Abstract
Purpose
The study of online hemodiafiltration (HDF) benefits over high-flux hemodialysis (HD) raises great interest. The purpose was to compare clinical and laboratory parameters in patients treated with HD who were switched to HDF.
Methods
Forty-eight HD patients (study group) were switched to HDF, while other 521 patients remained on HD as a control group. During last 6 HD months and during first year of HDF, we determined in both groups the following parameters: monthly–weekly dialysis time, systolic and diastolic blood pressure, body mass index (BMI), interdialytic body weight gain (IBWG), blood flow rate (Qb), weekly erythropoietin-stimulating agents dose (EPO), single-pool Kt/V, calcium, phosphorus (P), hemoglobin and normalized protein catabolic ration (nPCR), plus every 3 months—albumin, parathormone (PTH), ferritin and transferrin saturation (TSAT). In both groups, parameters in the last 6 HD months were compared to those in the first 6 months and, respectively, to those in the first year of HDF.
Results
In the study group, albumin and nPCR were significantly higher in the HD period not only compared to the first 6 months of HDF, but also compared to the first year of HDF. IBWG and P were higher with HD compared to the first year of HDF, but not with the first 6 months. PTH, Kt/V, Qb and EPO were higher in both HDF periods. In the control group, albumin was significantly higher in the first 6 months after the switch, but it was significantly lower in the first year. BMI, ferritin, PTH, Kt/V, Qb, TSAT and weekly dialysis time were higher in both HDF periods, while nPCR, EPO, SBP and DBP were lower. IBWG and Hb rose only during the first year after the switch, while P was lower in the first year, but not in the first 6 months.
Conclusions
Nutrition, assessed by albumin, nPCR and BMI, was not improved by HDF compared to HD. With HDF, Kt/V and phosphorus control were better, similar results were observed in the control group. A larger EPO dose was needed with HDF for maintaining a similar hemoglobin level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Standard hemodialysis provides excellent small molecule clearance, but mortality remains high in the dialysis population. The residual uraemic syndrome that is inadequately cleared by diffusion is thought to contribute to the poor outcome of maintenance dialysis patients [1]. Development of high-flux membranes has allowed higher ultrafiltration rates over 20 ml/h/mmHg per m2, favoring convection, while being thin enough to permit diffusion. Increasing recognition that “middle molecules” contribute to morbidity has fueled the development of techniques to enhance their clearance [2]. Online hemodiafiltration (HDF) combines diffusion and convection, involving large convective volumes that are generated by high-flux membranes and replaced with substitution fluid using ultrapure dialysis fluid [3]. Several studies have been completed comparing survival in HDF versus low-flux [4] and high-flux hemodialysis [5]. At this moment, there is no clear proved benefit of HDF on all-cause mortality and cardiovascular events compared to low-flux and high-flux hemodialysis. Recent evidence showed a beneficial effect of survival among patients who receive high-volume hemodiafiltration [4].
Emerging evidence suggests that HDF may be superior to classic diffusive hemodialysis in terms of patient morbidity [6]. Reduced hypotension during HDF has been reported [7]. HDF and also high-flux hemodialysis (HD) were associated with improved nutritional status and sustained reductions in pretreatment beta 2 microglobulin levels; however, the decrease was greater with HDF [1]. On short term, HDF may improve phosphate control compared to HD [8] and it could enhance the response to erythropoietin-stimulating agents (EPO) [9]. These outcomes were not universal, as there are studies which did not find significant improvement for HDF compared to HD in terms of intradialytic blood pressure control [10], nutritional status and EPO responsiveness [11].
This study compared HD and HDF by assessing some clinical (predialytic blood pressure, body mass index and interdialytic body weight gain, EPO dose) and laboratory features (parameters of nutrition, anemia, phosphocalcic metabolism and dialysis efficiency), in a group of HD patients who was switched to HDF.
Subjects and methods
This was a retrospective, multicenter and observational study which included hemodialysis patients from 7 Romanian dialysis centers.
Inclusion criteria
All patients on regular thrice-weekly high-flux hemodialysis treatment for at least 6 months using a native arterio-venous fistula or a synthetic graft as a vascular access for hemodialysis.
Exclusion criteria
Patients with acute clinical conditions requiring hospitalization, patients with missing clinical or laboratory data during any month of the study period (18 months), patients requiring a central venous catheter as a vascular access for hemodialysis and patients with parathyroidectomy during the study period.
A total of 580 patients respected the inclusion and the exclusion criteria. The patients were treated with bicarbonate-buffered high-flux hemodialysis using polysulphone, synthetic, high-flux dialyzers (Fresenius Medical Care, Bad Homburg, Germany) and polyamide, synthetic, high-flux dialyzers (Gambro AB, Stockholm, Sweden). The dialyzers prescription was driven by body weight (BW): if BW < 50 kg, then the dialyser surface used was 1.4 m2; if BW was between 50 and 70 kg, then the dialyser surface was between 1.7 and 1.9 m2 and if BW > 70 kg, then the dialyser surface was between 1.9 and 2.2 m2. The treatment time was at least 240 min/dialysis session, 3 times per week. Water quality was regularly monitored to ensure tight bacteriologic standards (total viable count <0.1 cfl/ml and endotoxin level <0.03 EU/ml).
Each dialysis center had the possibility to perform online hemodiafiltration to a maximum of 7 % of the total number of dialysis patients in the center. During a 3-month period of time, 59 patients out of 580 were switched to online postdilution hemodiafiltration (HDF). Patients who started HDF were selected based on common selection criteria for all the 7 dialysis centers involved. All patients respected at least one online hemodiafiltration inclusion criteria as stated by the National Health Insurance House of Romania (a) eKt/V ≤ 1.4 and phosphate > 5.5 mg/dl for 3 consecutive months; (b) young patients with increased survival chance in dialysis but with low chance of renal transplantation; (c) patients with uremic polyneuropathy despite efficient hemodialysis treatment; (d) patients with cardiovascular comorbidities or with diabetes mellitus. Out of 59 patients switched to HDF, 11 were not on HDF after 12 months (3 patients refused to continue HDF, 3 patients followed renal transplantation and 5 patients moved to other dialysis facilities). These remaining 48 HDF patients were considered as the study group. A mean substitution fluid volume of 21.6 l per session was used. The HDF treatment time and the dialyzers prescription with regard to body weight were similar as for high-flux hemodialysis period. Only polysulphone dialyzers were used for HDF.
The remaining 521 patients continued to be treated with high-flux hemodialysis and they were considered as the control group.
For patients in the study group, in the last 6 months of high-flux HD and the first 12 months of HDF, we assessed, on monthly basis (first midweek dialysis of each month), presession systolic blood pressure (SBP), presession diastolic blood pressure (DBP), body mass index (BMI), interdialytic body weight gain (IBWG), blood flow rate (Qb), weekly erythropoietin-stimulating agents dose (EPO), spKt/V–K/DOQI formula, total serum calcium (Ca), serum phosphate (P), hemoglobin (Hb) and normalized protein catabolic ratio (nPCR). Every 3 months (first midweek dialysis of the month), albumin, intact parathormone (PTH), ferritin and transferrin saturation (TSAT) were determined. The same clinical and laboratory parameters were determined, respecting the same schedule, for the patients in the control group.
In the study group, a pooled mean of the patient’s parameters in the last 6 months of HD before switching to HDF were compared to a pooled mean of the parameters in the first 6 months of HDF and, respectively, with a pooled mean of the parameters in the first 12 months of HDF. In the control group, a pooled mean of the patient’s results in the last 6 months before the switch to HDF in the study group was compared to a pooled mean of the parameters in the first 6 months after the switch and, respectively, with a pooled mean of the parameters in the first 12 months after the switch.
The treatment for anemia with iron and erythropoietin-stimulating agents and the treatment for mineral bone disease–chronic kidney disease with phosphate binders (calcium-containing and non-calcium-containing) and vitamin D derivates were administered as needed, following the same targets and principles during both HD and HDF periods of time. All centers were part of the same dialysis network, and common medical targets and treatment protocols were used for anemia, mineral bone disease, dialysis efficiency, blood pressure and nutrition. There was no treatment with ketoanalogs during the study period.
The study protocol was approved by the Ethics Committee of the involved centers.
Statistical analysis
Variables were expressed as mean ± standard deviation. A p value <0.05 was considered to be statistically significant. Student’s t-test for independent samples and Wilcoxon’s test for independent samples were applied for analysis of the results. All statistical calculations were made using the statistical software Rcmdr Version 1.6-0.
Results
The study group
In the study group, there were 32 men (66.66 %) and 12 women (33.33 %). The mean age was 44 years, and the mean dialysis vintage was 60 months. The following were causes of end-stage renal disease in the studied population: glomerulonephritis (n = 19; 40 %), diabetic nephropathy (n = 7; 15 %), nephroangiosclerosis (n = 3; 6 %) and others (n = 19; 39 %).
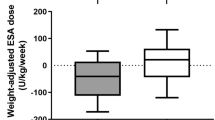
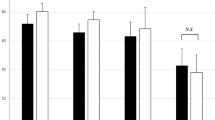
Albumin and nPCR were significantly lower at 6 and at 12 months of HDF compared to last 6 months of HD, while Kt/V, Qb, PTH and EPO were significantly higher (Table 1). IBWG was significantly lower during the first 12 months of HDF, but not during the first 6 months of HDF, compared to the last 6 months of HD (Table 1). P was not significantly lower during the first 6 HDF months compared to the last 6 HD months, but it decreased significantly during the first year of HDF compared to the same HD period (Table 1). The other studied parameters did not vary significantly during the first 6 and 12 months of HDF when compared to the last 6 months of HD.
The control group
In the control group, there were 289 men (55.5 %) and 232 women (44.5 %). The mean age was 56 years old, and the mean dialysis vintage was 59 months. The causes of end-stage renal disease in the control group were glomerulonephritis (n = 160; 31 %), diabetic nephropathy (n = 46; 9 %), nephroangiosclerosis (n = 37; 7 %) and others (n = 276; 53 %).
Albumin was significantly higher in the first 6 months after the switch, but it was significantly lower in the first year after the switch (Table 2). BMI, ferritin, PTH, Kt/V, Qb, TSAT and weekly dialysis time were significantly higher in the first 6 months, but also in the first 12 months after the switch (Table 2). nPCR, EPO, SBP and DBP were lower in the first 6 months and in the first 12 months compared to the last 6 months before the switch to HDF in the study group (Table 2). IBWG and Hb rose during the first year, but not during the first 6 months after the switch, while P was lower in the first year, but not in the first 6 months (Table 2).
Discussion
In this long-term study, we compared high-flux hemodialysis and online postdilution hemodiafiltration regarding a wide variety of clinical and laboratory parameters. We found that albumin level and nPCR were higher in HD compared to the first 6 months of HDF but also compared to the first 12 months of HDF. In the control group, albumin and nPCR were also lower in the first 12 months after the switch to HDF in the study group, compared to the last 6 months before the switch. These results do not show a role for HDF in influencing these nutritional markers. Albumin level reduction with HDF was also observed by other authors [8, 12, 13], but without having a clear clinical relevance. Combarnous et al. [14] studied the albumin loss with predilutional HDF, probably secondary to an interaction with the polymer (polyethersulfone membrane) surface. Albumin loss during HDF seemed to have no acute impact on plasma albumin. Several other studies did not prove a significantly difference between serum albumin levels in patients treated with HD versus patients treated with HDF [2, 11]. Although HDF has been reported to improve nutritional intake [15], this was not confirmed in our study by an increase in BMI in the first 12 months of HDF compared to HD period. More, the patients in the control group which continued on HD had an increase in BMI in both evaluation periods.
There was no significant variation in presession systolic and diastolic blood pressure in HD months compared to HDF months, while, in the control group, SBP and DBP were lower. A small elevation in arterial blood pressure has been described with convective HD treatment [16] and in one study presession diastolic blood pressure measured in upright position became slightly elevated in HDF compared to HD, hypothesizing a better baroreceptor sensibility with HDF [1].
HDF has been reported to remove phosphate more efficiently than HD [1, 17–19]. Recently published data from an ongoing large trial support the hypothesis that HDF is superior to HD regarding phosphate control [8]. In our study, phosphate was significantly decreased by HDF compared to HD during the first 12 months, but not during the first 6 months of HDF. The same pattern was seen in the control group, and this makes it difficult to conclude that HDF is better in removing phosphate than HD. PTH increased in both groups in every period of evaluation compared to the last 6 months before the switch to HDF, probably as a result of mineral bone disease aggravation. In most of the studies comparing HDF with high-flux hemodialysis, PTH did not differ significantly [2, 20]. In the same papers, as in ours, serum calcium also did not differ between HD and HDF. There is one study showing improved PTH values in patients switching from low-flux HD to HDF, along with better phosphate levels [21], suggesting the superiority of HDF compared to HD in terms of controlling mineral metabolism in dialysis patients.
A better management of anemia with HDF compared to HD is still controversial. The superiority of HDF compared to low-flux hemodialysis was observed by Bonforte et al. [9] who concluded that HDF allows considerable anemia correction in patients without EPO treatment, while it significantly reduces EPO doses in those on EPO treatment as compared with standard hemodialysis. Other studies comparing HDF with HD did not find a significantly difference in terms of EPO responsiveness [11] or hemoglobin level [2]. In our study, the hemoglobin level did not differ between HD period and HDF period, but EPO requirements were significantly higher with HDF in the first 6 month, but also in the first 12 months. In the control group, despite the fact that Hb was significantly higher during the first year after the switch, EPO dose was significantly lower. This could be explained by the elevation in ferritin and TSAT in this group, suggesting the role of iron treatment in correcting anemia. This seems to be in conflict with the results of Vaslaki et al. [22] who found a higher hematocrit at a comparable EPO dose in patients switched from HD to HDF. In our study, a possible explanation for the higher EPO consumption observed with HDF could be the clotting of the blood in tubing and dialyzers, as more anticoagulation is needed with HDF. TSAT and ferritin were similar during both HD and HDF periods. This result is not supported by Lin et al. [23] who reported lower ferritin levels and better iron utilization with HDF.
Dialysis efficiency expressed by Kt/V was significantly improved by HDF in the first 6 months, but also in the first 12 months compared to HD. It is not clear whether this is entirely secondary to the higher convection volumes used for HDF, since Qb used for HDF treatments was significantly higher compared to HD. An improvement in Kt/V was observed in the control group, along with increases in weekly dialysis time and Qb. There are several studies which argue for a benefit of HDF compared to HD regarding an improved Kt/V [1, 21], but there are also papers showing no difference between the two renal replacing therapies [2, 11]. High-efficiency HDF resulted in enhanced removal and lower basal levels of small, medium-sized and protein-bound solutes compared to low-flux hemodialysis in the study of Pedrini et al. [24]. Postdilution HDF in comparison with HD provided significant reduction in predialysis concentration of protein-bound compounds, especially those with the highest protein binding, and of beta(2)-microglobulin. For water-soluble compounds, no significant change of concentration was found [25].
This study has potential limitations such as the small number of patients enrolled in the study group compared to a larger number of patients in the control group, the lack of a prospective and blinded design and the fact that some of the patients used polysulphone dialyzers when treated with HDF and polyamide dialyzers when treated with HD.
In conclusion, nutrition, assessed by albumin, nPCR and BMI, was not improved by HDF compared to HD. Also, anemia management was not superior, since for similar hemoglobin levels, higher doses of EPO were needed with HDF. Dialysis efficiency expressed by Kt/V and phosphate levels were significantly improved after 12 months HDF, but exactly the same pattern was seen in patients treated only with HD. It is thus impossible to conclude that the switch to HDF made any significant difference to these parameters. We are aware that larger prospective randomized trials are needed before drawing a final conclusion concerning the potential benefits of HDF treatment compared to HD.
References
Schiffl H (2007) Prospective randomized cross-over long-term comparison of online haemodiafiltration and ultrapure high-flux haemodialysis. Eur J Med Res 12(1):26–33
Vilar E, Fry AC, Wellsted D, Tattersall JE, Greenwood RN, Farrington K (2009) Long-term outcomes in online hemodiafiltration and high-flux hemodialysis: a comparative analysis. Clin J Am Soc Nephrol 4(12):1944–1953
Henderson LW, Beans E (1978) Successful production of sterile pyrogen-free electrolyte solution by ultrafiltration. Kidney Int 14:522–525
Grooteman MP, van den Dorpel MA, Bots ML, Penne EL, van der Weerd NC, Mazairac AH, den Hoedt CH, van der Tweel I, Lévesque R, Nubé MJ, Ter Wee PM, Blankestijn PJ, for the CONTRAST Investigators (2012) Effect of online hemodiafiltration on all-cause mortality and cardiovascular outcomes. J Am Soc Nephrol 23(6):1087–1096
Comparison of Post-dilution On-line Hemodiafiltration and Hemodialysis (Turkish HDF study). Available at http://clinicaltrials.gov/ct2/show/NCT00411177. Accessed July 2012
Schmid H, Schiffl H (2012) Hemodiafiltration and survival of end-stage renal disease patients: the long journey goes on. Int Urol Nephrol. doi:10.1007/s11255-012-0232-y
Locatelli F, Altieri P, Andrulli S, Bolasco P, Sau G, Pedrini LA, Basile C, David S, Feriani M, Montagna G, Di Iorio BR, Memoli B, Cravero R, Battaglia G, Zoccali C (2010) Hemofiltration and hemodiafiltration reduce intradialytic hypotension in ESRD. J Am Soc Nephrol 21(10):1798–1807
Penne EL, van der Weerd NC, van den Dorpel MA, Grooteman MP, Lévesque R, Nubé MJ, Bots ML, Blankestijn PJ, ter Wee PM, CONTRAST Investigators (2010) Short-term effects of online hemodiafiltration on phosphate control: a result from the randomized controlled Convective Transport Study (CONTRAST). Am J Kidney Dis 55(1):77–87
Bonforte G, Grillo P, Zerbi S, Surian M (2002) Improvement of anemia in hemodialysis patients treated by hemodiafiltration with high-volume on-line-prepared substitution fluid. Blood Purif 20(4):357–363
Pinney JH, Oates T, Davenport A (2011) Haemodiafiltration does not reduce the frequency of intradialytic hypotensive episodes when compared to cooled high-flux haemodialysis. Nephron Clin Pract 119(2):c138–c144
Oates T, Pinney JH, Davenport A (2011) Haemodiafiltration versus high-flux haemodialysis: effects on phosphate control and erythropoietin response. Am J Nephrol 33(1):70–75
Stefánsson BV, Abramson M, Nilsson U, Haraldsson B (2012) Hemodiafiltration improves plasma 25-hepcidin levels: a prospective, randomized, blinded, cross-over study comparing hemodialysis and hemodiafiltration. Nephron Extra 2(1):55–65
Tomo T, Matsuyama K, Nasu M (2004) Effect of hemodiafiltration against radical stress in the course of blood purification. Blood Purif 22(suppl 2):72–77
Combarnous F, Tetta C, Cellier CC, Wratten ML, Custaud MA, De Catheu T, Fouque D, David S, Carraro G, Laville M (2002) Albumin loss in on-line hemodiafiltration. Int J Artif Organs 25(3):203–209
Cross J, Davenport A (2011) Does online hemodiafiltration lead to reduction in trace elements and vitamins? Hemodial Int 15(4):509–514
Altieri P, Sorba G, Bolasco P, Ledebo I, Ganadu M, Ferrara R, Menneas A, Asproni E, Casu D, Passaghe M, Sau G, Cadinu F, Sardinian Study Group on Hemofiltration On-line (2004) Comparison between hemofiltration and hemodiafiltration in a long-term prospective cross-over study. J Nephrol 17(3):414–422
Ward RA, Schmidt B, Hullin J, Hillebrand GF, Samtleben W (2000) A comparison of on-line hemodiafiltration and high-flux hemodialysis: a prospective clinical study. J Am Soc Nephrol 11(12):2344–2350
Vaslaki L, Major L, Berta K, Karatson A, Misz M, Pethoe F, Ladanyi E, Fodor B, Stein G, Pischetsrieder M, Zima T, Wojke R, Gauly A, Passlick-Deetjen J (2006) On-line haemodiafiltration versus haemodialysis: stable haematocrit with less erythropoietin and improvement of other relevant blood parameters. Blood Purif 24(2):163–173
Zehnder C, Gutzwiller JP, Renggli K (1999) Hemodiafiltration—a new treatment option for hyperphosphatemia in hemodialysis patients. Clin Nephrol 52(3):152–159
Pérez-García R, Albalate M, de Sequera P, Alcázar R, Puerta M, Ortega M, Corchete E (2012) On-line haemodiafiltration improves response to calcifediol treatment. Nefrologia. doi:10.3265/Nefrologia.pre2012.Jan.11189
Movilli E, Camerini C, Gaggia P, Poiatti P, Pola A, Viola BF, Zubani R, Jeannin G, Cancarini G (2011) Effect of post-dilutional on-line haemodiafiltration on serum calcium, phosphate and parathyroid hormone concentrations in uraemic patients. Nephrol Dial Transpl 26(12):4032–4037
Vaslaki L, Major L, Berta K, Karatson A, Misz M, Pethoe F, Ladanyi E, Fodor B, Stein G, Pischetsrieder M, Zima T, Wojke R, Gauly A, Passlick-Deetjen J (2006) On-line haemodiafiltration versus haemodialysis: stable haematocrit with less erythropoietin and improvement of other relevant blood parameters. Blood Purif 24:163–173
Lin CL, Huang CC, Yu CC, Wu CH, Chang CT, Hsu HH, Hsu PY, Yang CW (2002) Improved iron utilization and reduced erythropoietin resistance by on-line hemodiafiltration. Blood Purif 20:349–356
Pedrini LA, De Cristofaro V, Comelli M, Casino FG, Prencipe M, Baroni A, Campolo G, Manzoni C, Colì L, Ruggiero P, Acquistapace I, Auriemma L (2011) Long-term effects of high-efficiency on-line haemodiafiltration on uraemic toxicity. A multicentre prospective randomized study. Nephrol Dial Transpl 26(8):2617–2624
Meert N, Waterloos MA, Van Landschoot M, Dhondt A, Ledebo I, Glorieux G, Goeman J, Van der Eycken J, Vanholder R (2010) Prospective evaluation of the change of predialysis protein-bound uremic solute concentration with postdilution online hemodiafiltration. Artif Organs 34(7):580–585
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orasan, R.A., Patiu, I.M., Anghel, D. et al. Variation of clinical and laboratory features in chronic dialysis patients treated with high-flux hemodialysis after switching to online hemodiafiltration. Int Urol Nephrol 45, 1415–1422 (2013). https://doi.org/10.1007/s11255-012-0341-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-012-0341-7