Abstract
The overall number of very elderly patients (>79 years of age) requiring renal replacement therapy is rising in the Western societies, with a choice for managing advanced chronic renal disease among hemodialysis, peritoneal dialysis, kidney transplant, conservative, or palliative care. The selection of the most adequate alternatives should be tailored to meet individual needs, considering variables such as patient’s choice, clinical status, and social context, analyzed from a geriatric perspective, aiming not only to prolong patient’s life expectancy, but also to improve the patient’s quality of life. Frailty and sarcopenia are highly prevalent comorbidities found in very elderly population, particularly in the end-stage chronic renal disease population. Both comorbidities have a strong negative impact on health general status, and specific treatment should be provided in conjunction with the selected management for renal replacement, except when a palliative care has been implemented. Moreover, the detected degree of frailty in a renal patient can have an important influence on the decision about which modality of renal replacement treatment will be selected. All these alternatives and considerations are discussed in the present review article.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
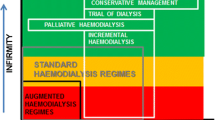
The number of very elderly patients (>79 years of age) who require renal replacement therapy is rising in the Western societies, currently representing approximately 25 % of the dialysis population [1, 2]. Elderly dialysis patients are usually characterized as having a tendency to start dialysis later, presenting fewer classic symptoms, having a higher number of comorbid conditions (diabetes mellitus, hypertension, and vascular disease), being exposed to polypharmacy (≥5 drugs), and having a higher risk of suffering from geriatric syndromes such as cognitive dysfunction, incontinence, gait disorders, falls, immobility, and frailty [3, 4]. Moreover, a subgroup of these individuals opt to discontinue chronic dialysis, and some even refuse its initiation [5, 6]. The currently available therapeutic alternatives for managing advanced chronic renal disease in the very elderly are as follows: hemodialysis, peritoneal dialysis, kidney transplant, and conservative or palliative care [7–9]. The selection of the most adequate alternatives should be tailored to meet individual needs taking into consideration variables such as patient’s choice, clinical status, and social context; and should be analyzed from a geriatric perspective, advocating not only to prolong patient’s life expectancy, but also to improve patient’s quality of life [10, 11]. Avoiding the risks of undertreatment, the management of the very elderly patients should be oriented toward objective biological expectations and to prevent any potential iatrogenic damage generated by known futile procedures [12]. Additionally, effective communication with patients and their families represents a cornerstone to ensure compliance to the treatment [11] (Table 1).
Dialysis
Older people represent the largest growing segment in chronic dialysis units primarily due to the fact that the prevalence of chronic kidney disease increases with age [1, 2, 13]. In very elderly patients, dialytic treatment is likely to be lifelong, with only a minority of all adult kidney transplantations taking place in this age subgroup [14]. Although there are many studies on quality of life and patient satisfaction, they are limited in scope, and collectively do not suggest that older patients are more tolerant of, less stressed by, and less depressed at dialysis than their younger counterparts [15, 16]. Besides, the vast majority of octogenarians (94 %) opt for treatment where dialysis was deemed appropriate by the renal care team [7]. However, since very elderly patients are usually more prone to rely upon their health care team in order to make treatment decisions, there is a higher risk that the modality favored by their physicians will become their treatment of choice [7]. Several reports have shown a reasonable survival for older people either on hemodialysis or on peritoneal dialysis, although it seems that an early dialysis initiation represents no significant medical advantage since it was found to be associated with greater mortality and hospitalization rates in this group [17, 18]. On the other hand, several studies have shown that survival is reduced in patients starting dialysis after a glomerular filtration rate (GFR) of 6 ml/min/1.73 m2, compared with starting dialysis earlier [19–21]. Thus, it seems that a setting based upon a GFR between 7 and 9 ml/min/1.73 m2 could be an adequate time for starting dialysis in clinical and laboratory stable very elderly end-stage chronic renal disease patients [19–22]. Additionally, because frail subjects are high prevalent among this group of patients, home assisted dialysis (peritoneal dialysis or hemodialysis) appears to be an adequate dialytic option for them, considering that about 60 % of this population needs any kind of assistance [23, 24]. Very elderly patients who are not able for self-care can be supported through assisted dialysis, particularly peritoneal dialysis, where trained caregivers provide daily dialysis assistance either in a nursing home or at the patient’s home [23–25].
Hemodialysis
In 1996, 7,054 patients aged 80 started dialysis; while in 2003, this number rose to 13,577, equivalent to an annual increase of 9.8 % in the USA [25]. After adjusting for population growth in this age group, the increase between 1996 and 2003 was 57 % [25, 26]. Elderly patients are treated more frequently by hemodialysis (81 %) than by peritoneal dialysis (19 %), when compared with younger patients: 65 versus 35 %, respectively [26]. High prevalence of dependency among very elderly people could help to explain the preference of hemodialysis, a passive therapeutic modality, as the treatment of choice [26, 27]. It has been reported that among all the stable elderly patients who started hemodialysis, one-third died and one-third suffered marked deterioration over a period of 6 years [25–27]. In this regard, stable very elderly patients on hemodialysis show survival advantage compared with those on a conservative treatment, except for fragile patients [3, 28]. Hemodialysis may offer some advantages for very elderly patients. First, it is an adequate modality for treating disabled elderly patients since, as mentioned before, it is an assisted (passive) therapy [25, 26]. Second, hemodialysis also offers an opportunity for socialization with physicians and other patients and also has a frequent follow-up by a medical team [25, 26]. Finally, hemodialysis takes a shorter treatment time compared with the peritoneal alternative [25–27]. On the other hand, octogenarian in hemodialysis are at higher risk of suffering several problems. A common and important one is the tendency to intra-dialytic hypotension (30 %), which can be followed by ischemic complications, such as stroke, and angina (cardiac or intestinal) [25–27]. These complications have been attributed to characteristic vascular autonomic dysfunction and/or arrhythmias usually observed in the elderly [27, 29]. Other significant complications of hemodialysis are vascular access related. Same as what happens with younger patients, permanent vascular accesses are preferable (safer) than catheters in very elderly patients [27, 30]. Since very elderly patients are more prone to have poor-quality vessels due to prior vascular interventions or senile vascular changes (atheroma and calcification) compared with younger patients, then slow maturation, inadequate blood flow, and tendency to obstruction (thrombosis) usually characterizes, not always, the evolution of native dialysis accesses in this group [29–31]. Conversely, a recent report found that very elderly patients had a vasculature suitable for autogenous access construction [32]. Arteriovenous graft provides an easier surface for cannulation and a shorter time to mature compared with arteriovenous fistula, but has a higher incidence of arm swelling and steal syndrome in the elderly [30–32]. Other reported hemodialysis complications are as follows: residual renal function loss (induced by intra-dialytic renal hypoperfusion), malnutrition (due to dialytic aminoacid losses), endovascular infections (promoted by immunosenescence changes), gastrointestinal bleeding (secondary to gastritis, ulcer, and angiodisplasia), traveling to/from dialysis units (hindered by immobility syndrome), reduced rehabilitation time, and dependence for transportation [30, 33]. Moreover, hemodialysis can even worsen geriatric syndromes in frail elderly patients, and consequently increased their mortality risk [33–36].
Peritoneal dialysis
In dialysis units where assisted modalities are available to support patients within their homes, 75 % of those who chose peritoneal dialysis received assisted peritoneal dialysis compared with self-care peritoneal dialysis [3]. Data from registries show that nurse-assisted patients have a median survival time comparable to that with independent elderly patients on renal replacement therapy, and adverse events were no different between both groups [3, 24]. It has been reported that the spent dialysate volume was significantly lower (3.8 l/day) in the very elderly group compared with younger ones, but these smaller volumes usually used in very elderly patients were not accompanied by a significantly increase in serum β2 microglobulin level compared with younger patients [30]. Moreover, it is considered that this strategy of smaller peritoneal dialysis volumes is beneficial to avoid excessive albumin loss from the peritoneal cavity [37]. It has also been documented that the occurrence of peritonitis and cardiovascular disease complications did not increase over time in the very elderly with respect to other age groups, and the same is valid for the rate of technical survival and reduction of serum albumin levels [30]. Pathogen microorganisms are similar to those in younger patients (Staphylococcus epidermidis), although some reports found a higher incidence of gram-negative bacteria, explained by the higher incidence of gastrointestinal pathology (constipation, diverticulosis, and bowel perforation) in this group [30, 37, 38]. Older patients are less active and have a weaker abdominal musculature, these characteristics explain why they have less frequent exit site and tunnel complications, and higher incidence of hernias compared with younger patients [38, 39]. Peritoneal dialysis offers many advantages for very old patients, such as access simplicity, exchange schedule flexibility, and cardiovascular stability (less hypotension and arrhythmia), due to slow solute and volume removal, preserved residual renal function, better control of hypertension, independence from hospitals (no need of transportation), more liberal diet, and a greater sense of well-being compared with those on hemodialysis [30, 37, 40, 41]. Besides, current information technologies such as telenephrology, and recording and monitoring devices, make it easier to handle very elderly peritoneal dialysis patients at home, and reduces their need of visiting dialysis units [42]. On the other hand, this modality may lead to some complications in this very elderly people, as it is the case of intensification of patient’s isolation and protein malnutrition (peritoneal protein loss) [24, 30]. Malnutrition is an important complication highly correlated with mortality [12]. It may reflect factors such as low income, social isolation, depression, dental problem, malabsorption, or drug-related effects [10, 12, 43]. Moreover, frequent clinical disorders in the very elderly such as cognitive, visual, and/or impaired manual dexterity pose additional barriers to prescribe peritoneal dialysis in this population [24]. A family member may perform peritoneal dialysis to a dependent elderly patient, but this situation should be considered temporary, and a caregiver should replace him/her in this task in order to avoid family burnout [3, 24, 30, 37].
Kidney transplantation
Successful aging and continuous improvement in medical care have made kidney transplantation possible in a very specific subgroup of very elderly patients [3]. Thus, most transplant centers do not consider a rigid age limit for renal transplantation; instead, they carefully evaluate the patient’s overall physiologic condition and not simply the chronological age in choosing a recipient [43, 44]. Because very elderly patients usually have many comorbid conditions, the pre-transplant assessment (screening for cardiovascular disease, infection, and malignancy) has even higher utility in this age group, and their re-evaluation should be performed more frequently compared with younger ones [3, 45]. A particularly careful screening for the presence and degree of frailty, coronary disease, congestive heart failure, cognitive impairment, and adherence to prescriptions is of paramount importance before working up elderly candidates for transplantation [46–49]. Studies reported that survival rate of well-selected patients over 70 years of age who had a longer life expectancy and better quality of life after kidney transplantation is longer and associated with better quality of life, compared with those on dialysis [3, 50, 51]. In order to optimize kidney allocation, appropriate donor and recipient selection should be based on the concept of matching an older donor with a recipient of comparable age (age-matching transplant), and the allocation of two marginal grafts in order to optimize the number of available functioning glomeruli [3].
Tailored immunotherapy can reduce the risk of infectious complications in the elderly. It seems reasonable to assume that the very elderly would be at higher risk of clinical complications (falls, fractures, and sarcopenia) than younger patients [12, 28, 46]. Therefore, a reduction of the exposure to prednisone has been proposed. Newer immunosuppressant drugs (tacrolimus, mycophenolate, sirolimus, etc.,) can even contribute to decrease corticosteroid dose [3]. Besides, since senile decline of cytochrome P450 activity is responsible for a higher removal of steroids and cyclosporine in elderly people, this phenomenon explains why old patients are more prone to the side effects due to these drugs [42]. Some studies have documented that older patients are less likely to experience allograft rejection compared with younger kidney transplant recipients, except in those cases in which the graft comes from older donors [3, 52, 53]. Conversely, others studies found an increased risk of graft rejection in the elderly [3]. The former finding could be explained by the reduced immune system capability observed in old subjects (immunosenescence), while the latter could be explained by metabolism modifications caused by immunosuppressant drugs in elderly recipients, as it was previously mentioned [3, 12].
Conservative treatment and palliative care
Even when conservative treatment and palliative care used neither dialysis nor renal prevention strategies (angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, etc.), there are marked differences between them [9]. The aim of the conservative treatment was to manage the complications of advanced chronic kidney disease without dialysis. Thus, it constitutes an alternative for handling non-terminal very old patients suffering from end-stage renal disease who are not able to dialyze (neither veins nor peritoneum in adequate status for dialysis) or do not want to do it (patient’s choice). It should be taken into account that about 5 % of aged population refused to start dialysis, and octogenarian patients may not receive dialysis due to lack of dialytic access, extremely frailty (marked dementia or multiple comorbidities), or intolerance to the procedure [9]. Withdrawal from dialysis is more frequent among nursing home dialysis patients, and discontinuation rate in this aged population is associated to social and medical reasons, such as severe dementia or terminal oncologic disease [54]. Many drugs can be used as part of a conservative therapeutic strategy such as loop diuretics (salt and water overload), cationic exchange resins (hyperkalemia), erythropoietin (anemia), bicarbonate (metabolic acidosis), activated charcoal (uremia), calcium supplements (hypocalcemia), and phosphate binders (hyperphosphatemia) [55–58]. Overall, these medications should be prescribed taking into consideration the geriatric principle of trying to avoid polypharmacy in the elderly [12]. Conservative treatment also includes nutritionist counseling (very low protein diet), and psychological support [58, 59]. Palliative treatment is applied to terminal patients, and its goal is to manage patient’s symptoms secondary to advanced chronic kidney disease [9]. This therapeutic strategy includes the use of oxygen (dyspnea), opioids (dyspnea and pain), antiemetics (nausea), anti-pruritic drugs and ointments (itching), anti-inflammatory drugs (pain), levomepromazine (clonus), and psychological support [3, 9, 58, 60].
Frailty and sarcopenia
Frailty and sarcopenia are prevalent comorbidities usually found in very elderly people, particularly in those affected by end-stage chronic renal disease [61–64]. Since both comorbidities have a strong negative impact on health general status, they should be detected early and treated, concomitantly with any of the above-mentioned renal replacement treatments except when a palliative treatment has been implemented [63–65].
Moreover, the degree of frailty in a renal patient can influence on the decision about which modality of renal replacement treatment could represent the best choice [51]. Frailty is a medical syndrome with multiple causes and contributors that is characterized by diminished strength, endurance, and reduced physiologic function that increases an individual’s vulnerability for developing increased dependency and/or death, while sarcopenia is a syndrome characterized by progressive and generalized loss of musculoskeletal mass and strength that occurs with advancing age, which increases the risk of adverse outcomes such as physical disability, poor quality of life, and death [63]. Several mechanisms may be involved in the onset and progression of sarcopenia such as proteolysis, altered neuromuscular integrity, and increased fat content in muscles [64]. Although sarcopenia may be a component of frailty, it is agreed that frailty is more multifaceted than sarcopenia alone, since frailty goes beyond physical factors to encompass psychological and social dimensions [62–64].
In order to diagnose frailty, many tests have been described, but the FRAIL questionnaire is a simple and clinically useful tool (Table 2) [63]. The diagnosis of sarcopenia is based on evaluation of the muscle changes mentioned above: Muscle mass can be assessed by body imaging techniques (computed tomography or magnetic resonance imaging) or bioimpedance analysis (lean body mass), muscle strength can be evaluated by measuring handgrip strength, and physical performance can be assessed by applying clinical test such as the short physical performance battery or timed get-up-and-go test (Table 3) [63, 64]. Therapeutic strategies based on the prescription of low intensity resistance and aerobic physical exercise, adequate caloric and protein intake, vitamin D supplementation, and avoidance of polypharmacy may prevent or delay the onset of frailty and sarcopenia. In order to establish the initial degree of compromise of these syndromes and to be able to monitor the evolution of their treatment, clinical scores have been developed such as the clinical frailty scale and the clinical sarcopenia stages, respectively (Tables 4, 5) [12, 63, 64].
Since the diagnosis and treatment of frailty and sarcopenia is crucial in general geriatrics patients, but there is no current information about this topic in end-stage renal disease oldest old patients, it would be very important to incorporate these evaluations in pre-dialysis, peritoneal dialysis, hemodialysis, and kidney transplant very old patients in order to learn about their impact on these groups.
Conclusion
There are several therapeutic alternatives which can be offered to very elderly patients suffering from end-stage renal disease, such as hemodialysis, peritoneal dialysis, kidney transplant, conservative, or palliative care, taking into consideration their choice of therapy and overall clinical and social status.
References
Ansell D, Feest T, Hodsman A, Rao R, Tomson C, Udayaraj U, Williams A, Warwick G (2007) UK Renal Registry Report 2006. UK Renal Registry, Bristol
Ansell D, Casteldine C, Feehally J, Fogarty D, Ford D, Inward C, Tomson C, Warwick G, Webb L, Williams A (2010) UK Renal Registry Report 2009. UK Renal Registry, Bristol
Somma C, Trillini M, Kasa M, Gentile G (2013) Managing end-stage renal disease in the elderly. Aging Health 9(5):539–552
Musso CG, Macías Nuñez JF (2007) Geriatric nephrology: its principles and aims. Electron J Biomed 2:6–8
Musso CG, Michelangelo H, Reynaldi J, Martinez B, Vidal F, Quevedo M, Parot M, Waisman G, Algranati L (2010) Combination of oral activated charcoal plus low protein diet as a new alternative for handling in the old end-stage renal disease patients. Saudi J Kidney Dial Transplant 21(1):102–104
Port FK, Wolfe RA, Hawthorne VM, Ferguson CW (1989) Discontinuation of dialysis therapy as a cause of death. Am J Nephrol 9(2):145–149
Brown EA, Johansson L (2011) Dialysis options for end-stage renal disease in older people. Nephron Clin Pract 119(Suppl 1):c10–c13
Singh P, Germain MJ, Cohen L, Unruh M (2014) The elderly patient on dialysis. In: geriatric considerations. Nephrol Dial Transpl 29(5):990–996
Jassal SV, Kelman EE, Watson D (2011) Non-dialysis care: an important component of care for elderly individuals with advanced stages of chronic kidney disease. Nephron Clin Pract 119(Suppl 1):c5–c9
Musso CG (2002) Geriatric nephrology and the ‘‘ephrogeriatric giants’’. Int Urol Nephrol 34(2):255–256
Bowling CB, O’Hare AM (2012) Managing older adults with CKD: individualized versus disease-based approaches. Am J Kidney Dis 59(2):293–302
Forciea M, Lavizzo-Mourey R, Schwab E (2000) Geriatric secrets. Hanley & Belfus, Philadelphia
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS (2007) Prevalence of chronic kidney disease in the United States. JAMA 298(17):2038–2047
Disney AP (1995) Demography and survival of patients receiving treatment for chronic renal failure in Australia and New Zealand: report on dialysis and renal transplantation treatment from the Australia and New Zealand Dialysis and Transplant Registry. Am J Kidney Dis 25(1):165–175
Kutner NG, Zhang R, McClellan WM (2000) Patient-reported quality of life early in dialysis treatment: effects associated with usual exercise activity. Nephrol Nurs J 27(4):357–367
Westlie L, Umen A, Nestrud S, Kjellstrand CM (1984) Mortality, morbidity, and life satisfaction in the very old dialysis patient. Trans Am Soc Artif Intern Organs 30:21–30
Crews DC, Scialla JJ, Liu J, Guo H, Bandeen-Roche K, Ephraim PL, Jaar BG, Sozio SM, Miskulin DC, Tangri N, Shafi T, Meyer KB, Wu AW, Powe NR, Boulware LE (2014) Predialysis health, dialysis timing, and outcomes among older United States adults. J Am Soc Nephrol 25(2):370–379
Trigka K, Chouchoulis K, Kaza M, Mpimpi A, Kyritsis I, Musso C, Dousdampanis P (2014) Age, nutrition, and hemodialysis. 51 ERA-EDTA Congress. Abstract
Tattersall J, Greenwood R, Farrington K (1995) Urea kinetics and when to commence dialysis. Am J Nephrol 15:283–289
Ruggenenti P, Perna A, Benini R, Bertani T, Zoccali C, Maggiore Q, Salvadori M, Remuzzi G (1999) In chronic nephropathies prolonged ACE inhibition can induce remission: Dynamic of time-dependent changes in GFR. Investigators of the GISEN Group. Gruppo Intaliano Studi Epidemiologici in Nefrologia. J Am Soc Nephrol 10:997–1006
Canada-USA (CANUSA) Peritoneal Dialysis Study Group (1996) Adequacy of dialysis and nutrition in continuous ambulatory peritoneal dialysis: association with clinical outcomes. J Am Soc Nephrol 7(2):198–207
Cooper BA, Branley P, Bulfone L, Collins JF, Craig JC, Fraenkel MB, Harris A, Johnson DW, Kesselhut J, Li JJ, Luxton G, Pilmore A, Tiller DJ, Harris DC, Pollock CA, IDEAL Study (2010) A randomized, controlled trial of early versus late initiation of dialysis. N Engl J Med 363(7):609–619
Reddy NC, Korbet SM, Wozniak JA, Floramo SL, Lewis EJ (2007) Staff-assisted nursing home haemodialysis: patient characteristics and outcomes. Nephrol Dial Transplant 22(5):1399–1406
Musso CG, Oreopoulos DG (2010) Peritoneal dialysis in the elderly: general aspects. Electron J Biomed 1:6–8
Kurella M, Covinsky KE, Collins AJ, Chertow GM (2007) Octogenarians and nonagenarians starting dialysis in the United States. Ann Intern Med 146(3):177–183
Letourneau I, Ouimet D, Dumont M, Pichette V, Leblanc M (2003) Renal replacement in end-stage renal disease patients over 75 years old. Am J Nephrol 23:71–77
Roake J (2004) Dialysis in the elderly. N Z Med J 117(1195):1–4
Musso CG (2005) Clinical catastrophic events in geriatrics: its physiopathological bases. Electron J Biomed 1:9–12
Tang I, Vrahnos D, Valaitis D, Lau A (1992) Vascular access thrombosis during recombinant human erythropoietin therapy. ASAIO J 38:M528
Dimkovic N, Oreopoulos D (2008) Substitutive treatments of end-stage renal disease in the elderly: dialysis. In: Macías Núñez JF, Oreopoulos D, Cameron S (eds) The ageing kidney in health and disease. Springer, New York, pp 443–463
Didlake R, Raju S, Rhodes R, Bower J (1991) Dialysis access in patients older than 65 years. In: Sommer BG, Henry ML (eds) Vascular access for hemodialysis II. Wall Gore and Associates, Inc., Boston
Olsha O, Hijazi J, Goldin I, Shemesh DJ (2014) Vascular access in hemodialysis patients older than 80 years. Vasc Surg. doi:10.1016/j.jvs
Macías Núñez JF, Musso CG (2013) Nephrogeriatrics. In: d´Hyver de las Deses C (ed) Geriatrics. Manual Moderno, México, pp 443–453
Musso CG, Macías Núñez JF (2006) Feed-back between geriatric syndromes: general system theory in geriatrics. Int Urol Nephrol 38(3–4):785–786
Musso CG, Reynaldi J (2009) Peritoneal dialysis, hemodialysis, and intestinal dialysis in old and very old people. Nefrol Argent 7(3):278–281
Kurella Tamura M, Larive B, Unruh ML, Stokes JB, Nissenson A, Mehta RL, Chertow GM, Frequent Hemodialysis Network Trial Group (2010) Prevalence and correlates of cognitive impairment in hemodialysis patients: the Frequent Hemodialysis Network trials. Clin J Am Soc Nephrol 5(8):1429–1438
Hiramatsu M, Ishida M, Tonozuka Y, Mikami H, Yamanari T, Momoki N, Onishi A, Maruyama K (2012) Application of peritoneal dialysis in elderly patients by classifying the age into young-old, old, and oldest-old. Contrib Nephrol 177:48–56
Wakeen MJ, Zimmerman SW, Bidwell D (1994) Viscus perforation in peritoneal dialysis patients: diagnosis and outcome. Perit Dial Int 14(4):371–377
Bargman JM (1993) Complications of peritoneal dialysis related to increased intraabdominal pressure. Kidney Int Suppl 40:S75–S80
Joshi U, Guo Q, Yi C, Huang R, Li Z, Yu X, Yang X (2014) Clinical outcomes in elderly patients on chronic peritoneal dialysis: a retrospective study from a single center in china. Perit Dial Int 34(3):299–307
Nissensen A, Diaz-Buxo J, Adock A, Nelms M (1990) Peritoneal dialysis in the geriatric patients. Am J Kidney Dis 16:335–338
Musso C, Aguilera J, Otero C, Vilas M, Luna D, de Quirós FG (2013) Informatic nephrology. Int Urol Nephrol 45(4):1033–1038
Scibona P, Angriman F, Vazquez C, Ferreyro B, Perelsztein A, Simonovich V, Jauregui J, Musso CG, Belloso W (2014) Individualization of drug therapy in older people. Rev Clin Gerontol 24:145–157
Tso PL (2014) Access to renal transplantation for the elderly in the face of new allocation policy: a review of contemporary perspectives on “older” issues. Transplant Rev (Orlando). 28(1):6–14
Lenihan CR, Hurley MP, Tan JC (2013) Comorbidities and kidney transplant evaluation in the elderly. Am J Nephrol 38(3):204–211
Karim A, Farrugia D, Cheshire J, Mahboob S, Begaj I, Ray D, Sharif A (2014) Recipient age and risk for mortality after kidney transplantation in England. Transplantation 97(8):832–838
Ismail N, Hakim RM, Helderman JH (1994) Renal replacement therapies in the elderly: Part II. Renal transplantation. Am J Kidney Dis 23(1):1–15
Faravardeh A, Eickhoff M, Jackson S, Spong R, Kukla A, Issa N, Matas AJ, Ibrahim HN (2013) Predictors of graft failure and death in elderly kidney transplant recipients. Transplantation 96(12):1089–1096
Ponticelli C, Podestà MA, Graziani G (2014) Renal transplantation in elderly patients. How to select the candidates to the waiting list? Transplant Rev (Orlando) 28(4):188–192
Li Y, Li J, Fu Q, Chen L, Fei J, Deng S, Qiu J, Chen G, Huang G, Wang C (2013) Kidney transplantation from living related donors aged more than 60 years: a single center experience. Ren Fail 35(9):1251–1254
Toyoda M, Yamanaga S, Kawabata C, Hidaka Y, Inadome A, Arakane F, Uekihara S, Seishi I (2014) Long-term safety of living kidney donors aged 60 and older. Transplant Proc 46(2):318–320
Herrero JC, Gutiérrez E, Martínez A, González E, Morales E, Muñoz MA, Valentín M, Bueno B, Praga M, Hernández E, Morales JM, Rodicio JL, Andrés A (2003) Results of kidney transplantation in recipients over 70 years of age: experience at a single center. Transplant Proc 35(5):1675–1676
Saudan P, Berney T, Leski M, Morel P, Bolle JF, Martin PY (2001) Renal transplantation in the elderly: a long-term, single-centre experience. Nephrol Dial Transplant 16(4):824–828
Markowitz AJ, Rabow MW (2003) Practical considerations in dialysis withdrawal: to have that option is a blessing. JAMA 290(6):815
Musso CG, Reynaldi J, Vilas M, De Miguel R, Imperiali N, Algranati L (2010) Fractional excretion of K, Na and Cl following furosemide infusion in healthy, young and very old people. Int Urol Nephrol 42(1):273–277
Musso CG (2004) Potassium metabolism in patients with chronic kidney disease. Part II: patients on dialysis (stage 5). Int Urol Nephrol 36(3):469–472
Musso CG, Michelangelo H, Reynaldi J, Martinez B, Vidal F, Quevedo M, Parot M, Waisman G, Algranati L (2010) Combination of oral activated charcoal plus low protein diet as a new alternative for handling in the old end-stage renal disease patients. Saudi J Kidney Dis Transpl 21(1):102–104
Brown E, Chambers E, Eggeling C, Watson M (2007) End of life care in nephrology. Oxford University Press, New York
Brunori G, Viola BF, Parrinello G, De Biase V, Como G, Franco V, Garibotto G, Zubani R, Cancarini GC (2007) Efficacy and safety of a very-low-protein diet when postponing dialysis in the elderly: a prospective randomized multicenter controlled study. Am J Kidney Dis 49(5):569–580
Musso CG, Michelangelo H, Reynaldi J, Martinez B, Vidal F, Quevedo M, Parot M, Waisman G, Algranati L (2008) Intestinal dialysis in very old patients. Electron J Biomed 1:77–78
Painter P, Roshanravan B (2013) The association of physical activity and physical function with clinical outcomes in adults with chronic kidney disease. Curr Opin Nephrol Hypertens 22(6):615–623
Jauregui JR, Kecskes C, Patiño O, Musso CG, Galich A, Rodota L (2012) Sarcopenia. A relevant entity in the very elderly. Rev Hops Ital B Aires 32(4):162–168
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, Cesari M, Chumlea WC, Doehner W, Evans J, Fried LP, Guralnik JM, Katz PR, Malmstrom TK, McCarter RJ, Gutierrez Robledo LM, Rockwood K, von Haehling S, Vandewoude MF, Walston J (2013) Frailty consensus: a call to action. J Am Med Dir Assoc 14(6):392–397
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M, European Working Group on Sarcopenia in Older People (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in Older People. Age Ageing 39(4):412–423
Pianta TF, Kutner NG (1999) Improving physical functioning in the elderly dialysis patient: relevance of physical therapy. ANNA J 26(1):11–14
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Musso, C.G., Trigka, K., Dousdampanis, P. et al. Therapeutic alternatives and palliative care for advanced renal disease in the very elderly: a review of the literature. Int Urol Nephrol 47, 647–654 (2015). https://doi.org/10.1007/s11255-014-0886-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-014-0886-8