Abstract
Objective
Associations between 25 hydroxy vitamin D [25(OH)D], adipokines levels, and insulin resistance have been reported. The aim of this study was to explore the effects of cholecalciferol supplementation on vitamin D levels, insulin resistance, leptin, and adiponectin levels in vitamin D-deficient peritoneal dialysis (PD) patients.
Methods
In nineteen vitamin D-deficient PD patients, who were treated with cholecalciferol, fasting serum glucose, insulin, adiponectin, leptin, 25(OH)D and parathyroid hormone (PTH) were measured before and after cholecalciferol replacement therapy. Eighteen (94.7 %) PD patients with vitamin D deficiency were receiving active vitamin D compounds (alphacalciferol) for PTH control. Alphacalciferol dosing was kept constant during treatment with cholecalciferol.
Results
While mean 25(OH)D significantly increased from (10.2 ± 4.9 ng/ml) to (82.9 ± 56.5 ng/ml) (p < 0.05), mean homeostatic model assessment-insulin resistance index significantly decreased from (4.6 ± 3.6) to (2.8 ± 2.0) after cholecalciferol replacement therapy (p < 0.05). Serum leptin levels (12.9 ± 17.6 ng/ml) significantly increased (18.1 ± 19.5 ng/ml) (p < 0.05), while there was no change in serum adiponectin, calcium, and phosphate after vitamin D replacement. Serum PTH levels significantly decreased from 551.9 ± 276.6 pg/ml to 434.0 ± 273.4 ng/ml.
Conclusions
Cholecalciferol replacement therapy significantly decreases PTH levels and insulin resistance. The results of this study need to be confirmed in larger clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adipocytes produce and secrete several proteins that act as veritable hormones, collectively called adipokines such as leptin and adiponectin, that play a central role in whole-body homeostasis by influencing a variety of biological and physiological processes, including food intake, insulin action, lipid, and glucose metabolism, regulation of energy balance, coagulation, angiogenesis, and vascular remodeling. Alteration in adipokines levels has been implicated in the pathogenesis of insulin resistance, dyslipidemia, and atherosclerosis [1–6].
Glucose intolerance, alteration in adipokines levels, hyperinsulinemia, and insulin resistance are the common findings in patients on dialysis. Several factors such as uremic toxins, exercise tolerance, metabolic acidosis and secondary hyperparathyroidism implicated in the pathogenesis of these disturbances in dialysis patients [7–10].
The relationship among serum 25(OH)D, adipokines, and insulin resistance was reported in patients with normal kidney functions [11–14]. Vitamin D deficiency is very common in patients on chronic dialysis [15–18].
The aim of this study was to investigate the effect of vitamin D replacement with cholecalciferol in peritoneal dialysis patients with vitamin D deficiency on serum leptin, adiponectin levels, and insulin resistance.
Materials and methods
We conducted a prospective clinical pilot study in vitamin D-deficient PD patients to explore the effects of cholecalciferol replacement on vitamin D levels, PTH, insulin resistance, serum adiponectin, and leptin.
Nineteen PD patients (11 men, 8 women) on dialysis for longer than 3 months were studied. In all patients, 25(OH)D level was less than 20 ng/ml (<50 nmol/l). This study was approved by the institutional ethical committee.
Diabetic, clinically unstable patients, those with tumors or inflammatory diseases (such as chronic pulmonary disease, and malnutrition), and those treated with immunosuppressives were excluded. No patient showed signs of inflammation or infection during the study period. No participant had morbid obesity (BMI > 40 kg/m2), infections, or any other serious medical problems.
In our clinic, we prescribe cholecalciferol to all CKD patients whose 25(OH) D levels are less than 30 ng/ml (75 nmol/l). In this study, all patients were prescribed colecalciferol as a rutin protocol, 50 000 IU orally once per week for 4–8 weeks. Calcitriol or alphacalciferol dosing (if patients were on either of these drugs) was held constant during treatment with cholecalciferol. The levels of 25(OH) were rechecked and, if still deficient, the patient was given another course of cholecalciferol. Serum samples were taken monthly for calcium and phosphorus and quarterly for PTH for 3 months.
Patients were seen in the PD clinic every 4 weeks. At the beginning of the study, serum levels of corrected total calcium, phosphorus, albumin, total protein, iPTH, and 25(OH)D were measured. The usage of active vitamin D (1 alpha calcidiol and calcitriol) was documented.
Body mass index (BMI) was calculated by dividing the dry weight in kilograms by the square of the height in meters. Total adipose tissue mass (TATM) was assessed by means of bioelectrical impedance analysis using a commercially available bioimpedance analyzer (Body Composition analyzer Type TBF-300 m).
Fasting samples of venous blood were obtained from an antecubital vein between 08:30 and 09:00 h in all subjects for the estimation of hormonal and general analytical data. Blood samples were centrifuged immediately, and the serum samples were stored at −20 °C until analysis of the data.
25(OH) D levels were measured by radioimmunometric assay (Recipe Chemical Instrument GmbH, Munich Germany). Serum adiponectin levels were determined using enzyme-linked immunosorbent assay kits (Linco Research, St. Charles, MI, USA). Serum leptin was measured using enzyme-linked immunosorbent assay kit (DRG instruments GmbH, Marburg, Germany). The insulin levels were determined by chemiluminescent-based Immulite 2000 system (DPC, Los Angeles, CA, USA). Calcium, phosphate, alkaline phosphatase, albumin, creatinine, glucose, cholesterol, and triglycerides were measured using standard laboratory techniques.
Assessment of insulin resistance using homeostatic model assessment-insulin resistance (HOMA-IR)
Insulin resistance was assessed using the HOMA-IR originally described by Matthews et al. [19].
HOMA-IR was calculated using the following formula:
Bioelectrical impedance analysis
Lean body mass and total percentage body fat were determined using a bioelectrical impedance analyzer (RJL Systems, Clinton Township, MI, USA).
Statistical analyses
Data are presented as mean ± SD. The paired t test or Wilcoxon signed-rank test was used when baseline data were compared with those obtained during follow-up. Correlation between 25(OH)D3 and PTH, BMD, cholesterol, adiponectin, and leptin levels was tested using Pearson and Spearman correlations where appropriate. A two-tailed p value of 0.05 was considered significant. All statistical analyses were performed with SPSS version 14.0 (SPSS Software, Chicago, IL, USA).
Results
Causes of renal failure in PD patients included chronic glomerulonephritis (n = 6), hypertensive nephrosclerosis (n = 5), and unknown (n = 8). The mean age was 47.2 ± 13.1 years. BMI, fat mass, fat percentage were 26.2 ± 7.6 kg/m2, 15.7 ± 11.6 kg, and 21.1 ± 11.5, respectively.
All patients were on continuous ambulatory peritoneal dialysis (CAPD). According to the peritoneal equilibration test (PET) performed in the last 6 months, mean ratio of solute concentrations in dialysate and plasma (D/P ratio) for urea at 4 h’dwell time was 0.75 ± 0.10. The mean of urea and creatinine clearance was 3.8 ± 4.2 ml/min. The mean KT/V urea was 2.0 ± 0.3. Ten patients were using 2 L 1.36 % dextrose solutions (13.6 mg/ml glucose) 3 times and once 2 L icodextrin daily. Five patients were on 2 times 2 L 1.36 % dextrose solutions (13.6 mg/ml glucose) and once 2 L 2.27 % dextrose solutions (22.7 mg/ml Glucose) and once 2 L icodextrin daily. Two patients were on four daily CAPD exchanges with 2 L 1.36 % dextrose solutions (13.6 mg/ml glucose). Two patients were using three times 2 L 2.27 % dextrose solutions (22.7 mg/ml glucose) and once 2 L icodextrin daily.
Eighteen (94.7 %) of the patients were taking 1 α (OH)D therapy (p < 0.05). The mean dose of 1 α (OH)D was 0.54 ± 0.27 μg. No patients were taking any multivitamin tablets.
While mean 25(OH)D significantly increased from (10.2 ± 4.6 ng/ml) to (82.9 ± 56.5 ng/ml) (p < 0.05), mean HOMA-IR index significantly decreased from (4.6 ± 3.6) to (2.7 ± 1.9) after vitamin D replacement (p < 0.05). Serum leptin levels (12.9 ± 17.6 ng/ml) significantly increased (18.1 ± 19.5 ng/ml) (p < 0.05) while there was no change in serum adiponectin, calcium, and phosphore. Serum PTH levels significantly decreased from (551.6 ± 276.6 pg/ml) to (434.0 ± 273.4 ng/ml) (Table 1).
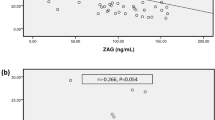
After vitamin D replacement, HOMA-IR index was positively correlated with serum leptin levels (r = 0.510; p = 0.036). No significant correlation between 25(OH)D and PTH, age, serum albumin, and duration of dialysis was found in PD patients (Table 2).
Discussion
We have regularly prescribed cholecalciferol for dialysis patients with vitamin D deficiency in our unit. Cholecalciferol replacement led to normalization of 25(OH)D levels, and a decrease in PTH, and HOMA-IR index in our study.
Eighteen (94.7 %) of PD patients with vitamin D deficiency were receiving active vitamin D compounds (alphacalciferol) for PTH control (p > 0.05). Alphacalciferol dosing was held constant during replacement with cholecalciferol.
In our another study, we found that PD patients with hypovitaminosis D are at higher risk of insulin resistance even they are on active vitamin D treatment for PTH control. In that study, we found a negative correlation between serum 25(OH)D levels and insulin resistance in PD patients and in multiple regression analyses, the independent predictors of HOMA-IR index were 25(OH)D levels, duration of dialysis and percentage of fat in PD patients [20].
Several studies in patients with normal renal function reported that vitamin D, or its active metabolite 1,25-dihydroxyvitamin D (1,25(OH)2D), improves insulin sensitivity, even in patients with glucose metabolism parameters within normal ranges. As the mechanisms which may lead to this effect potential relationships with improvements in insulin resistance, altered insulin receptor expression and specific effects on insulin action were implicated. It was reported that these actions may be mediated by systemic or local production of 1,25(OH)2D or by suppression of parathyroid hormone. The studies performed in patients with normal renal function have shown that insulin sensitivity is improved by as much as 60 % when levels of vitamin D are increased from 25 to 75 nmol/l, and this is better than troglitazone (54 %) or metformin (13 %) [21–23].
Kautzky-Willer et al. [24] investigated the effect of a 12-week intravenous treatment with 1,25(OH)2D, on glucose metabolism in 10 hemodialysis patients compared with 10 healthy control subjects by the frequently sampled intravenous glucose tolerance test, analyzed with the minimal model technique. These authors reported that intravenous vitamin D treatment led to a significant reduction of parathyroid hormone levels and to a complete normalization of insulin sensitivity in the hemodialysis patients and that intravenous 1,25(OH)2D improves insulin resistance in uremic patients, acting per se or by reducing secondary hyperparathyroidism.
Gunal et al. [25] examined the effect of a four-week intravenous treatment with 1 alpha-hydroxyvitamin D3 on insulin sensitivity in 14 patients on chronic hemodialysis. The following treatment with 1 alpha-hydroxyvitamin D3, levels of parathyroid hormone, the insulin concentrations decreased and C-peptide concentrations increased. These authors reported that intravenous 1 alpha-hydroxyvitamin D3 treatment has improved insulin sensitivity directly or by reducing secondary hyperparathyroidism in uremic patients on chronic hemodialysis.
Bonakdaran et al. [26] assessed the effect of oral calcitriol on glucose metabolism in 27 patients on hemodialysis. In patients who received oral calcitriol for eight weeks, in blood sugar after 75 grams of glucose, HOMA-IR, total cholesterol and triglycerides, there was a significant decrease after the study period. These authors reported that vitamin D has a significant influence on glucose metabolism.
The studies have shown that increased PTH concentrations were associated with impaired glucose tolerance and decreased insulin sensitivity. Treatment with vitamin D decreases serum PTH levels [11–13]. In our study, we detected a decrease in PTH levels after replacement. Vitamin D may stimulate the expression of insulin receptor and thereby enhance insulin responsiveness for glucose transport [27, 28]. Vitamin D deficiency might induce a higher inflammatory response, which is associated with insulin resistance [29–31]. Vitamin D replacement may control all these factors. We found a significant decrease in insulin resistance after vitamin D replacement even the patients had already been on active vitamin D.
Adiponectin is a multifunctional protein with protective roles against the development of insulin resistance, dyslipidemia, nonalcoholic fatty liver disease, atherosclerosis, cardiac hypertrophy, and ischemic injury. Obesity is associated with decreased adiponectin levels [1–3].
Gannagé-Yared et al. [32] reported that higher 25(OH)D levels associated with higher adiponectin levels, in a small population of young and lean subjects with vitamin D sufficiency. Nimitphong et al. [33] showed a positive relation between 25(OH)D and adiponectin.
Vaidya et al. [34] reported in a cross-sectional analyses performed on 1,206 women from the Nurses’ Health Study I (NHS) and 439 men from the Health Professionals Follow-Up Study that higher 25(OH)D concentrations were independently associated with higher adiponectin concentrations in large populations of women and men. Lorente-Cebrián et al. [11] reported that 1,25(OH)2D attenuates adiponectin production in human adipocytes, thereby reducing the expression of both pro- and anti-inflammatory factors. Menendez et al. [12] showed that vitamin D3 presents a direct inhibitory effect on leptin secretion from human adipose tissue culture. Vitamin D receptor has been identified in preadipocytes [35, 36], and it is possible that 1,25(OH)2D, the active form of this vitamin, may regulate the adiponectin gene expression. As a hormone, vitamin D is thought to play a role in regulating the production of tumor necrosis factor-a [35], which is one of the proposed factors affecting the synthesis of adiponectin [36]. However, we could not find any change in serum adiponectin levels after vitamin D replacement while serum leptin levels increased significantly.
Our study has several limitations. The small sample size limits the power of our study. It is not a placebo controlled drug study. We prescribe cholecalcipherol to all patients with vitamin D deficiency as a routine approach. This study examined effect of this routine approach on insulin resistance, serum leptin, and adipoleptin levels in PD patients. Vitamin D studies in patients on dialysis have predominantly used active vitamin D compounds and focused on 1,25(OH)2D deficiency. However, to our knowledge, this is the first study to examine the effect of vitamin D replacement with cholecalcipherol on serum leptin, adiponectin, and insulin resistance in dialysis patients.
As a conclusion, our results show that insulin resistance decreased after vitamin D replacement in PD patients with vitamin D deficiency even the patients had been on active vitamin D. However, leptin levels increased while adiponectin levels did not change after vitamin D replacement. Prospective larger clinical trials are needed to more clearly define these relations.
References
Shimada K, Miyazaki T, Daida H (2004) Adiponectin and atherosclerotic disease. Clin Chim Acta 344:1–12
Cnop M, Havel PJ, Utzschneider KM et al (2003) Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex. Diabetologia 46:459–469
Tschritter O, Fritsche A, Thamer C et al (2003) Plasma adiponectin concentrations predict insulin sensitivity of both glucose and lipid metabolism. Diabetes 52:239–243
Chen C, Chang YC, Liu CL, Liu TP, Chang KJ et al (2007) Leptin induces proliferation and anti-apoptosis in human hepatocarcinoma cells by up- regulating cyclin D1 and down-regulating Bax via a Janus kinase 2-linked pathway. Endocr Relat Cancer 14:513–529
Hoda MR, Keely SJ, Bertelsen LS, Junger WG, Dharmasena D et al (2007) Leptin acts as a mitogenic and antiapoptotic factor for colonic cancer cells. Brit J Surg 94:346–354
Ahima RS, Saper CB, Flier JS, Elmquist JK (2000) Leptin regulation of neuroendocrine systems. Front Neuroendocrinol 21:263–307
Rodríguez-Carmona Ana, Fontán MiguelPérez, Cordido Fernando, Falcón TeresaGarcía, García-Buela Jesús (2000) Hyperleptinemia is not correlated with markers of protein malnutrition in chronic renal failure. Nephron 86:274–280
Huang JW, Yen CJ, Chiang HW, Hung KY, Tsai TJ, Wu KD (2004) Adiponectin in peritoneal dialysis patients: a comparison with hemodialysis patients and subjects with normal renal function. Am J Kidney Dis 43:1047–1055
Taskapan MC, Taskapan H, Sahin I, Keskin L, Atmaca H, Ozyalin F (2007) Serum leptin, resistin, and lipid levels in patients with end stage renal failure with regard to dialysis modality. Ren Fail 29(2):147–154
Taskapan MC, Taskapan H, Sahin I, Keskin L, Atmaca H, Ozyalin F (2007) Relationship between insulin resistance and malondialdehyde levels in dialysis patients. Ren Fail 29(5):649–651
Lorente-Cebrián S, Eriksson A, Dunlop T, Mejhert N, Dahlman I, Aström G, Sjölin E, Wåhlén K, Carlberg C, Laurencikiene J, Hedén P, Arner P, Rydén M (2012) Differential effects of 1a,25-dihydroxycholecalciferol on MCP-1 and adiponectin production in human white adipocytes. Eur J Nutr 51(3):335–342
Menendez C, Lage M, Peino R, Baldelli R, Concheiro P et al (2001) Retinoic acid and vitamin D(3) powerfully inhibit in vitro leptin secretion by human adipose tissue. J Endocrinol 170:425–431
Reis JP, von Muhlen D, Kritz-Silverstein D, Wingard DL, Barrett-Connor E (2007) Vitamin D, parathyroid hormone levels, and the prevalence of metabolic syndrome in community-dwelling older adults. Diabetes Care 30:1549–1555
Vaidya A, Forman JP, Underwood PC et al (2011) The influence of body-mass index and renin-angiotensin-aldosterone system activity on the relationship between 25-hydroxyvitamin D and adiponectin in Caucasian men. Eur J Endocrinol 164:995–1002
Taskapan H, Ersoy FF, Passadakis P, Tam P, Memmos D, Katopodis K, Ozener C, Akcicek F, Camsarı T, Ates K, Ataman R, Vlachojannis JG, Dombros N, Utas C, Akpolat T, Bozfakioglu S, Wu GG, Karayaylali I, Arınsoy T, Stathakis Ch, Yavuz M, Tsakiris D, Dimitriades A, Yılmaz ME, Gultekin M, Karayalçin B, Polat N, Oreopoulos DG (2006) Severe vitamin D deficiency in chronic renal failure patients on peritoneal dialysis. Clin Nephrol Clin Nephrol 66(4):247–255
Taskapan H, Wei M, Oreopoulos DG (2006) 25(OH) Vitamin D(3) in patients with chronic kidney disease and those on dialysis: rediscovering its importance. Int Urol Nephrol 38(2):323–329
Taskapan H, Ersoy FF, Passadakis P, Tam P, Memmos D, Katopodis K, Ozener C, Akcicek F, Camsarı T, Ates K, Ataman R, Vlachojannis JG, Dombros N, Utas C, Akpolat T, Bozfakioglu S, Wu GG, Karayaylalı I, Arınsoy T, Stathakis Ch, Yavuz M, Tsakiris D, Dimitriades A, Yılmaz ME, Gultekin M, Karayalçin B, Polat N, Oreopoulos DG (2005) Body pain during daily activities in patients on peritoneal dialysis. Dial Transplant 2:58–72
Taskapan H (2012) Is 24,25(OH)D level really high in dialysis patients with high FGF23 levels? Int Urol Nephrol (Epub ahead of print)
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and B-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Bindal ME, Taskapan H (2011) Hypovitaminosis D and insulin resistance in peritoneal dialysis patients. Int Urol Nephrol 43(2):527–534
Chiu KC, Chu A, Go VL, Saad MF (2004) Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr 79(5):820–825
Norman AW, Frankel JB, Heldt AM, Grodsky GM (1980) Vitamin D deficiency inhibits pancreatic secretion of insulin. Science 209(4458):823–825
Inzucchi SE, Maggs DG, Spollett GR, Page SL, Rife FS, Walton V et al (1998) Efficacy and metabolic effects of metformin and troglitazone in type II diabetes mellitus. N Engl J Med 338(13):867–872
Kautzky-Willer A, Pacini G, Barnas U, Ludvik B, Streli C, Graf H, Prager R (1995) Intravenous calcitriol normalizes insulin sensitivity in uremic patients. Kidney Int 47(1):200–206
Gunal AI, Celiker H, Celebi H, Ustundağ B, Gunal SY (1997) Intravenous alfacalcidol improves insulin resistance in hemodialysis patients. Clin Nephrol 48(2):109–113
Bonakdaran S, Ayatollahi H, Mojahedi MJ, Sharifipoor F, Shakeri M (2008) Impact of treatment with oral calcitriol on glucose intolerance and dyslipidemia(s) in hemodialysis patients. Saudi J Kidney Dis Transpl 19(6):942–947
Maestro B, Davila N, Carranza MC, Calle C (2003) Identification of a Vitamin D response element in the human insulin receptor gene promoter. J Steroid Biochem Mol Biol 84:223–230
Maestro B, Campion J, Davila N, Calle C (2000) Stimulation by 1,25- dihydroxyvitamin D3 of insulin receptor expression and insulin responsiveness for glucose transport in U-937 human promonocytic cells. Endocr J 47:383–391
Cohen-Lahav M, Douvdevani A, Chaimovitz C, Shany S (2007) The anti-inflammatory activity of 1,25-dihydroxyvitamin D3 in macrophages. J Steroid Biochem Mol Biol 103:558–562
Cantorna MT, Mahon BD (2005) D-hormone and the immune system. J Rheumatol Suppl 76:11–20
Shoelson SE, Herrero L, Naaz A (2007) Obesity, inflammation, and insulin resistance. Gastroenterology 132:2169–2180
Gannagé-Yared MH, Chedid R, Khalife S et al (2009) Vitamin D in relation to metabolic risk factors, insulin sensitivity and adiponectin in a young middle-eastern population. Eur J Endocrinol 160:965–971
Nimitphong H, Chanprasertyothin S, Jongjaroenprasert W, Ongphiphadhanakul B (2009) The association between vitamin D status and circulating adiponectin independent of adiposity in subjects with abnormal glucose tolerance. Endocrine 36:205–210
Vaidya A, Williams JS, Forman JP (2012) The independent association between 25-hydroxyvitamin D and adiponectin and its relation with BMI in two large cohorts: the NHS and the HPFS. Obesity (Silver Spring) 20(1):186
Lee S, Lee DK, Choi E, Lee JW (2005) Identification of a functional vitamin D response element in the murine Insig-2 promoter and its potential role in the differentiation of 3T3–L1 preadipocytes. Mol Endocrinol 19:399–408
Kamei Y, Kawada T, Kazuki R, Ono T, Kato S, Sugimoto E (1993) Vitamin D receptor gene expression is up-regulated by 1, 25-dihydroxyvitamin D3 in 3T3–L1 preadipocytes. Biochem Biophys Res Commun 193:948–955
Acknowledgments
This study was supported by Inonu University Medical Research Center.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ulutas, O., Taskapan, H., Taskapan, M.C. et al. Vitamin D deficiency, insulin resistance, serum adipokine, and leptin levels in peritoneal dialysis patients. Int Urol Nephrol 45, 879–884 (2013). https://doi.org/10.1007/s11255-012-0308-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-012-0308-8