Abstract
Objective
Bowel preparation (BP) is performed routinely before intestinal surgery to reduce the risk of postoperative infectious complications. We studied the effect of BP on patients who underwent radical cystectomy and ileal conduit surgery. Our goal was to determine whether BP in these patients provided any benefits postoperatively.
Methods
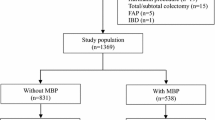
Between Match 2006 and January 2009, 86 patients scheduled for radical cystectomy and ileal conduit were randomized to preoperative BP (group A) or surgery without BP (group B). Outcomes studied included operative time, recovery of patient and surgical complications.
Results
Eighty-six patients were included in the study, 47 in group A and 39 in group B. All surgeries were performed successfully using ileum. Postoperative complications were documented in 5 and 6 patients in groups A and B, respectively. Anastomotic leak occurred in 1 patient in group A, leading to multiple organ dysfunction and sepsis, with a fatal outcome. One case of ileus and three wound infections were also seen in group A. In group B, wound infection and ileus occurred in two patients each, anastomotic leak developed in 1 patient resulting to reoperation and one patient died from pulmonary embolism. No statistical difference in the frequency of complications and recovery of patient was observed between the 2 groups.
Conclusions
Our results suggest that no advantage is gained by preoperative BP in radical cystectomy and ileal conduit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bowel Preparation(BP)is the standard of practice for patients undergoing colorectal surgeries. Urologists also accept it as dogma in reconstructive urological surgeries utilizing bowel segments.
Theoretically, reducing the bacterial load should reduce the rate of postoperative infection. However, recent multicentric trials have suggested that there was no evidence to support the use of BP in patients undergoing colorectal surgery [1, 2], and the benefit of BP in urologic reconstruction has also been questioned [3]. Therefore, we performed this trial comparing the outcomes and complication rates of ileal urinary diversion with and without BP.
Patients and methods
We studied prospectively 86 patients receiving ileal urinary diversion in our center from March 2006 to January 2009. Patients with a history of radiotherapy, immunosuppression, antibiotic administration within one preparative week, or liver and renal dysfunction were excluded. All patients were randomized to two groups: patients in group A (47 patients) received oral sodium phosphosoda (OSPS; two divided dose of Fleets phosphosoda 45 ml each, separated by 24 h), oral erythromycin 0.5 g tid and metronidazole 0.2 g tid for 2 days. Group B (39 patients) had no preoperative bowel preparation. All patients were allowed to a fluid diet for 24 h, with no oral intake 8 h before surgery. Intravenous third-generation cephalosporins was administered 1 h before surgery in both groups. The study protocol was approved by our Institutional Ethics Committee and written informed consent was obtained from all participants.
All urinary diversions performed used an ileal conduit after radical cystectomy. Intestinal lumens were cleansed by Benzalkonium Bromide (BB). A gastrostomy was required in all cases. All surgical procedures were performed by two experienced urologists. Intraoperative and postoperative routine management were same for all cases.
Statistical analysis
The t test was used to compare various parameters between the 2 groups, such as hospital stay, interval to oral diet, and operative time. Fisher’s exact test was used to calculate the differences in various complications between the 2 groups at level 0.05. Statistical analysis was done using SPSS, version 13.0 for Windows (SPSS, Chicago, IL).
Results
All patients tolerated BP and had ileal urinary diversion successfully performed. Characteristics, comorbid factors and complications after surgery in the two groups are shown in Table 1.
Both groups were similar with regard to age, sex and comorbid conditions. BP did not affect operative time or intestinal motility recovery. There were no significant differences in incidence of postoperative ileus, wound infection, anastomotic leak or mortality. There was one death in each group: the fatality in group A was a 74-year-old man who developed anastomotic leak after 5 days and underwent reoperation. Although he survived multiple organ dysfunction and sepsis postoperatively, he eventually died at home after 97 days. The fatality in group B was an 82-year-old man who had a massive pulmonary embolism. The anastomotic leak in group B was in a 67-year-old woman who required repeat enteroenterostomy. All wound infections and episodes of ileus in both groups resolved with standard therapy.
Discussion
The concept of bowel antisepsis and cleansing appeared in the 1940s and was generally accepted by the 1970s. The goal is to decrease the risk of infectious complications. This is theoretically accomplished by decreasing the bacterial load in the intestinal lumen and by decreasing the risk of spillage of feces in the operative field. Though most surgeons still practice bowel preparation of some form, challenges to the use of BP arose in the 1960s from surgeons who performed primary repair of colonic trauma, with good results in selected cases [4]. A recent systematic review by Guenaga et al. [5] carried out with meticulous selection of studies to prevent bias and type II error concluded that prophylactic mechanical bowel preparation prior to colorectal surgery had not been proven valuable and should be abandoned. Further, some aspects of BP have adverse effects, such as intestinal mucosal architectural change [6] and electrolyte disturbance in dehydrated or elderly patients [7, 8].
The ileum and colon are used most often for urinary tract reconstruction and have been employed in all types of reconstructive procedures. Methods of BP in urology follow the same principles used in General Surgery, although published data on BP for urinary diversion are limited. One group reported a day of BP for patients who underwent radical cystectomy and urinary diversion, with a satisfactory outcome [9].
However, there are negative aspects to BP as well. Patients needing radical cystectomy are usually older than 70, because invasive bladder cancer most commonly occurs beyond the 70th year of life [10]. As a result, medical comorbidities are common, and besides substantially reduced patient comfort, BP has been shown to cause severe side-effects such as electrolyte or acid–base imbalances and dehydration [11]. The liberal fluid infusion that is typically employed to reestablish intravascular volume intensifies these disturbances and causes tissue edema [12]. This problem prolongs wound healing and bowel function recovery time and increases reintervention rate, hospital stay, mortality and the incidence of severe cardiopulmonary complication [13].
The bacterial concentration ranges from 105 to 107 in the distal ileum, 106 to 108 in the ascending colon and 1010 to 1012 in the descending colon [14]. Recently, Jung B et al. [15] reported that mechanical bowel preparation did not affect the intramucosal bacterial colony count. In our center, our preference is to use ileum. Since BP was no longer universally advocated in colorectal surgery, withholding BP was therefore considered reasonable for procedures utilizing ileum, e.g. urinary diversion. Also patient acceptance was likely to be higher without BP.
Our study compared the effects of BP and withholding BP. Our results showed that BP did not reduce the infectious complication rate. We inferred that intravenous antibiotics and local use of BB provided adequate sterilization, and prevention of spillage could be achieved by stapling techniques. Thus, BP provided no demonstrable benefits in this patient population. These results support the observations of Ali Tabibi et al. [16] and Shafii et al. [17], although the first study was performed without random assignment and the latter was a retrospective analysis.
Although our study was prospective and randomized, the number of patients was relatively small. Moreover, our trial was not blinded. Large prospective randomized, double-blind series evaluating BP in urinary diversion using ileum would be needed to confirm our preliminary conclusion.
Conclusion
The results of this small study suggest that no advantage is gained by preoperative BP in radical cystectomy and ileal conduit. If these results are confirmed, surgery using ileum for urinary diversion could be safely performed without BP. Our experience supports the conclusion in colorectal surgery and implies the potential abandonment of BP in urinary diversion using ileum.
References
Jung B, Påhlman L, Nyström PO et al (2007) Multicentre randomized clinical trial of mechanical bowel preparation in elective colonic resection. Br J Surg 94:689–695. doi:10.1002/bjs.5816
Contant CM, Hop WC, van’t San HP et al (2007) Mechanical bowel preparation for elective colorectal surgery: a multicentre randomized trial. Lancet 370:2112–2117. doi:10.1016/S0140-6736(07)61905-9
Ferguson KH, McNeil JJ, Morey AF (2002) Mechanical and antibiotic bowel preparation for urinary diversion surgery. J Urol 167:2352–2356
LoCicero J 3rd, Tajima T, Drapanas T (1975) A half-century of experience in the management of colon injuries: changing concepts. J Trauma 15:575–579
Guenaga KK, Matos D, Wille-Jørgensen P (2009) Mechanical bowel preparation for elective colorectal surgery. Cochrane Database Syst Rev CD0001544. doi: 10.1002/14651858.CD001544.pub3
Bucher P, Gervaz P, Egger JF et al (2006) Morphologic alterations associated with mechanical bowel preparation before elective colorectal surgery: a randomized trial. Dis Colon Rectum 49:109–112. doi:10.1007/s10350-005-0215-5
Frizelle FA, Colls BM (2005) Hyponatremia and seizures after bowel preparation: report of three cases. Dis Colon Rectum 48:393–396. doi:10.1007/s10350-004-0778-6
Beloosesky Y, Grinblat J, Weiss A et al (2003) Electrolyte disorders following oral sodium phosphate administration for bowel cleansing in elderly patients. Arch Intern Med 163:803–808
Pruthi RS, Chun J, Richman M (2003) Reducing time to oral diet and hospital discharge in patients undergoing radical cystectomy using a perioperative care plan. Urology 62:661–665. doi:10.1016/S0090-4295(03)00651-4
American Cancer Society, Surveillance and Health Policy Research (2009) Probability of developing invasive cancers over selected age intervals by sex, US, 2003–2005. American CancerSocietyWeb.http://www.cancer.org/docroot/MED/content/downloads/MED_1_1x_CF F2009_Probability_Dev_Invasive_Cancer_Age_Inter.asp
Holte K, Nielsen KG, Madsen JL et al (2004) Physiologic effects of bowel preparation. Dis Colon Rectum 47:1397–1402. doi:10.1007/s10350-004-0592-1
Jacob M, Chappell D, Rehm M (2007) Clinical update: perioperative fluid management. Lancet 365:1984–1986. doi:10.1016/S0140-6736(07)60926-x
Brandstrup B, Tønnesen H, Beier-Holgersen R et al (2003) Effects of intravenous fluid restriction on postoperative complications: comparison of two perioperative fluid regimens: a randomized assessor-blinded multicenter trial. Ann Surg 238:641–648. doi:10.1097/01.sla.0000094387.50865.23
Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (2007) Campell-Walsh Urology. In: Dahl DM, Scott McDougal W (eds) Use of intestinal segments and urinary diversion, 9th edn. WB Saunders, Philadelphia Section XV, Chapter 80
Jung B, Matthiessen P, Smedh K et al (2010) Mechanical bowel preparation does not affect the intramucosal bacterial colony count. Int J Colorectal Dis 25:439–442. doi:10.1007/s00384-009-0863-3
Tabibi A, Simforoosh N, Basiri A et al (2007) Bowel preparation versus no preparation before ileal urinary diversion. Urology 70:654–658. doi:10.1016/j.urology.2007.06.1107
Shafii M, Murphy DM, Donovan MG et al (2002) Is mechanical bowel preparation necessary in patients undergoing cystectomy and urinary diversion? BJU Int 89:879–881. doi:10.1046/j.1464-410X.2002.02780.x
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xu, R., Zhao, X., Zhong, Z. et al. No advantage is gained by preoperative bowel preparation in radical cystectomy and ileal conduit: a randomized controlled trial of 86 patients. Int Urol Nephrol 42, 947–950 (2010). https://doi.org/10.1007/s11255-010-9732-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-010-9732-9