Abstract
Purpose
Because most population-based studies on the epidemiology of chronic kidney disease (CKD) are cross-sectional, there is, except for end-stage renal disease, hardly any information on incidence rates.
Methods
We conducted a retrospective cohort study in a dynamic population, using data of 784,563 adult participants retrieved from the Integrated Primary Care Information database, a primary care database containing the complete electronic longitudinal medical records. CKD (both incidence and prevalence) was based on (1) an increased urine albumin-to-creatinine ratio, (2) a decreased estimated glomerular filtration rate, or (3) explicit statement in the medical record. Results were stratified by age according to the WHO standard population, sex, and diabetes mellitus.
Results
Based on a single measurement only, the incidence rate of CKD in adults was 1,213 per 100,000 person-years, and 6.7 percent of the adult population had a prevalent diagnosis of CKD. The incidence rate increased by age and was the highest in participants with diabetes with an incidence of 25,000 per 100,000 person-years, affecting over 75 percent of participants with diabetes.
Conclusions
This is the first study to report the incidence rates of all stages of CKD for the entire adult population, stratified by sex, 5-year age groups, and diabetes. Our data demonstrate that the incidence of CKD increases with age and is the highest in participants with diabetes mellitus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
The prevalence of chronic kidney disease (CKD) has been widely studied in population-based, cross-sectional studies, with marked heterogeneity in prevalence data ranging from 19 to 71 percent for the highest age category [1–3], probably due to selection bias [4]. Limited information is available on (age-specific) incidence rates for CKD [2, 5–13].
Chronic kidney disease is associated with an increased risk of hospitalization, cardiovascular, and all-cause mortality and constitutes a major health problem with substantial healthcare costs [14–18]. A recent meta-analysis showed that the relative risk of mortality, stratified by estimated glomerular filtration rate (eGFR), is similar in those with and without diabetes [19]. This suggests that the underlying CKD is an important predictor for mortality. Another meta-analysis reported a similar pattern in participants with hypertension emphasizing the importance of CKD as a predictor of clinical outcomes [19–21].
Objective
The objective of this study was to investigate the epidemiology, in particular the incidence, of CKD using prospectively gathered electronic health care records from a community-dwelling adult population. We studied the incidence and prevalence of CKD in the adult population stratified by sex, 5-year age categories (WHO standard population) [22], and the presence of diabetes mellitus.
Methods
Setting
All data were retrieved from the Integrated Primary Care Information (IPCI) project, a longitudinal observational, dynamic database which contains the electronic medical records of a group of 150 general practitioners (GPs) in the Netherlands. In the Dutch health care system, the GP plays a pivotal role and acts as a gatekeeper of medical care and information. Almost all inhabitants of the Netherlands are registered with a GP, independent of their health status. In the Dutch health care, the GP has a crucial role and functions as gatekeeper for care. This implies that only the GP can refer the patient to a specialist and that there is a strong communication between the GP and the specialist. With CKD, the GP is responsible for diagnosis, evaluation, treatment, and follow-up, unless the patient should be referred to a specialist, as documented in the national interdisciplinary referral agreement [23]. Patients should be referred with macro-albuminuria, an eGFR < 45 ml/min/1,73 m2 with age < 65 years, an eGFR < 30 ml/min/1,73 m2 with age > 65 years, or when an underlying renal disease is suspected. Details of the IPCI database have been described elsewhere [24, 25]. Briefly, the database contains the complete electronic medical records of approximately 1,000,000 participants. These records contain anonymous longitudinal data on demographics, symptoms and diagnoses (coded and in free text), referrals, laboratory findings, hospitalizations, discharge letters, and drug prescriptions (inclusive indication and dosage regimen). To maximize completeness of the data, GPs participating in the IPCI project are not allowed to maintain a system of paper-based records besides the electronic medical records. The system complies with European Union guidelines on the use of data for medical research and has been proven valid for pharmaco-epidemiologic studies [25]. The scientific and ethical advisory board of the IPCI project approved the study.
Study design
Retrospective cohort study in a dynamic population.
Participants
The source population comprised all adults (20 years or older) who were registered with their GP for at least 365 days. The study period started on January 1, 1996 and ended on March 1, 2011. Participants with (a history of) a renal transplant prior to study entry were excluded. Participants were followed until renal transplant, death, transfer out of practice, last data drawdown, or end of the study period, whichever came first.
Outcome
Chronic kidney disease was based on abnormalities in estimated glomerular filtration rate (eGFR), albuminuria as a marker of kidney damage, or an explicit statement in the medical record, and stratified by stages 1–5 [26]. The eGFR was obtained from the equation published by the Chronic Kidney Disease Epidemiology (CKD-EPI) Collaboration [27]:
where Scr is serum creatinine (mg/dl), κ is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min indicates the minimum of Scr/κ or 1, and max indicates the maximum of Scr/κ or 1.
For the urine albumin-to-creatinine ratio (ACR), we used a cutoff of 3.5 mg/mmol (~30 mg/g) for women and 2.5 mg/mmol (~22 mg/g) for men for (micro-) albuminuria as a marker for kidney damage to define stages 1 and 2 of CKD. The last eGFR before the ACR measurement was used to distinguish between stages 1 and 2 of CKD. If no SCR measurement was available, the eGFR was assumed to be >90 ml/min/1.73 m2.
In addition, the complete electronic medical record was screened for an explicit statement indicating CKD, using an algorithm including “kidney/renal” in combination with “insufficiency/failure”, “renal replacement therapy”, “dialysis”, and “transplantation”.
A definite diagnosis of CKD was made according to KDIGO guidelines if there were two measurements, at least 90 days apart, indicating either (micro-) albuminuria or eGFR < 60 ml/min/1.73 m2, or two explicit statements in the medical record (at least 90 days apart) indicating CKD. The first date was used as index date. A “possible diagnosis” was based on a single abnormal measurement or explicit statement indicating CKD in the medical record. Participants with a statement in the medical record indicating CKD before the start of follow-up that could not be confirmed by subsequent measurements were excluded from the stage-specific analysis. Participants with a statement in the medical record indicating CKD after start of follow-up that could not be confirmed by subsequent measurements were not accounted, and follow-up was censored from that date. The following stages were used: stage 1 “eGFR ≥ 90 ml/min/1.73 m2 with kidney damage”, stage 2 “eGFR 60–89 ml/min/1.73 m2 with kidney damage”, stage 3 “eGFR 30–59 ml/min/1.73 m2”, stage 4 “eGFR 15–29 ml/min/1.73 m2”, stage 5 “eGFR < 15 ml/min/1.73 m2 or dialysis” [28].
Diabetes mellitus
Because diabetes is a risk factor for the development of end-stage renal disease (ESRD), we stratified our analyses by underlying diabetes [14–16]. The diagnosis of diabetes was based on a prescription of a drug within the World Health Organization (WHO) Anatomical Therapeutic Chemical (ATC) classification system “A10” (drugs used in diabetes) [29].
Statistical analysis
The incidence rate was determined by dividing the number of cases by the total number of person-years of follow-up. Participants were censored on the date of first diagnosis for the respective disease stage. Overall incidence rates were calculated for the adult study population. Incidence rates were expressed per 100,000 person-years. Ninety-five percent confidence intervals were calculated based on a Poisson distribution [30].
Prevalence was determined by dividing the number of cases by the number of persons with follow-up in the study population on January 1 of each calendar year. Cases included participants with a prevalent diagnosis or an incident diagnosis of CKD prior to the 1st of January. As CKD is a progressive disease, participants were allowed to move between stage-specific categories of CKD. Results displayed were weighted for the calendar year-specific denominator. Ninety-five percent confidence intervals were calculated based on normal distribution.
The results on the incidence and prevalence of CKD were stratified for age according to the WHO standard population, sex, and presence of diabetes mellitus [31].
Results
The source population consisted of 784,856 adult participants with a valid history of at least 365 days in the IPCI database. A total of 293 participants were excluded because of a history of a renal transplant prior to start of follow-up, leaving 784,563 participants available for analysis.
The median age of the study population was 44.4 years at the start of follow-up [interquartile range (IQR) 31.7–59.2 years]; 48.1 % were males and 4.3 % of participants had a diagnosis of diabetes. A total of 2.1 million person-years of follow-up were available for the study population, the maximal duration of follow-up being 10.7 years, with a median of 2.3 years (IQR 1.3–3.4 years). Detailed population characteristics are available (online table 1 and 2).
For the study population, 1,379,097 eGFR measurements and 178,425 ACR measurements were available. A total of 42,780 participants had evidence of CKD prior to the start of follow-up; of these, 41,343 participants had an abnormal measurement, and in an additional 1,437 participants, the presence of CKD was explicitly stated in the medical record with no measurement available prior to the start of follow-up. There were 23,643 incident cases of CKD; of these, 22,722 were based on abnormal measurements, and an additional 921 cases were based on explicit statements in the medical record.
Incidence of CKD
The overall incidence of a possible diagnosis of CKD in adults was 1,213 per 100,000 person-years (95 % CI 1,198–1,283 per 100,000 person-years). The overall incidence rates for stages 1–5 CKD were 205, 11, 859, 41, and 24 per 100,000 person-years. The overall incidence of a definite diagnosis of CKD was 479 per 100,000 person-years (95 % CI 470–489 per 100,000 person-years). The overall incidence rates for stages 1–5 CKD were 60, 5, 370, 25, and 18 per 100,000 person-years. Confirmation of the first incident abnormal SCR or ACR measurement by a subsequent abnormal measurement (as required for definite diagnosis of CKD) was obtained after a median of 301 days (interquartile range 148–444 days).
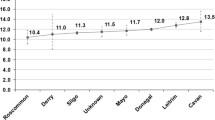
For a possible diagnosis, the incidence rate was higher in females (1,362 per 100,000 person-years) than in males (1,029 per 100,000 person-years), p < 0.001. The incidence rates were higher in participants with diabetes (7,120 per 100,000 person-years) than in those without (973 per 100,000 person-years; p < 0.001). The highest incidence rate of CKD was reached in women with diabetes, aged ≥ 85 years (25,000 per 100,000 person-years). Results stratified by age, sex, and diabetes are shown in Fig. 1 and Table 1. There was a marked increase in the incidence rate for stages 3 and 4 CKD as of the age of 50 years and older, both in participants with and without diabetes, whereas the incidence rate of stage 2 CKD only increased with age in participants with diabetes. (Figures 2a–e) Comprehensive stage-specific tables are available (online tables 3A-E).
Prevalence of CKD
The overall prevalence of CKD (possible diagnosis) was 6.7 % (95 CI % 6.6–6.7 %) and 0.55, 0.03, 5.38, 0.41, 0.16 % for stages 1–5. The overall prevalence of CKD (definite diagnosis) was 5.1 % (5.1–5.1 %) and 0.32, 0.03, 4.17, 0.38, 0.15 % for stages 1–5. In line with the incidence data, the prevalence of CKD increased with age, female sex, and diabetes to more than 75 % in diabetic female participants aged ≥ 85 years as shown in Table 2 and Fig. 3. Prevalence of all stages of CKD, except for stage 1, increased with age (Fig. 4a–e). In participants with diabetes, the prevalence of stages 1 and 2 CKD was higher in males. In participants without diabetes, stage 5 CKD was significantly more prevalent in males than in females from the age of 75 onward (Fig. 4e). Irrespective of the presence of diabetes, the prevalence of stage 3 CKD was higher in females than in males for all age groups. Comprehensive stage-specific tables are available (online tables 4A–E).
Discussion
This is the first study to report incidence rates of CKD for the entire community-dwelling adult population for stages 1–5 of CKD, stratified by sex, 5-year age groups, and diabetes. The overall incidence of CKD in adults in our study was 1,213 per 100,000 person-years. The incidence rate increased with age and was the highest in females and in participants with diabetes mellitus. Indeed, in female diabetic participants, the incidence rate was close to 25,000 per 100,000 person-years. For stage 1 of CKD—especially in participants with diabetes—the prevalence decreased with advancing age, despite an increase in incidence rate, possibly due to a more rapid decline in eGFR with reclassification to prevalent stage 3 of CKD or excess mortality. Strengths of our data are the population-based setting, large sample size, and the use of laboratory data to define CKD. In addition, the risk of selection bias is unlikely as almost all inhabitants of the Netherlands are registered with a GP, and data are collected as part of routine patient care, irrespective of any research questions.
As for all observational research, our study has potential limitations as well. Diagnostic bias might be a concern as laboratory results were taken in the process of day-to-day patient care—in asymptomatic participants, this could imply that the incidence and prevalence of CKD are underestimated as no laboratory results were available. Individual laboratory data on analysis technique and calibration were not available. Estimated GFR might not adequately reflect actual GFR, especially in those with diabetes [32–39]. In that respect, our data reflect clinical practice because there is no general accepted formula to estimate GFR from serum creatinine with adjustment for diabetes at this point in time. In addition, potential misclassification is reported to be limited for GFR < 90 ml/min/1.73 m2 [32]. Finally, participants with stages 4 and 5 CKD are detected; however, for those referred to the specialist, limited data on disease progression, with the exception of dialysis and transplant, are available after initial diagnosis. Therefore, it is not possible to confirm whether all patients indeed progressed to end-stage renal disease.
Few studies have reported incidence rates for CKD in the general population [5–13]. Comparison of incidence rates in our study with results of these studies is difficult, because these used a different case definition of CKD. The overall prevalence of our study is in line with the findings from previous cross-sectional studies, although there is substantial heterogeneity among these studies as well, with reported prevalence rates of 19–71 percent in the older age categories (Table 3) [2]. In prospective studies, where data are progressively collected during the study period, it is possible to confirm a first abnormal measurement (indicating CKD), with a second abnormal measurement (“definite diagnosis”) within a reasonable time. In our study population that reflects day-to-day clinical practice, a first abnormal measurement is followed by a second measurement only after a median 301 days (IQR 148–444 days), and it might be missing completely as a result of referral to a specialist. Therefore, the use of a definite diagnosis of CKD likely underestimates the real values in a population-based study.
In conclusion, this study is the first to report incidence rates for stages 1–5 of CKD stratified by age, sex, and diabetes. Our results are expected to be generalizable to a western, predominantly Caucasian population, although differences in nationally implemented clinical guidelines, health care policy, and reimbursement might contribute to divergent findings in other countries. It shows that CKD is a major health problem, which affects the majority of the population at older age, especially in those with diabetes.
References
McClellan W et al (2006) Racial differences in the prevalence of chronic kidney disease among participants in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Cohort Study. J Am Soc Nephrol 17(6):1710–1715
Zhang QL, Rothenbacher D (2008) Prevalence of chronic kidney disease in population-based studies: systematic review. BMC Public Health 8:117
Hallan SI et al (2006) International comparison of the relationship of chronic kidney disease prevalence and ESRD risk. J Am Soc Nephrol 17(8):2275–2284
Strandhagen E et al (2010) Selection bias in a population survey with registry linkage: potential effect on socioeconomic gradient in cardiovascular risk. Eur J Epidemiol 25(3):163–172
Collins G, Altman D (2012) Predicting the risk of chronic kidney disease in the UK: an evaluation of QKidney(R) scores using a primary care database. Br J Gen Pract 62(597):e243–e250
Drey N et al (2003) A population-based study of the incidence and outcomes of diagnosed chronic kidney disease. Am J Kidney Dis 42(4):677–684
Tohidi M et al (2012) Incidence of chronic kidney disease and its risk factors, results of over 10 year follow up in an Iranian cohort. PLoS One 7(9):e45304
Nagai K et al (2013) Annual incidence of persistent proteinuria in the general population from Ibaraki annual urinalysis study. Clin Exp Nephrol 17(2):255–260
Liu JH et al (2012) The risk for chronic kidney disease in patients with heart diseases: a 7-year follow-up in a cohort study in Taiwan. BMC Nephrol 13:77
Butt AA, Wang X, Fried LF (2011) HCV infection and the incidence of CKD. Am J Kidney Dis 57(3):396–402
Evans K et al (2011) Race differences in access to health care and disparities in incident chronic kidney disease in the US. Nephrol Dial Transplant 26(3):899–908
Zoppini G et al (2009) Higher HDL cholesterol levels are associated with a lower incidence of chronic kidney disease in patients with type 2 diabetes. Nutr Metab Cardiovasc Dis 19(8):580–586
Yamagata K et al (2007) Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int 71(2):159–166
Nitsch D et al (2013) Associations of estimated glomerular filtration rate and albuminuria with mortality and renal failure by sex: a meta-analysis. BMJ 346:f324
Go AS et al (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351(13):1296–1305
Roderick PJ et al (2009) CKD and mortality risk in older people: a community-based population study in the United Kingdom. Am J Kidney Dis 53(6):950–960
Nitsch D et al (2011) CKD and hospitalization in the elderly: a community-based cohort study in the United Kingdom. Am J Kidney Dis 57(5):664–672
Kerr M et al (2012) Estimating the financial cost of chronic kidney disease to the NHS in England. Nephrol Dial Transplant 27(3 Suppl):Iii73–Iii80
Fox CS et al (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 380(9854):1662–1673
Naud J et al (2012) Current understanding of drug disposition in kidney disease. J Clin Pharmacol 52(1 Suppl):10S–22S
Mahmoodi BK et al (2012) Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without hypertension: a meta-analysis. Lancet 380(9854):1649–1661
Ahmad OB, et al. (2001) Age standardization of rate: a new WHO standard. [cited 2013 21 Feb 2013]; Available from: http://www.who.int/healthinfo/paper31.pdf
De Grauw WJC, K.H., Bilo HJG, Faber EF, Flikweert S†, Gaillard CAJM, Labots-Vogelesang SM, Verduijn MM, Verstappen WHJM, Vleming LJ, Walma EP, Van Balen, JAM. (2009) Landelijke Transmurale Afspraak Chronische nierschade (National Interdisciplinary Referral Agreement Chronic Kidney Disease). Huisarts en Wetenschap (12): pp. 586–597
Vlug AE et al (1999) Postmarketing surveillance based on electronic patient records: the IPCI project. Methods Inf Med 38(4–5):339–344
van der Lei J et al (1993) The introduction of computer-based patient records in The Netherlands. Ann Intern Med 119(10):1036–1041
K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis, 2002. 39(2 Suppl 1): p. S1–266
Levey AS et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
KDIGO clinical practice guideline for the diagnosis, evaluation, prevention, and treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int Suppl 2009(113): pp S1–130
Hvidberg E, Andersen AH (1980) New classification of drugs. The Medical list and the Drug catalogue are introduced in Anatomical–Therapeutic–Chemical classification code (ACT-code) in 1981. Ugeskr Laeger 142(6):396–397
Rothman KJGS (1998) Modern epidemiology, 2nd edn. Lipincott and W.a.W, Philadelphia
Population WS; Available from: http://www.who.int/healthinfo/paper31.pdf
Stevens LA et al (2010) Development and validation of GFR-estimating equations using diabetes, transplant and weight. Nephrol Dial Transplant 25(2):449–457
Camargo EG et al (2011) The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is less accurate in patients with Type 2 diabetes when compared with healthy individuals. Diabet Med 28(1):90–95
Drion I et al (2011) The Cockcroft-Gault: a better predictor of renal function in an overweight and obese diabetic population. Obes Facts 4(5):393–399
Iliadis F et al (2011) Glomerular filtration rate estimation in patients with type 2 diabetes: creatinine- or cystatin C-based equations? Diabetologia 54(12):2987–2994
Nair S, Hardy KJ, Wilding JP (2011) The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula performs worse than the Modification of Diet in Renal Disease (MDRD) equation in estimating glomerular filtration rate in Type 2 diabetic chronic kidney disease. Diabet Med 28(10):1279
Rognant N et al (2011) Performance of the chronic kidney disease epidemiology collaboration equation to estimate glomerular filtration rate in diabetic patients. Diabetes Care 34(6):1320–1322
Silveiro SP et al (2011) Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation pronouncedly underestimates glomerular filtration rate in type 2 diabetes. Diabetes Care 34(11):2353–2355
Trimarchi H et al (2012) Creatinine- vs. cystatin C-based equations compared with 99mTcDTPA scintigraphy to assess glomerular filtration rate in chronic kidney disease. J Nephrol 25(6):1003–1015
Viktorsdottir O et al (2005) Prevalence of chronic kidney disease based on estimated glomerular filtration rate and proteinuria in Icelandic adults. Nephrol Dial Transplant 20(9):1799–1807
Coresh J et al (2005) Chronic kidney disease awareness, prevalence, and trends among U.S. adults, 1999 to 2000. J Am Soc Nephrol 16(1):180–188
Nitsch D et al (2006) Prevalence of renal impairment and its association with cardiovascular risk factors in a general population: results of the Swiss SAPALDIA study. Nephrol Dial Transplant 21(4):935–944
Cirillo M et al (2006) Low glomerular filtration in the population: prevalence, associated disorders, and awareness. Kidney Int 70(4):800–806
Brown WW et al (2003) Early detection of kidney disease in community settings: the Kidney Early Evaluation Program (KEEP). Am J Kidney Dis 42(1):22–35
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first author works for the Medicine Evaluation Board, the drug regulatory agency in the Netherlands.
The views expressed in this article are the personal view of the author and may not be understood or quoted as being made on behalf of or reflecting the position of the regulatory agency.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
van Blijderveen, J.C., Straus, S.M., Zietse, R. et al. A population-based study on the prevalence and incidence of chronic kidney disease in the Netherlands. Int Urol Nephrol 46, 583–592 (2014). https://doi.org/10.1007/s11255-013-0563-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-013-0563-3