imitate the position of the operator, and the measurement should be started and continued for 15 s as soon as we pull out the resectoscope for specimen collecting or irrigation solution exchanging. For each patient, the measurement is triplicated. We also measured the background PM2.5 when a surgery started.
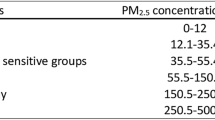
We used the Air Quality Index (AQI, The National Ambient Air Quality Standards for Particle Pollution; Web site: http://www.epa.gov/airquality/particlepollution/2012/decfsstandards.pdf) for PM2.5 revised by the US Environmental Protection Agency (EPA) to evaluate how clean or polluted the air is. For example, the AQI converts concentrations for fine particles to a number on a scale from 0 to 500, different scores in the scale refers to different qualities of the air, such as ‘good,’ ‘moderate’ and ‘unhealthy for sensitive groups.’ The AQI breakpoints are outlined in the table below:
AQI category | PM2.5 breakpoints (μg/m3) |
|---|---|
Good | 0.0–12.0 |
Moderate | 12.1–35.4 |
Unhealthy for sensitive groups | 35.5–55.4 |
Unhealthy | 55.5–150.4 |
Very unhealthy | 150.5–250.4 |
Hazardous | 250.5–350.4 |
350.5–500 |
Statistical analysis
The instant PM2.5 value of each procedure was recorded and plotted in linear graphs. Inhalation dose for each cut were calculated by exposure concentration and inhalation rate: D = ∫t1t2C(t)·IR(t)·dt/60 [12], where D stands for the inhalation dose, μg; C(t) is the real-time exposure concentration, μg/m; t1 and t2 stand for the start and end time of exposure, respectively, s; and IR(t) is the respiratory rate, m3/min. The mean respiratory rate for adults with light intensity activity level is 1.2 × 10−2 m3/min, respectively [13]. The mean ± standard deviation amount of inhalation dose of PM2.5 was calculated, and the Student t test was performed to test the differences between them. The accumulation of PM2.5 dose according to time from the cut was calculated in percentages. We compared the inhalation dose of PM2.5 in different procedures and different conditions (distance, with or without the use of wall suction). All analyses were performed using SPSS 17.0 software. P values were two-tailed and considered significant when <0.05.
Results
The characteristics of the patients and the surgery types they had undergone are shown in Table 1. PM2.5 was measured in 25 surgeries; these operations took place between November 2013 and March 2014 at Fudan University Shanghai Cancer Center, China. Each type of surgeries was consecutively selected, the mean age of the patients was nearly 60 years old, and most patients had a normal body mass index (BMI). Background PM2.5 was measured when a surgery started in the operating room, and the value was nearly 5 μg/m3, which is quite same for all of the surgeries.
The instant PM2.5 value of each procedure was recorded and plotted in linear graphs as shown in Fig. 1. The concentration of PM2.5 varies at different distances from the incision site. In superficial surgeries, the operator (40 cm) may inhale 2.47 μg PM2.5 at every single cut, while the assistant (60 cm) may inhale 1.18 μg, and the scrub nurse (120 cm) may only inhale about 0.19 μg PM2.5. The similar phenomenon can also be seen in other open surgeries. In laparoscopic surgeries, the operator may inhale 4.33 μg PM2.5, while the assistant and the scrub nurse may inhale 1.21 μg and 0.08 μg PM2.5.
Concentrations for PM2.5 and their relation with AQI are shown in Table 2. The AQI of the air 40 cm from the incision site usually turns to ‘unhealthy’ or ‘very unhealthy’ 3–6 s after a single cut, and the peak PM2.5 concentration may reach 245.7, 149.4 and 165.1 μg/m3 for superficial, abdominal and pelvic surgeries. In laparoscopic surgeries, the AQI 40 cm facing the trocar reached ‘hazardous’ in 3 s after we open the trocar valve with a peak concentration of 517.5 μg/m3. However, in transurethral surgeries, the AQI 40 cm away from the resectoscope is generally at moderate level.
Figure 2 shows the accumulation of PM2.5 dose (40 cm away from the incision site or trocar) calculated in percentages. It took 5.1, 5.8 and 6.6 s for the inhalation dose to reach 80 % after a single cut in superficial, abdominal or pelvic surgeries. In laparoscopic surgeries, it took 3.7 s for the inhalation dose to reach 80 %.
We measured PM2.5 with and without a wall suction for surgical smoke evacuation (Fig. 3). In open surgeries, wall suction is used and the concentration of PM2.5 and the inhalation dose are shown in Fig. 3. With the use of wall suction, inhalation dose decreased from 2.47 to 1.29 μg (48 % off) in superficial surgeries, 1.72–0.84 μg (52 % off) in abdominal surgeries and 1.61–0.57 μg (65 % off).
Discussion
Many studies have evaluated the composition and concentration of surgical smoke. However, few studies have investigated PM2.5 produced during surgeries. In the current study, we verified the amount of PM2.5 that surgical staffs may be involved with in five types of urology surgeries. The main finding of the article is that in most of the surgeries, the concentration of PM2.5 of a single smoke plume could become very unhealthy for involved surgeons. In open superficial surgeries, for example, the chief surgeon may inhale 2.47 μg of PM2.5 in 15 s after a single cut. Generally speaking, one will inhale such amount of particular matter only if he stands in an air-polluted area with a 55 μg/m3 PM2.5 for the same time length, and this level of PM2.5 is much higher than the short-term fine particle standard (35 μg/m3) which was issued by the US EPA [14]. On the other hand, the real-time concentration of PM2.5 will reach a peak level about 3–6 s after a single cut. At this period of time, PM2.5 may become ‘very unhealthy’ or even ‘hazardous’ (Table 2). Luckily, while the distance to the incision site increases, the concentration and inhalation dose of PM2.5 decrease rapidly; the assistant will inhale less than half the dose compared with the chief surgeon, while the scrub nurse may inhale nearly none. Data also showed that the accumulation dose of PM2.5 can reach 80 % usually at the sixth second for open surgeries and at the fourth second for laparoscopic surgeries (Fig. 2). We then measured PM2.5 with a wall suction for surgical smoke evacuation. This simple and widely used device can easily capture surgical smoke and reduce the concentration of PM2.5.
In 2004, the first American Heart Association scientific statement concluded that exposure to particulate matter air pollution contributes to cardiovascular morbidity and mortality [6]. Further studies extended the findings that exposure to PM2.5 over a few hours to weeks can trigger cardiovascular disease-related mortality and nonfatal event [15]. In Europe, the multicenter European Study of Cohorts for Air Pollution Effects (ESCAPE) project was held to investigate air pollutants and their associated disease. The results of ESCAPE concluded that exposure to air pollutants, especially PM2.5 may increase natural-cause mortality (HR = 1.07 per 5 μg/m3 increase) [16], incidence of lung cancer (HR = 1.18 per 5 μg/m3 increase) [17], acute coronary events (HR = 1.13 per 5 μg/m3 increase) [18] and low birthweight (HR = 1.18 per 5 μg/m3 increase) [19]. Generally speaking, in those large epidemiology studies, PM2.5 was measured in the outdoor atmosphere. The anthropogenic sources of outdoor PM2.5 include motor vehicle emissions, tire fragmentation, road dust and other industrial combustion, while the natural sources include wood burning, soil, pollens and molds. In contrast, surgical smoke is usually composed of hydrocarbons, nitriles, fatty acids, phenols, blood and tissue particles, viruses and bacteria, quite different from the outdoor atmosphere. How much harm surgical PM2.5 will do to surgeons is still unknown. However, we cannot conclude that surgical PM2.5 is not harmful simply because they are not traffic emissions. Multiple studies of air pollutants have been held in different cities to help isolate the pollutants that may be more responsible for the health effects, and consistent positive findings with PM2.5 instead of other certain particles were found [15]. In the ESCAPE study, PM2.5 consistently associated with natural-cause mortality even if the author adjusted the model with traffic variables [16]. So the size/morphology of surgical particle matters may be their major characteristic, for they are a ‘group’ of particles which can reach the small airways and alveoli just the same as PM2.5 from the atmosphere, thus causing systemic inflammation, systemic oxidative stress, thrombosis and coagulation. On the other hand, chemicals present in surgical smoke include carbon monoxide, acrylonitrile, hydrogen cyanide, formaldehyde and benzene. Some of those are carcinogenic and can have independent and potentially synergistic or antagonistic effects with each other and with PM2.5 [4].
In 2007, Spearman et al. did a survey on surgical staffs, found that most people were concerned about exposure to surgical smoke and felt that precautions were inadequate. However, the author mentioned that the use of smoke extraction equipment is very limited [20]. Usually, in order to avoid surgical smoke pollution, we can use local exhaust ventilations (such as wall suction or smoke evacuator) and respiratory protections (such as surgical mask or N95 or other National Institute for Occupational Safety and Health (NIOSH)-approved respirator). In a survey done in 2012, we noticed that wall suction may be the most widely used for surgical smoke control [11]. In our institute, we use wall suction for smoke evacuation and we do observed a 48–62 % decrease in surgical PM2.5 exposure. Thus, for procedures that produce only nuisance levels of smoke, wall suction is entirely adequate. For respiratory protections, the literature indicated that only ‘N95 or other NIOSH-approved respirator’ choice ensures some measure of protection [11]. Truthfully, we investigated that regular surgical masks (used in our institute) are nearly useless in reducing PM2.5 (data not shown).
Conclusions
During surgeries, the concentration of PM2.5 could reach a very unhealthy status, especially for the chief surgeon who is the nearest to the incision site. Surgical smoke evacuation in the first few seconds of a cut is essential; however, using smoke evacuators such as a wall suction alone may not be enough. Surgeons and other OR personnel should be aware of the potential health hazards and should take proper measures to minimize their exposure to surgical PM2.5.
References
Choi SH, Kwon TG, Chung SK, Kim TH (2014) Surgical smoke may be a biohazard to surgeons performing laparoscopic surgery. Surg Endosc 28(8):2374–2380. doi:10.1007/s00464-014-3472-3
Zhao C, Kim MK, Kim HJ, Lee SK, Chung YJ, Park JK (2013) Comparative safety analysis of surgical smoke from transurethral resection of the bladder tumors and transurethral resection of the prostate. Urology 82(3):744.e9–744.e14. doi:10.1016/j.urology.2013.05.028
Hensman C, Baty D, Willis RG, Cuschieri A (1998) Chemical composition of smoke produced by high-frequency electrosurgery in a closed gaseous environment. An in vitro study. Surg Endosc 12(8):1017–1019
Barrett WL, Garber SM (2003) Surgical smoke: a review of the literature. Is this just a lot of hot air? Surg Endosc 17(6):979–987. doi:10.1007/s00464-002-8584-5
Garden JM, O’Banion MK, Bakus AD, Olson C (2002) Viral disease transmitted by laser-generated plume (aerosol). Arch Dermatol 138(10):1303–1307
Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, Luepker R, Mittleman M, Samet J, Smith SC Jr, Tager I (2004) Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation 109(21):2655–2671. doi:10.1161/01.CIR.0000128587.30041.C8
Weld KJ, Dryer S, Ames CD, Cho K, Hogan C, Lee M, Biswas P, Landman J (2007) Analysis of surgical smoke produced by various energy-based instruments and effect on laparoscopic visibility. J Endourol 21(3):347–351. doi:10.1089/end.2006.9994
Walczak DA, Grobelski B, Pasieka Z (2011) “There is no smoke without a fire”—surgical smoke and the risk connected with it. Pol Przegl Chir 83(11):634–639. doi:10.2478/v10035-011-0101-x
Atkinson RW, Kang S, Anderson HR, Mills IC, Walton HA (2014) Epidemiological time series studies of PM2.5 and daily mortality and hospital admissions: a systematic review and meta-analysis. Thorax 69(7):660–665. doi:10.1136/thoraxjnl-2013-204492
Semple S, Ibrahim AE, Apsley A, Steiner M, Turner S (2013) Using a new, low-cost air quality sensor to quantify second-hand smoke (SHS) levels in homes. Tob Control. doi:10.1136/tobaccocontrol-2013-051188
Edwards BE, Reiman RE (2012) Comparison of current and past surgical smoke control practices. AORN J 95(3):337–350. doi:10.1016/j.aorn.2011.07.019
Yu Q, Lu Y, Xiao S, Shen J, Li X, Ma W, Chen L (2012) Commuters’ exposure to PM1 by common travel modes in Shanghai. Atmos Environ 59:39–46
U.S. Environmental Protection Agency (EPA) (2011) Exposure factors handbook: 2011 Edition. National Center for Environmental Assessment W, DC; EPA/600/R-09/052F. Available from the National Technical Information Service, Springfield, VA, and online at http://www.epa.gov/ncea/efh
Revised Air Quality Standards For Particle Pollution and Updates to the Air Quality Index (AQI). The National Ambient Air Quality Standards for Particle Pollution web site: http://www.epa.gov/airquality/particlepollution/2012/decfsstandards.pdf
Brook RD, Rajagopalan S, Pope CA 3rd, Brook JR, Bhatnagar A, Diez-Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, Peters A, Siscovick D, Smith SC Jr, Whitsel L, Kaufman JD (2010) Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 121(21):2331–2378. doi:10.1161/CIR.0b013e3181dbece1
Beelen R, Raaschou-Nielsen O, Stafoggia M, Andersen ZJ, Weinmayr G, Hoffmann B, Wolf K, Samoli E, Fischer P, Nieuwenhuijsen M, Vineis P, Xun WW, Katsouyanni K, Dimakopoulou K, Oudin A, Forsberg B, Modig L, Havulinna AS, Lanki T, Turunen A, Oftedal B, Nystad W, Nafstad P, De Faire U, Pedersen NL, Ostenson CG, Fratiglioni L, Penell J, Korek M, Pershagen G, Eriksen KT, Overvad K, Ellermann T, Eeftens M, Peeters PH, Meliefste K, Wang M, Bueno-de-Mesquita B, Sugiri D, Kramer U, Heinrich J, de Hoogh K, Key T, Peters A, Hampel R, Concin H, Nagel G, Ineichen A, Schaffner E, Probst-Hensch N, Kunzli N, Schindler C, Schikowski T, Adam M, Phuleria H, Vilier A, Clavel-Chapelon F, Declercq C, Grioni S, Krogh V, Tsai MY, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Katsoulis M, Trichopoulou A, Brunekreef B, Hoek G (2014) Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet 383(9919):785–795. doi:10.1016/S0140-6736(13)62158-3
Raaschou-Nielsen O, Andersen ZJ, Beelen R, Samoli E, Stafoggia M, Weinmayr G, Hoffmann B, Fischer P, Nieuwenhuijsen MJ, Brunekreef B, Xun WW, Katsouyanni K, Dimakopoulou K, Sommar J, Forsberg B, Modig L, Oudin A, Oftedal B, Schwarze PE, Nafstad P, De Faire U, Pedersen NL, Ostenson CG, Fratiglioni L, Penell J, Korek M, Pershagen G, Eriksen KT, Sorensen M, Tjonneland A, Ellermann T, Eeftens M, Peeters PH, Meliefste K, Wang M, Bueno-de-Mesquita B, Key TJ, de Hoogh K, Concin H, Nagel G, Vilier A, Grioni S, Krogh V, Tsai MY, Ricceri F, Sacerdote C, Galassi C, Migliore E, Ranzi A, Cesaroni G, Badaloni C, Forastiere F, Tamayo I, Amiano P, Dorronsoro M, Trichopoulou A, Bamia C, Vineis P, Hoek G (2013) Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol 14(9):813–822. doi:10.1016/S1470-2045(13)70279-1
Cesaroni G, Forastiere F, Stafoggia M, Andersen ZJ, Badaloni C, Beelen R, Caracciolo B, de Faire U, Erbel R, Eriksen KT, Fratiglioni L, Galassi C, Hampel R, Heier M, Hennig F, Hilding A, Hoffmann B, Houthuijs D, Jockel KH, Korek M, Lanki T, Leander K, Magnusson PK, Migliore E, Ostenson CG, Overvad K, Pedersen NL, Juha Pekkanen J, Penell J, Pershagen G, Pyko A, Raaschou-Nielsen O, Ranzi A, Ricceri F, Sacerdote C, Salomaa V, Swart W, Turunen AW, Vineis P, Weinmayr G, Wolf K, de Hoogh K, Hoek G, Brunekreef B, Peters A (2014) Long term exposure to ambient air pollution and incidence of acute coronary events: prospective cohort study and meta-analysis in 11 European cohorts from the ESCAPE Project. BMJ 348:f7412
Pedersen M, Giorgis-Allemand L, Bernard C, Aguilera I, Andersen AM, Ballester F, Beelen RM, Chatzi L, Cirach M, Danileviciute A, Dedele A, Eijsden M, Estarlich M, Fernandez-Somoano A, Fernandez MF, Forastiere F, Gehring U, Grazuleviciene R, Gruzieva O, Heude B, Hoek G, de Hoogh K, van den Hooven EH, Haberg SE, Jaddoe VW, Klumper C, Korek M, Kramer U, Lerchundi A, Lepeule J, Nafstad P, Nystad W, Patelarou E, Porta D, Postma D, Raaschou-Nielsen O, Rudnai P, Sunyer J, Stephanou E, Sorensen M, Thiering E, Tuffnell D, Varro MJ, Vrijkotte TG, Wijga A, Wilhelm M, Wright J, Nieuwenhuijsen MJ, Pershagen G, Brunekreef B, Kogevinas M, Slama R (2013) Ambient air pollution and low birthweight: a European cohort study (ESCAPE). Lancet Respir Med 1(9):695–704. doi:10.1016/S2213-2600(13)70192-9
Spearman J, Tsavellas G, Nichols P (2007) Current attitudes and practices towards diathermy smoke. Ann R Coll Surg Engl 89(2):162–165. doi:10.1308/003588407X155752
Acknowledgments
This work was supported by grants from the National Natural Science Foundation of China (No. 81202004).
Author contributions
Hong-Kai Wang, Fei Mo and Hai-Liang Zhang had full access to all of the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Hong-Kai Wang, Fei Mo, Chun-Guang Ma, Bo Dai, Guo-Hai Shi, and Yao Zhu involved in acquisition of data. Hai-Liang Zhang involved in study concept and design. Hong-Kai Wang wrote the manuscript. Supervision: Ding-Wei Ye and Hai-Liang Zhang conceived of the study and participated in its design and coordination.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
All authors declare no competing financial interests.
Additional information
Hong-Kai Wang and Fei Mo have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Wang, HK., Mo, F., Ma, CG. et al. Evaluation of fine particles in surgical smoke from an urologist’s operating room by time and by distance. Int Urol Nephrol 47, 1671–1678 (2015). https://doi.org/10.1007/s11255-015-1080-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1080-3