Abstract
Background
To present a comprehensive experience of botulinum toxin A (BTX-A) injected into the detrusor muscle in patients with spinal cord injuries (SCI) causing neurogenic detrusor overactivity.
Methods
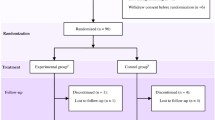
Three hundred units of BTX-A were injected cystoscopically into the detrusor muscle of 108 patients with neurogenic detrusor overactivity secondary to SCI at 30 different locations. Evaluations were performed before the injections and 6 weeks after, and they included determination of bladder urinary continence status, frequency/volume chart of CIC, concomitant anticholinergic medication use, Incontinence Quality of Life questionnaire (I-QOL) and patient satisfaction. Key urodynamic parameters (reflex volume, maximum detrusor pressure during voiding, detrusor compliance and maximum cystometric capacity) were analyzed at the outset and during the follow-up (6, 12 and 36 weeks) examinations.
Results
By the time of the urodynamic follow-up examinations (6, 12 and 36 weeks), the mean cystometric capacity (P < 0.05) and the mean reflex volume (P < 0.05) increased significantly, while the mean voiding pressure (P < 0.05) decreased significantly. No complications or side effects were reported. Most patients considerably reduced or even stopped taking anticholinergic drugs and were satisfied with the treatment.
Conclusions
This retrospective study indicates that BTX-A injections into the detrusor muscle to treat neurogenic detrusor overactivity secondary to SCI are safe and valuable. Significant improvement of bladder function corresponded with continence and subjective satisfaction indicated by the treated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord injury (SCI) results from a variety of traumatic and non-traumatic events with an annual incidence of up to 40 cases per million people [1]. Prevention of upper urinary tract damage and renal failure is the ultimate goal of any urological treatment, but urinary incontinence in a young paraplegic with suprasacral SCI associated with neurogenic detrusor overactivity (NDO) can greatly reduce quality of life.
Currently, clean intermittent catheterization (CIC) combined with anticholinergic medication is the “gold standard” treatment for NDO. In fact, 90% of patients with neurogenic bladder dysfunction can be treated effectively with anticholinergic medication and CIC [2]. However, detrusor overactivity recurs immediately after withdrawal of medication, even after long-term treatment with anticholinergic medication. This implies that there are no long-lasting therapeutic effects of pharmacological treatments. Thus, patients with NDO must be permanently treated with anticholinergic medications and face lifelong side effects unless an alternative treatment is found.
A relatively new alternative treatment, injection of botulinum toxin A (BTX-A) into the detrusor muscle, was first reported by Schurch et al. [3] in adult patients with neurogenic bladder hyperreflexia due to SCI.
BTX-A is a neurotoxin produced by Clostridium botulinum, which causes botulism and is the most potent natural poison. The neurotoxin binds to the pre-synaptic nerve endings of cholinergic neurons and enters the neuron by receptor-mediated endocytosis. In the neuron, the catalytic domain specifically cleaves the SNAP-25 protein, which is essential for normal synaptic vesicle fusion. This cleavage results in the inhibition of neuronal acetylcholine secretion, which ultimately leads to a temporary chemodenervation and the loss or reduction of neuronal activity at the target organs [4]. In general, this chemodenervation is fully reversible [5]. Recently, injection of BTX-A into the detrusor smooth muscle to treat detrusor overactivity and neurogenic incontinence has been proven to be effective [3, 6]. This minimally invasive procedure offers a new therapeutic option to patients who are resistant to or incompatible with anticholinergic drug therapy and surgical procedures such as enterocystoplasty. This study summarizes the experience of a center in China with injection of BTX-A(Lanzhou Institute of Biological Products, China) into the detrusor muscle to manage NDO in patients secondary to traumatic SCI. It has been concluded before that Chinese BTX-A and Allergan’s Botox have similar efficacy, safety, tolerability profiles and equivalence of doses for blepharospasm and hemifacial spasm treatments [7, 8].
Patients and methods
Between September 2002 and August 2009, we treated 108 patients (81 males and 27 females) with NDO secondary to traumatic SCI who experienced unacceptable side effects or were resistant to anticholinergic medication (Table 1). SCI was diagnosed according to ASIA standards [9]. The patients received BTX-A injections in conjunction with CIC to treat neurogenic lower and upper urinary tract dysfunction (detrusor overactivity, low compliance, reduced bladder capacity, incontinence and upper urinary dilation). Detrusor overactivity was diagnosed urodynamically. Incontinence was defined as any episode of urinary voiding between two CICs and was quantified with an absorbent pad.
All eligible patients gave informed consent before starting the treatment program. Before the BTX-A injections and 6 weeks after, patients were asked to keep a diary on incontinence, diuresis, CIC timing and the amount of anticholinergic medication during tapering. The urodynamic evaluation was performed at the outset and during the follow-up(6, 12 and 36 weeks) examinations, and variables were defined according to standards recommended by the International Continence Society(ICS) [10]. During the urodynamic assessments, special attention was given to the following key parameters: (1) the reflex volume (RV), which was defined as the infused volume at the start of the first reflex detrusor contraction during the filling phase, (2) the maximum detrusor pressure during voiding (MVP), (3) the bladder compliance, which was defined as the relationship between the change in bladder volume and the change in detrusor pressure (calculated by dividing the volume change by the change in detrusor pressure during the change in bladder volume) and (4) the maximum cystometric capacity (MCC), which was defined as the infused volume during involuntary voiding or the volume at the time that the investigator decided to stop filling (usually at 500 ml).
All patients were asked to complete the Incontinence Quality of Life Questionnaire (I-QOL) [11] before and 6 weeks after the injections. The questionnaire was a 22-item, domain-specific, validated, self-report test that detected changes in the self-perceived severity of incontinence. The QoL index was expressed as a score ranging from 0 (poor self-perceived QoL due to incontinence) to 100 (incontinence does not negatively affect QoL).
Patient satisfaction after BTX-A injection was rated on a scale from 1 to 10 (1 was defined as “not satisfied” and 10 was defined as “very satisfied”) [12].
BTX-A injections were performed with a normal 22 FF rigid cystoscope and a flexible injection needle. Three hundred units of BTX-A diluted in 15 ml saline were injected into the detrusor muscle at 30 different sites (10 units of the toxin in 0.5 ml saline per site). Care was taken to avoid the trigonum. Clinical and urodynamic data from the follow-up examinations were analyzed. The urodynamic parameters RV, MVP, detrusor compliance and MCC were measured at the follow-up assessment(6, 12 and 36 months) and compared to the baseline values. Patient satisfaction was also recorded.
Data are expressed as the mean (range). Paired t-tests (RV, MVP, and MCC) and chi-square tests (incontinence between CIC) were used for statistical comparisons considering P < 0.05 to indicate statistical significance.
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
A total of 108 patients with NDO secondary to traumatic SCI who experienced unacceptable side effects or were resistant to anticholinergic medication were treated with BTX-A injections. The patient characteristics are shown in Table 1.
Clinical and urodynamic data from the urodynamic examinations before and after detrusor BTX-A injections were analyzed. The data are shown in Table 2, Fig. 1.
Among the 80 patients who were incontinent before the BTX-A injections, 51 (63.75%) were continent at the follow-up examination 6 weeks after the injections. In 29 (36.25%) patients who were still incontinent after the BTX-A injections, 23 (28.75%) experienced a reduced degree of urinary incontinence and another 6 (7.5%) did not respond to BTX-A.
Before the BTX-A injections, 80 patients used anticholinergic medications (Table 1); daily doses ranged from 4–8 mg of tolterodine. After the BTX-A injections, 43 (53.75%) of these patients stopped taking anticholinergics. Another 28 (35%) patients reduced their daily requirements: 12 patients reduced their daily dose by 75%; 10 patients reduced their dose by 50%; 6 patients reduced their dose by 25% and 9 patients continued with the same dose levels (Fig. 2).
The urodynamic parameters were measured at the follow-up assessment(6, 12 and 36 months). MCC increased from 125.55 ± 49.09 ml to 313.09 ± 140.38 ml, 306.18 ± 132.32 ml and 140.00 ± 58.22 ml, respectively. MVP decreased from 53.27 ± 19.82 cm H2O to 39.36 ± 22.74 cm H2O, 40.00 ± 21.56 cm H2O, and 49.27 ± 17.97 cm H2O, respectively. RV increased from 57.91 ± 29.75 ml to 128.64 ± 77.22 ml, 126.09 ± 73.98 ml and 63.09 + 31.17 ml, respectively. The bladder compliance increased from 11.52 ± 7.80 ml/cm H2O to 16.74 ± 10.37 ml/cm H2O, 16.31 ± 10.38 ml/cm H2O and 12.13 ± 7.88 ml/cm H2O, respectively.
After treatment, the mean QoL index increased from 23.4 + 19.6 initially to 78.7 + 23.6 6 weeks after injection (P < 0.001). Most patients were either satisfied or very satisfied with their overall experience with BTX-A (Fig. 3). The mean patient satisfaction score was 6.4. No side effects of BTX-A were reported in our study.
In our study, 19 patients were treated with repeated BTX-A injections including 11 patients who received 2 injections, 6 patients who received 3 injections and 2 patients who received 5 injections. The results for the urodynamic outcome measurements after 6 weeks post-injections 1, 2 and 3 were given in Table 3. RV, MCC and MVP improved significantly after each BTX-A treatment compared to the baseline values.
Discussion
The physiologic alterations that accompany spinal cord injury (SCI), myelomeningocele (MMC) or multiple sclerosis (MS) can lead to significant bladder dysfunction. These disturbances are known to have a major impact on overall morbidity and quality of life. In the majority of SCI, MMC and MS patients, bladder dysfunction is categorized as upper motor neuron (UMN) dysfunction. UMN syndrome presents as a disruption of the descending pathways, which provide inhibitory input to the sacral micturition center. The loss of supraspinal control leads to involuntary, reflexive bladder contractions and frequently results in neurogenic incontinence. Additionally, in most cases, an impaired coordination of the detrusor and sphincter system (detrusor sphincter dyssynergia (DSD)) can result in elevated bladder pressure during micturition, which leads to structural bladder damage, vesicoureteral reflux and renal insufficiency. Management strategies for UMN syndrome should meet three main objectives: low-pressure urine storage, low-pressure voiding and adequate urine drainage. However, from the patient’s point of view, the most important goals are continence and good tolerability of the therapy [13].
The management of neurogenic bladder dysfunction has undergone many changes over the past 25 years. The gold standard for treating neurological bladder dysfunction has been anticholinergic medications, such as Tolterodine, and CIC. More than 90% of standard patients with SCI can be treated successfully with anticholinergic medications and CIC. However, in patients with severe hyperreflexia of the detrusor and/or DSD, anticholinergic medications are not sufficient. Furthermore, anticholinergic medications exhibit inherent dose-dependent side effects and, thus, might not be tolerated. The lack of efficacy, the presence of side effects and the poor compliance are the main reasons for considering alternative treatment options [1].
Previously, the only alternative in these cases was invasive surgery, such as sacral root stimulation or bladder augmentation. As an alternative to oral anticholinergic medication, the injection of BTX-A into the detrusor muscle has been suggested for patients who are incompatible with anticholinergic drug therapy prior to surgeries such as enterocystoplasty [13].
Intradetrusor injection of BTX-A was first described by Stohrer et al. [6] at the ICS meeting in 1999, followed by Schurch et al. [3] in 2000, who described a treatment option for patients who did not respond to or could not tolerate anticholinergic medications but were opposed to invasive surgical treatments such as enterocystoplasty. The report represented a milestone in the management of drug-resistant NDO. Recently, the largest study ever in this relatively new field was published by Reitz et al. In this report [13], the results of a multicenter study of 200 patients strongly supported the overwhelming benefits of BTX-A detrusor injections in neurogenic patients.
The first trials with BTX-A indicated promising results concerning the clinical and urodynamic benefits of this new treatment option. The neurotoxin injected into the bladder wall blocked the neuromuscular junction and relaxed the detrusor muscle for at least 36 weeks [3]. Highly efficient binding of the neurotoxin to the intramuscular nerve terminals may prevent passage into the circulatory system and any subsequent systemic side effects. The suburothelial injection of BTX not only had an effect on motor function, but it also affected the sensory function of the urinary bladder by restoring both the levels and the ratios of ATP and NO released from the urothelium [14].
This report presents the data of 108 patients treated with BTX-A and is the first study of its kind in China. In patients with NDO secondary to traumatic SCI, high bladder pressure frequently leads to structural bladder damage with restricted capacity and compliance. In these difficult cases, BTX-A was injected into the detrusor muscle. Injection of BTX-A was a simple and safe procedure without any complications or adverse effects. A dose titration study of the population studied in 2000 revealed that 300 units of BTX-A diluted in 30 ml of saline solution and injected at 30 locations within the detrusor muscle were sufficient to treat even severe NDO [3].
The trigonum was not injected, and no injections were made near the ureteric orifice in order to avoid damage to the upper urinary tract. It was determined by several major considerations. The submucosal nerve plexus, which is thought to be mainly sensory, is particularly prominent in the trigonum [15], and inserting a needle into this area risks impairing sensory nerve endings. Also, trigonal innervation is more complex than bladder dome innervation. The superficial and deep trigonum appears to be innervated by adrenergic, cholinergic and non-adrenergic non-cholinergic excitatory pathways [16]. Therefore, the effect of BTX-A, which selectively blocks the release of acetylcholine, would have been more difficult to analyze.
Forty-three of the 80 patients in the present study had previously used oral anticholinergics and they completely discontinued the medication after treatment with BTX-A. In the remaining 37 patients, 28 considerably reduced their intake of oral anticholinergics, which ended or alleviated systemic side effects related to the drugs. However, the reason that these patients needed to continue taking anticholinergic medications at all was unclear. From the urologist’s point of view, the objective improvement of bladder function as indicated by the urodynamic data supported the patients’ reports of partially or completely improved continence. For protection of bladder integrity and the upper urinary tract, low-pressure storage and low-pressure voiding were essential.
The relaxation of the detrusor muscle induced by BTX-A injections significantly increased reflex volume and bladder capacity after 6 weeks. This enabled patients to reduce the number of CIC within a 24-h period and improved patients’ quality of life. High voiding pressures, which may cause severe long-term complications, were significantly reduced to normal values after 6 weeks. Follow-up was 36 weeks, and the effect of BTX-A seemed to vanish gradually after that time. So this chemodenervation is fully reversible.
In the studied population, 6 out of 108 patients were identified as non-responders who experienced neither clinical nor urodynamic benefits. The reason that these patients did not respond was unclear; however, errors during toxin preparation and dilution could have contributed. Also, the ideal dose and dilution of BTX-A remain controversial. Some patients with severe restrictions in bladder compliance due to changes in the detrusor muscle or fibrosis did not respond to any conservative treatments (anticholinergic medication, intradetrusor injection with BTX-A, or neuromodulation). Another very important issue affecting efficacy is the injection technique [17]. Lately, we have preferred the suburothelial technique because it seems to be more effective and safer, and after comparing 2 recent studies, suburothelial injection seemed to be more effective than the intramuscular technique [18, 19]. The injection of BTX-A into the suburothelial space results in ballooning of the bladder mucosa at the injection site as a form of visual feedback.
The beneficial effects that were observed in the 102 responders were related to clinical as well as urodynamic parameters. From the patients’ point of view, continence and a good tolerability of the BTX-A treatment are essential because of their major impact on patient compliance and quality of life. Urodynamically, most patients achieved a state of low-pressure urine storage, low-pressure voiding and adequate urine drainage in combination with CIC.
The validity and responsiveness of the I-QOL questionnaire used in our study were previously confirmed in patients with neurogenic diseases [20]. The questionnaire was domain-specific for urinary incontinence, and the results indicated a dramatic improvement. Overall, most of the patients in the present study were satisfied with the BTX-A treatment with an average satisfaction score of 6.4. This value is comparable to previously published articles [12, 21]. Therefore, we are convinced that the injection of BTX-A into the detrusor muscle combined with CIC offers an adequate management option for patients with incontinence due to NDO secondary to traumatic SCI.
In this study, we also evaluated the efficacy and safety of BTX-A after repeated injections. Previous studies [22, 23] showed that repeated BTX-A injections were effective in patients with difficult-to-treat NDO. One potential problem with repeated administration of BTX-A is the formation of neutralizing antibodies (NAB) to the toxin, which diminish the treatment effects after repeated injections [24]. However, the lack of tachyphylaxis in our study and in the other published repeated dose studies [22, 23] suggests that NAB formation is not a serious problem. Risk factors for the formation of NAB are a high BTX-A dose and short injection intervals [25]. For the detrusor, relatively long injection intervals are important in reducing the risk of NAB formation.
There were limitations to this study. Only a few of the patients received repeated BTX-A injections, so we were unable to observe the effects of repeated injections on a large scale.
Conclusion
This retrospective study summarizes our experiences with injection of BTX-A into the detrusor muscle to treat neurogenic incontinence due to detrusor overactivity secondary to SCI and confirms that this new approach is a safe and valuable therapy without side effects. Significant improved bladder function corresponded with continence and subjective satisfaction as indicated by the treated patients.
References
Sekhon LH, Fehlings MG (2001) Epidemiology,demographics, and pathophysiology of acute spinal cord injury. Spine 26(24 Suppl):S2–S12
Riccabona M, Koen M, Schindler M et al (2004) Botulinum-A toxin injection into the detrusor: a safe alternative in the treatment of children with myelomeningocele with detrusor hyperreflexia. J Urol 171:845–848
Schurch B, Stohrer M, Kramer G et al (2000) Botulinum-A toxin for treating detrusor hyperreflexia in spinal cord injured patients: a new alternative to anticholinergic drugs? Preliminary results. J Urol 164:692–697
Lacy DB, Tepp W, Cohen AC et al (1998) Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat Struct Biol 5:898–902
de Paiva A, Meunier FA, Molgo J et al (1999) Functional repair of motor endplates after botulinum neurotoxin type A poisoning: biphasic switch of synaptic activity between nerve sprouts and their parent terminals. Proc Natl Acad Sci USA 96:3200–3205
Stohrer M, Schurch B, Kramer G et al (1999) Botulinum A toxin in the treatment of detrusor hyperreflexia in spinal cord injury. A new alternative to medical and surgical procedures? Neurourol Urodyn 18:401–402
Rieder CR, Schestatsky P, Socal MP et al (2007) A double-blind, randomized, crossover study of prosigne versus botox in patients with blepharospasm and hemifacial spasm. Clin Neuropharmacol 30:39–42
Quagliato EM, Carelli EF, Viana MA (2010) Prospective, randomized, double-blind study, comparing botulinum toxins type A botox and prosigne for blepharospasm and hemifacial spasm treatment. Clin Neuropharmacol 33:27–31
Maynard FM Jr, Bracken MB, Creasey G et al (1997) International standards for neurological and functional classification of spinal cord injury. American spinal injury association. Spinal Cord 35:266–274
Blaivas JG, Awad SA, Bissada N et al (2005) Urodynamic procedures: recommendations of the urodynamic society I. Procedures that should be available for routine urologic practice. Neurourol Urodyn 1:51–55
Schurch B, Denys P, Kozma CM et al (2007) Botulinum toxin A improves the quality of life of patients with neurogenic urinary incontinence. Eur Urol 52:850–858
Schulte-Baukloh H, Weiss C, Stolze T et al (2005) Botulinum-A toxin detrusor and sphincter injection in treatment of overactive bladder syndrome: objective outcome and patient satisfaction. Eur Urol 48:984–990
Reitz A, Stohrer M, Kramer G et al (2004) European experience of 200 cases treated with botulinum-A toxin injections into the detrusor muscle for urinary incontinence due to neurogenic detrusor overactivity. Eur Urol 45:510–515
Smith CP, Gangitano DA, Munoz A et al (2008) Botulinum toxin type A normalizes alterations in urothelial ATP and NO release induced by chronic spinal cord injury. Neurochem Int 52:1068–1075
Dixon J, Glosing J (1987) Structure and innervation in the human. In: Torrens M, Morrison JFB (eds) The physiology of the lower urinary tract. Springer, New York, pp 3–22
Brading A (1987) Physiology of bladder smooth muscle. In: Torrens M, Morrison JFB (eds) The physiology of the lower urinary tract. Springer, New York, pp 161–192
Akbar M, Abel R, Seyler TM et al (2007) Repeated botulinum-A toxin injections in the treatment of myelodysplastic children and patients with spinal cord injuries with neurogenic bladder dysfunction. BJU Int 100:639–645
Kuo HC (2004) Urodynamic evidence of effectiveness of botulinum A toxin injection in treatment of detrusor overactivity refractory to anticholinergic agents. Urology 63:868–872
Kuo HC (2005) Clinical effects of suburothelial injection of botulinum A toxin on patients with nonneurogenic detrusor overactivity refractory to anticholinergics. Urology 66:94–98
Schurch B, Denys P, Kozma CM et al (2007) Reliability and validity of the incontinence quality of Life questionnaire in patients with neurogenic urinary incontinence. Arch Phys Med Rehabil 88:646–652
Hori S, Patki P, Attar KH (2009) Patients’ perspective of botulinum toxin-A as a long-term treatment option for neurogenic detrusor overactivity secondary to spinal cord injury. BJU Int 104:216–220
Grosse J, Kramer G, Stohrer M (2005) Success of repeat detrusor injections of botulinum a toxin in patients with severe neurogenic detrusor overactivity and incontinence. Eur Urol 47:653–659
Schulte-Baukloh H, Knispel HH, Stolze T et al (2005) Repeated botulinum-A toxin injections in treatment of children with neurogenic detrusor overactivity. Urology 66:865–870
Dressler D, Hallett M (2006) Immunological aspects of botox, dysport and myobloc/neurobloc. Eur J Neurol 13(Suppl. 1):11–15
Herrmann J, Geth K, Mall V et al (2004) Clinical impact of antibody formation to botulinum toxin A in children. Ann Neurol 55:732–735
Acknowledgment
The source of funding for this research is China National Technology R&G Program, No. 2008BAI50B06.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, G., Liao, L. Injections of Botulinum Toxin A into the detrusor to treat neurogenic detrusor overactivity secondary to spinal cord injury. Int Urol Nephrol 43, 655–662 (2011). https://doi.org/10.1007/s11255-010-9873-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-010-9873-x