Abstract
Background
The relationship between parathyroid function, an important determinant of bone turnover, and bone mineral density (BMD) in patients with chronic kidney disease is not fully understood. We wanted to analyze the association between BMD and parathyroid function in hemodialysis patients in details.
Methods
In a cross-sectional design, data from 270 patients (age 55 ± 15 years, 60% men, all Caucasian) on maintenance hemodialysis were analyzed. All patients underwent dual energy X-ray absorptiometry of the lumbar spine (LS), femoral neck (FN) and distal radius (DR). In addition to routine laboratory tests, blood samples were collected for iPTH, serum markers of bone metabolism (alkaline phosphatase, type I collagen crosslinked-C-telopeptide) and 25OH vitamin D.
Results
Based on Z-scores, bone mineral density was moderately reduced only at the femoral neck in the total cohort. The average Z-score of the “low PTH” group (iPTH < 100 pg/ml) was not different from the Z-score of patients with iPTH in the “target range” (100–300 pg/ml) at any measurement site. While iPTH was negatively correlated with BMD at all measurement sites in patients with iPTH > 100 pg/ml (rho = −0.255, −0.278 and −0.251 for LS, FN and DR, respectively, P < 0.001 for all), BMD was independent of iPTH in patients with iPTH < 100 pg/ml. Furthermore, iPTH was not associated with serum markers of bone metabolism, but these markers were negatively correlated with BMD in the “low PTH” group.
Conclusions
Low PTH levels are not associated with low BMD in patients with end-stage kidney disease. Furthermore, bone metabolism seems to be independent of iPTH in patients with relative hypoparathyroidism likely reflecting skeletal resistance to PTH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Disorders of the mineral and bone metabolism are among the most prevalent complications of chronic kidney disease (CKD). They are responsible for disabling symptoms and consequences [1, 2], impaired quality of life [3] and even increased mortality [4]. CKD-associated mineral and bone disorder has been identified as a potential risk factor for cardiovascular morbidity and mortality in this patient population [1, 5]; hence, the term CKD-mineral and bone disorder (CKD-MBD) has been suggested to describe the complexity of the syndrome [2].
The prevalence of low BMD varies between 50 and 80% at the radius, 16–47% at the femoral neck and 13–29% at the lumbar spine, based on various studies in patients on hemodialysis [6]. Fracture rates are also very high among patients with CKD [4, 7, 8]. Similarly to the general population, low bone density in dialysis patients also seems to be related to fracture risk [9, 10]. This association, however, has not been consistently found in the different studies [11–14].
One reason for the conflicting results is that in patients with CKD, low BMD may coexist with a wide range of bone abnormalities, from high-turnover bone lesions in patients with secondary or tertiary hyperparathyroidism to profoundly reduced bone remodeling in patients with adynamic bone disease (ABD) [12, 15, 16]. Since bone strength is dependent on both bone density and bone quality [2, 17], extremes of bone turnover may have significant impact on fragility in addition to changes in BMD [18, 19].
Furthermore, the relationship between bone mineral density and bone turnover (as usually assessed by serum PTH concentration as a surrogate) [17, 20] is also very complex. Earlier studies did not find any relationship between BMD and turnover in dialyzed patients [14, 21, 22]. Subsequently, Taal et al. [23] reported that PTH was an independent negative predictor of BMD at the femoral neck and total hip. In a study involving 70 uremic patients, Urena et al. [9] found that high PTH was associated with low BMD only at the mid-radius. Gerakis et al. [12] reported that only femoral BMD was significantly reduced in patients with osteitis fibrosa assessed by bone biopsy but not in patients with ABD.
Significant hyperparathyroidism, i.e., serum iPTH > 300 pg/ml, usually associated with high bone turnover, is associated with low BMD [20]. It is much less clear whether ABD, usually associated with relatively low serum iPTH (relative hypoparathyroidism: iPTH < 100 or 150 pg/ml), is associated with reduced BMD or increased fracture risk. In a recent study, both high bone turnover and adynamic bone disease were associated with osteoporosis [16]. This problem is further complicated by the fact that ABD may be associated with aluminum toxicity and also with malnutrition. It has been repeatedly suggested, therefore, that studies are needed to investigate the relationships between BMD and fracture and between BMD and bone turnover in patients with CKD [15]. The aim of this cross-sectional study was to determine whether relative hypoparathyroidism, defined by serum iPTH < 100 pg/ml, likely reflecting low bone turnover, is associated with reduced bone mineral density compared to patients with iPTH in the target range. We also wanted to analyze the association between serum iPTH and bone metabolism across the full range of parathyroid function, including relative hypoparathyroidism. Finally, we wanted to identify factors associated with low BMD in patients on maintenance hemodialysis.
Methods
We performed a cross-sectional study including patients managed by maintenance hemodialysis. Patients from two dialysis units, where 418 patients received chronic hemodialysis during the study period between 1999 and 2004, were approached. Patients who were willing to participate and were able to commute to the diagnostic center were included in the study. One of the dialysis units was in the same building as the diagnostic center; consequently, patients from this unit, who needed transportation, were also included. A total of 270 patients, who had bone mineral density measurement and sufficient laboratory data (at least three serum Ca and P measurements within 6 months and one PTH measurement within 3 months prior to the densitometry), were included in the final analysis. The patients received three dialysis sessions per week; the mean treatment time was 230 ± 23 min per session.
Clinical information including demographic data, body weight and diagnosis of diabetes were collected from dialysis charts. Post-dialysis “target” weight, as determined by the most responsible nephrologist, was tabulated as “weight”. Patients with active hepatitis or who had been on HD for less than 3 months or had a history of parathyroidectomy were excluded from the analysis.
Bone densitometry (ODM) was assessed by dual-energy X-ray absorptiometry (DEXA) using a Norland XR 26 densitometer. Measurements were taken at three standard skeletal sites: lumbar spine (LS), femoral neck (FN) and distal third of radius (DR). Bone density and Z-scores (the number of standard deviations of the measured value from the mean value of age- and sex-matched reference population, established by the manufacturer) were tabulated. Z-scores were used in the analyses in order to control the association between density, age and gender.
Blood samples were taken before the mid-week dialysis sessions. Serum calcium was corrected for serum albumin level. For calcium and phosphorus, we calculated the mean of 3–6 monthly measurement values prior to the ODM. Serum intact PTH (pg/ml) was determined by second-generation electrochemiluminescence assay (iPTH Elecsys System; Roche, Mannheim, Germany) (normal range: 15–65 pg/ml). Type I collagen crosslinked-C-telopeptide (crosslaps, CRL) (pmol/l) was measured by the Serum Cross-Laps™ One Step ELISA (Osteometer BioTech A/S, Herlev, Denmark). Plasma levels of 25(OH)D3 vitamin were analyzed by a high-performance liquid chromatograph (HPLC) method using Bio-Rad reagents kit (Bio-Rad Laboratories, Inc., Hercules, Ca, USA). The 25(OH)D3 and CRL were measured once, within 2 weeks from the densitometry. Similarly, only one measurement of PTH and alkaline phosphatase (ALP) was included in the study dataset.
To obtain cohorts that were likely to correspond to low, normal or high bone turnover, patients were grouped into three groups based on serum iPTH results: “low PTH” (“relative hypoparathyroidism”, likely reflecting low bone turnover): serum iPTH < 100 pg/ml; “target PTH”: iPTH 100–300 pg/ml; and “high PTH”: iPTH > 300 pg/ml (corresponding to secondary or tertiary hyperparathyroidism and high likelihood of high-turnover bone disease).
Statistical analysis was carried out using the SPSS 15.0 software. The data were summarized using proportions, means (± standard deviation, SD) or median (interquartile range, IQR), as appropriate. Continuous variables were compared using Student’s T test, ANOVA, Mann–Whitney U test or Kruskal–Wallis test, and categorical variables were analyzed with the chi-square test. In analysis of variance, Scheffe’s multiple comparison was used to detect significant differences between patient groups. In all statistics, two-sided test was used and the results have been recognized statistically significant when alpha was < 0.05. Potentially important associations were evaluated using Pearson or Spearman correlation and were also tested for significance in multiple regression equations. Multivariate linear and logistic regression models were used to analyze the predictors of bone density. Significant or nearly significant (alpha < 0.1) predictors in bivariate analyses were entered into the multivariate models. The groups formed by serum iPTH were represented by dummy variables in the multivariate models. Residual plots were used to confirm linear relationship, and polynomial terms were introduced when appropriate. Variance influence factors (VIF) were used to indicate collinearity between independent variables in the multivariate regression models. Influential outliers were detected calculating Cook’s distances. Goodness-of-fit was tested using R 2 in linear and the Hosmer–Lemeshow test in logistic regression. No imputation method was used to replace missing data. In multivariate analyses, cases with missing data were excluded analysis by analysis.
Results
A total of 270 patients, all Caucasians, were included in the analysis. 60% were men, the prevalence of diabetes mellitus was 28% and mean age was 55 ± 15 years. Of the 107 women, 97 were post-menopausal. Basic demographic and clinical characteristics are summarized in Table 1. The most prevalent underlying kidney disease was chronic glomerulonephritis (29%). The prevalence of other kidney diseases was: diabetic nephropathy 26%, chronic pyelonephritis and chronic tubulo-interstitial disease 15%, hypertensive nephrosclerosis and analgetic nephropathy 12%, autosomal dominant polycystic kidney disease 8%, other or unknown 10%. The median duration of end-stage renal disease was 16.5 months (3–279 months). Among the patients, 12.6% had previously received steroid treatment either for their primary kidney disease or for renal transplantation.
Seventy-three percent of patients received calcium carbonate as phosphate binder. Occasionally in some patients, in case of hypercalcemia, a magnesium-containing antacid (magnesium trisilicicum + magnesium oxide) was added to calcium carbonate or was temporarily used instead of the calcium-based binder. Only a minority (2%) of patients received sevelamer HCl. Of all patients, 31% were treated with active vitamin D compounds, exclusively in the form of oral calcitriol (Table 1).
Table 1 also shows the basic demographic and laboratory parameters for the three groups formed by serum iPTH: “low PTH” (serum iPTH 1–100 pg/ml); “target PTH” (serum iPTH 101–300 pg/ml); “high PTH” (serum iPTH > 300 pg/ml). As expected, serum phosphorus levels were significantly higher in the “high PTH” group, while calcium levels were higher in the “low PTH” group. Serum alkaline phosphatase (ALP) and CRL correlated well with iPTH and were significantly different between the three groups. A trend of decreasing 25-OH-vitamin D level from the “low” to the “high PTH” group was seen but the difference did not reach statistical significance. However 25-OH-vitamin D level, correlated inversely with serum iPTH in the study population (Table 4).
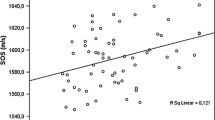
Bone density was higher in men than in women at all sites (distal radius: 1.11 vs. 0.69 g/cm2, femoral neck: 0.78 vs. 0.71 g/cm2 and lumbar spine: 1.04 vs. 0.90 g/cm2; P < 0.001 for all). BMD measured at the femoral neck (r = −0.339, P < 0.001) and distal radius (r = −0.183, P = 0.003), but not at the lumbar spine, was negatively correlated with age. For further analysis, we used Z-scores in order to control for the effect of age and gender on bone mass. Based on Z-scores, bone mineral density measured at the femoral neck was moderately reduced in the total study cohort, whereas Z-scores for the lumbar spine and distal radius were not reduced (Table 1). Patients in the “high PTH” group had significantly lower Z-scores at all measurement sites compared to patients in either the “target” or the “low PTH” groups. The average Z-score of the “low PTH” group, however, was not different from the average Z-score of patients who were in the “target PTH” group, at all measurement sites (Table 1; Fig. 1).
Z-scores were positively correlated with the patients’ weight. Interestingly, Z-scores were also positively correlated with age (Table 2). Diabetic patients had significantly higher Z-scores at the lumbar spine (0.57 vs. −0.28, P = 0.002) and at the radius (0.09 vs. −0.78, P < 0.001) but not at the femoral neck.
Z-scores were negatively correlated with biochemical markers of bone remodeling, namely ALP and CRL, at all measurement sites (Table 2). Z-scores measured on the femoral neck and lumbar spine also showed significant negative correlation with PTH. The association between PTH and Z-score on the distal radius was far from linear: it demonstrated a reversed U-shaped curve with a turning point at PTH = 100 pg/ml (Fig. 2). In order to control for the effect of PTH in the multivariate analysis, a polynomial regression equation using PTH square [24] was created to fit the model to the unique shape of this relationship (Table 3).
To determine whether iPTH was independently associated with bone mineral density, we constructed multivariate regression models—one for each measurement site—with Z-scores being the dependent variable. Variables associated significantly with Z-scores in bivariate analyses were entered in the model as independent variables. To avoid multi-collinearity, only ALP and not CRL was entered into the model. In the multivariate analysis, a distinct pattern of associations was seen for the radius on one hand and for the femoral neck and lumbar spine on the other. Body weight, Ca × P product and serum iPTH were independent predictors of bone density at all measurement sites. Higher weight, higher Ca × P product and lower iPTH were associated with higher Z-scores, independent of the other variables tested in the models. Interestingly, increasing age and female gender were independently associated with higher Z-scores at the femoral neck and the lumbar spine but not at the radius. Longer duration of ESRD was associated with decreased Z-score only at the radius, whereas higher ALP (reflecting higher bone turnover) was associated with reduced Z-score (independently of serum iPTH) both at the radius and at the femoral neck, but not at the lumbar spine. Finally, diabetes was independently associated with higher density at the radius and the lumbar spine (Table 3).
In the next step, we performed a set of analyses in which we focused on the “low PTH” group in order to elucidate the relationship between parathyroid function and bone metabolism in patients with “relative hypoparathyroidism” and likely low bone turnover. In this group, serum iPTH and Z-scores were not correlated at any sites, whereas in patients with serum iPTH above 100 pg/ml, the expected negative correlation was seen between the two variables at all sites (Tables 2, 4; Fig. 2). Next we examined the relationship between Z-score and biochemical markers of bone turnover. Within the “low PTH” group, the association between Z-score and CRL (distal radius: rho = −0.493, P = 0.001; femoral neck: rho = −0.294, P = 0.077, lumbar spine: rho = −0.303, P = 0.057), and also between Z-scores and ALP (distal radius: rho = −0.260, P = 0.012, lumbar spine: rho = −0.244, P = 0.021) was similar to the associations in the total population (Table 2). In a set of sensitivity analyses, different PTH cut-off points (65 and 150 pg/ml) were used to define the “low PTH” group; in both analyses, qualitatively similar results were seen.
Finally, the association between iPTH and biochemical markers of bone turnover was assessed. As expected, highly significant positive correlations were found between iPTH versus ALP (rho = 0.333, P < 0.001) or CRL (rho = 0.388, P < 0.001) in the total population. No correlation, however, was seen between iPTH and either ALP (rho = −0.110, P = NS) or CRL (rho = 0.126, P = NS) in patients with “low PTH” (Table 4).
Discussion
In this study we report data which suggest that relative hypoparathyroidism in hemodialysis patients, likely corresponding to adynamic bone disease, is not associated with reduced BMD compared to patients with serum iPTH in the recommended target range. The presented data also confirm that secondary hyperparathyroidism is associated with significantly reduced bone density at all measurement sites whereas patients with normal or low iPTH only had significant reduction of bone density at the femoral neck compared to the age- and gender-adjusted general population.
A PTH level less than 195 pg/ml was associated with a 5.8-fold increase in risk of hip fracture in a local registry data analysis by Coco et al. [18]. Bone mineral density, however, was not measured in that study. It is possible that the association between low PTH and fracture risk in this study was in part the result of malnutrition, suggested by the low serum albumin in that study. Patients with PTH levels in the lowest tercile had higher fracture prevalence in the study published by Atsumi et al. [25]. In this paper, PTH was not correlated with BMD at the lumbar spine. When interpreting these results, however, the potential aluminum exposure of the enrolled patients has to be considered, since during and prior to the study period the use of aluminum-based phosphate binders was relatively prevalent in Japan. In our cohort, nutritional status was good (mean albumin level 40 g/l) and the exposure to aluminum-based phosphate binders was minimal. Furthermore, the aluminum content of the ultrapure dialysate used by the participating dialysis units was minimal.
Differences in the characteristics of the populations studied could certainly explain some of the differences between the findings in the literature. Furthermore, cortical (represented by the distal radius and, to some extent, the femoral neck) and trabecular bone respond differently to the effects of PTH and likely to the effects of uremia, as well. The artifact introduced by spinal osteophytes and the calcification of the abdominal aorta and other large blood vessels could have also contributed to the differences between different studies. Finally, the non-linear association between serum iPTH and BMD could also, in part, be responsible for the conflicting results.
A negative correlation between serum iPTH and BMD measured at different sites was reported by several researchers [9, 23, 26], but the linearity of this association was not analyzed. Gerakis et al. reported that vertebral BMD was not different between the different types of renal osteodystrophy (ROD) assessed by bone biopsy. On the other hand, femoral BMD was significantly reduced in patients with osteitis fibrosa but not in patients with adynamic bone disease on the bone biopsy [12]. Since we did not perform bone biopsy, we cannot comment on the association between different types of ROD and BMD. Our results, however, are in accord with the findings of Gerakis et al. concerning the lack of substantial reduction of BMD in patients with low iPTH (relative hypoparathyroidism).
We want to emphasize, however, that despite the apparently sufficient bone mass, adynamic bone disease is not the preferred state of bone, since it may be associated with vascular calcification, cardiovascular mortality [27–30] and likely increased risk of bone fracture as well [18, 30].
The NKF K/DOQI guideline suggests that 150 pg/ml should be used as lower limit for the normal range of PTH in patients with ESRD. Lower cut-off of 120 pg/ml [31] or even 65 pg/ml [32, 33] was used in several studies. We observed an inverse U-shaped relationship between PTH and bone density at the radius in our dataset. The curve had a nadir at 100 pg/ml; therefore, we chose this cut-off point to identify patients with “low” PTH.
The guideline suggested cut-off was primarily derived from one study [34] in which previous aluminum exposure from phosphate binders might have been an issue. [35, 36] It has been suggested that a different target PTH range should be used in patients with versus those without significant aluminum deposition in the bone. [37] Data from patients without evidence of aluminum intoxication on bone biopsy were analyzed in a study in Toronto [20]. Based on their findings, the authors suggested 100 pg/ml as the lower limit for the target range of PTH. Fournier et al. [37] also biopsied patients who have never been exposed to aluminum and suggested an even lower cut-off; however, the assay used for PTH measurement was different from other studies.
In our study, 300 pg/ml was used as cut-off to define high remodeling rate, according to the NKF K/DOQI guideline. iPTH levels above this limit in our dataset (“high PTH” group) were associated with significantly reduced Z-score similarly to previous reports [9, 23]. This was true for all measured sites (radius, femur and the spine). These results are in agreement with the recommendations of the guideline to maintain iPTH below 300 pg/ml in hemodialysis patients.
Patients in the “high PTH” group tended to have lower 25(OH)D3 levels compared to the other groups. The majority of the study cohort was vitamin D deficient. The use of calcitriol was the most prevalent in the high-PTH group without any nutritional vitamin D utilization. This reflects the approach suggested by the treatment guidelines at the time of the data collection. In fact, the current NKF K/DOQI guideline does not recommend the use of nutritional vitamin D for the treatment of hyperparathyroidism because of the lack of proper randomized controlled trials. Observational studies, however, suggested an association between serum 25(OH)D3 vitamin level and PTH [38]. Furthermore, 25(OH)D3 supplementation resulted in a reduction of serum PTH in a more recent study [39]. Consequently, we feel it is prudent to correct vitamin D deficiency or insufficiency even in dialysis-dependent patients. This approach has also been suggested by others, as well [35].
Interestingly, we found no association between iPTH and BMD or between iPTH and serum markers of bone turnover in hemodialysis patients with iPTH levels below 100 pg/ml, who are at high risk of having adynamic bone disease. Importantly, the expected significant negative associations between those parameters were found in patients with serum iPTH > 100 pg/ml.
Ueda et al. [40] reported earlier that there was no association between BMD and PTH in patients with iPTH < 180 pg/ml. However, they did not assess the association between iPTH and markers of bone metabolism or between bone markers and BMD to further characterize this phenomenon. It is possible that the observed lack of effect of PTH on bone in the relatively low range of 0–100 pg/ml reflects the resistance of the skeleton against PTH, as suggested by others [41, 42]. Serum ALP, which is frequently used to assess osteoblast activity, and serum crosslaps, which reflects bone resorption, were both significantly correlated with BMD even in the low iPTH range suggesting that the bone of those patients is not completely “dormant” and bone turnover is associated with BMD even in this subset of patients. At the same time, both ALP and crosslaps levels were independent of serum iPTH, further suggesting that bone metabolism is largely independent of PTH in those patients.
Alternatively, it is possible that the apparent independence of bone metabolism seen in our patients with measured iPTH levels < 100 pg/ml is due to the fact that what we measured is not the active hormone but, to some extent, inactive peptide fragments [43]. Although we cannot completely exclude this possibility, we believe that this could not fully explain the observed results. Serum PTH values obtained by the older assays (also utilized in this study), which cross-react with amino-terminally truncated PTH fragments, correlate closely with results obtained with the newer Bio-Intact PTH assay, which only measures the full length hormone [17, 44]. Furthermore, the values obtained with the older assays are only about twice as high as obtained with the Bio-intact assay. This means that an association between iPTH levels and BMD or serum markers of bone metabolism should have been detected in our analysis if it existed. Therefore, we suggest that our finding reflects the functional resistance of the skeleton to iPTH in dialysis patients.
We cannot completely rule out that the lack of association is a result of small dispersion in the iPTH measurements. We feel, however, that this is unlikely, since similar lack of association was previously observed by other authors as well [40] while an association between serum PTH and BMD at the hip was demonstrated in a study among healthy individuals [45] where PTH was in normal range (i.e., the dispersion of data was even less). Furthermore, in a yet unpublished analysis assessing the association between serum PTH and markers of bone metabolism, we did find an association between serum PTH and serum markers of bone turnover (which we did not see in patients on dialysis) in the patient group with serum PTH less than 100 pg/ml, but the association was absent in patients with serum PTH below 65 pg/ml (Mucsi et al., unpublished observation).
Although the use of calcium carbonate and calcitriol was the lowest in the “low PTH” group, the difference between the three groups was not significant. It is possible therefore that patients in the “low PTH” group were overtreated with calcium carbonate and calcitriol.
We found a positive correlation between Z-scores and age in our patients. This is somewhat surprising as the Z-score is already corrected for age. This may mean that the association between age and bone mineral density is somewhat similar to the association between age and cardiovascular risk in dialysis patients. Accordingly, the reduction in BMD is relatively larger in younger dialysis patients compared to age- and gender-matched controls (i.e., the Z-score is a bigger negative number) whereas in elderly individuals the difference between dialysis patients and matched controls is relatively less.
In contrast to earlier findings, the prevalence of diabetes mellitus was not higher in our low-iPTH group and the average iPTH levels were similar in diabetics versus non-diabetics. However, the relationship between DM and low bone turnover cannot be assessed in our dataset, due to the lack of bone histology. Patients with diabetes had higher bone density on the radius and at the lumbar spine. This is consistent with earlier observations in patients with type 2 diabetes, where diabetes was associated with higher bone density and low bone turnover [46, 47]. Possible explanation for this phenomenon is the anabolic effect of insulin on bone in hyperinsulinaemia, since the insulin resistance is restricted to the effect of insulin on the glucose transport. The reason why we could not detect a difference in the BMD measured at the femoral neck between patients with or without diabetes is not known. Increased calcification of the aorta in diabetes can also interfere with BMD measurement at the lumbar spine.
Several limitations of this study need to be noted. Bone biopsy was not carried out in this large dialysis population; therefore, we could not assess the association between bone turnover and BMD. Although serum iPTH has a high positive predicting value in identifying high-turnover bone disease, bone turnover cannot be predicted with sufficient accuracy in dialysis patients if iPTH is below 300 pg/ml [12, 20].
We used the total alkaline phosphatase to assess osteoblastic activity since the bone isoenzyme was measured only in a minority of our population. Other isoenzymes of ALP, such as liver or intestine could have introduced bias into our analyses, although we excluded patients with active liver disease from the analysis. The differences in ALP between the three PTH groups were disproportionate compared to the differences in PTH levels. The use of total ALP instead of the bone-specific isoenzyme could partly explain this discrepancy. In addition, several other factors influence the actual bone turnover and its resistance to PTH, such as genetic factors, inflammatory cytokines, aluminum exposure, uremic toxins, estrogen insufficiency, that can also result in discrepancy in the levels of PTH and turnover markers.
Although we did not measure serum aluminum in our patients, we believe that aluminum toxicity did not influence our results significantly. Aluminum-containing phosphate binders were generally avoided and were administered only for short time periods not exceeding 4 weeks. Furthermore, according to local regulations, the aluminum content of the city tap water was less than 200 μg/l. The aluminum content of the ultrapure water produced by the water treatment system in the dialysis units involved has regularly been tested, and aluminum concentrations were consistently below the specified threshold of 5 μg/l.
There are limitations to the use of DEXA in patients with ESRD, as well. DEXA uses projective technique to measure the mineral content in the bone corresponding to the projected area. Cortical and cancellous bone structures will be superimposed making it impossible to differentiate between the two bone compartments. In addition, hyperparathyroidism can have opposite effects in these two different bone structures. Changes in bone ultrastructure may also affect DEXA results making it impossible to differentiate between mineralization defect and volume loss.
In summary, we reported here that bone mineral density in dialysis patients with relative hypoparathyroidism (iPTH < 100 pg/ml) was similar to patients with serum iPTH in the target range of 100–300 pg/ml. Furthermore, both BMD and bone turnover, as assessed by serum crosslaps and ALP, were independent of PTH in patients with relative hypoparathyroidism.
The association between fracture risk, BMD and bone turnover needs further studies that utilize bone biopsy.
References
Moe SM et al (2007) Chronic kidney disease-mineral-bone disorder: a new paradigm. Adv Chronic Kidney Dis 14(1):3–12
Moe S et al (2006) Definition, evaluation, and classification of renal osteodystrophy: a position statement from kidney disease: improving global outcomes (KDIGO). Kidney Int 69(11):1945–1953
Johansen KL, Chertow GM (2007) Chronic kidney disease mineral bone disorder and health-related quality of life among incident end-stage renal-disease patients. J Ren Nutr 17(5):305–313
Mittalhenkle A, Gillen DL, Stehman-Breen CO (2004) Increased risk of mortality associated with hip fracture in the dialysis population. Am J Kidney Dis 44(4):672–679
Toussaint ND et al (2008) Associations between vascular calcification, arterial stiffness and bone mineral density in chronic kidney disease. Nephrol Dial Transplant 23(2):586–593
Ersoy FF (2007) Osteoporosis in the elderly with chronic kidney disease. Int Urol Nephrol 39(1):321–331
Alem AM et al (2000) Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 58(1):396–399
Jadoul M et al (2006) Incidence and risk factors for hip or other bone fractures among hemodialysis patients in the dialysis outcomes and practice patterns study. Kidney Int 70(7):1358–1366
Urena P et al (2003) Bone mineral density, biochemical markers and skeletal fractures in haemodialysis patients. Nephrol Dial Transplant 18(11):2325–2331
Jamal SA, Hayden JA, Beyene J (2007) Low bone mineral density and fractures in long-term hemodialysis patients: a meta-analysis. Am J Kidney Dis 49(5):674–681
Ersoy FF et al (2006) Bone mineral density and its correlation with clinical and laboratory factors in chronic peritoneal dialysis patients. J Bone Miner Metab 24(1):79–86
Gerakis A et al (2000) Correlation of bone mineral density with the histological findings of renal osteodystrophy in patients on hemodialysis. J Nephrol 13(6):437–443
Jamal SA et al (2002) Bone density and heel ultrasound testing do not identify patients with dialysis-dependent renal failure who have had fractures. Am J Kidney Dis 39(4):843–849
Merino JL et al (2004) Changes in bone mineral density during the first year of dialysis treatment. Int Urol Nephrol 36(2):285–286
Cunningham J et al (2004) Osteoporosis in chronic kidney disease. Am J Kidney Dis 43(3):566–571
Barreto FC et al (2006) Osteoporosis in hemodialysis patients revisited by bone histomorphometry: a new insight into an old problem. Kidney Int 69(10):1852–1857
Martin KJ et al (2004) Diagnosis, assessment, and treatment of bone turnover abnormalities in renal osteodystrophy. Am J Kidney Dis 43(3):558–565
Coco M, Rush H (2000) Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 36(6):1115–1121
Danese MD et al (2006) PTH and the risks for hip, vertebral, and pelvic fractures among patients on dialysis. Am J Kidney Dis 47(1):149–156
Wang M et al (1995) Relationship between intact 1–84 parathyroid hormone and bone histomorphometric parameters in dialysis patients without aluminum toxicity. Am J Kidney Dis 26(5):836–844
Eeckhout E et al (1989) Monitoring of bone mineral content in patients on regular hemodialysis. Nephron 52(2):158–161
Lechleitner P et al (1994) Bone mineral densitometry in dialyzed patients: quantitative computed tomography versus dual photon absorptiometry. Bone 15(4):387–391
Taal MW et al (1999) Risk factors for reduced bone density in haemodialysis patients. Nephrol Dial Transplant 14(8):1922–1928
Kleinbaum DG, Kupper LL, Muller KE, Nizam A (eds) (1998) Applied regression analysis and other multivariable methods, 3rd edn. Duxbury Press, Pacific Grove, pp 281–316
Atsumi K et al (1999) Risk factors for vertebral fractures in renal osteodystrophy. Am J Kidney Dis 33(2):287–293
Dolgos S et al (2008) Determinants of bone mass in end-stage renal failure patients at the time of kidney transplantation. Clin Transpl 22(4):462–468
Guh JY et al (2002) Risk factors and risk for mortality of mild hypoparathyroidism in hemodialysis patients. Am J Kidney Dis 39(6):1245–1254
London GM et al (2003) Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transpl 18(9):1731–1740
London GM et al (2004) Arterial calcifications and bone histomorphometry in end-stage renal disease. J Am Soc Nephrol 15(7):1943–1951
Spasovski GB (2007) Bone health and vascular calcification relationships in chronic kidney disease. Int Urol Nephrol 39(4):1209–1216
Torres A et al (1995) Bone disease in predialysis, hemodialysis, and CAPD patients: evidence of a better bone response to PTH. Kidney Int 47(5):1434–1442
Hutchison AJ et al (1993) Correlation of bone histology with parathyroid hormone, vitamin D3, and radiology in end-stage renal disease. Kidney Int 44(5):1071–1077
Gerakis A et al (1996) Biochemical markers for non-invasive diagnosis of hyperparathyroid bone disease and adynamic bone in patients on haemodialysis. Nephrol Dial Transpl 11(12):2430–2438
Quarles LD, Lobaugh B, Murphy G (1992) Intact parathyroid hormone overestimates the presence and severity of parathyroid-mediated osseous abnormalities in uremia. J Clin Endocrinol Metab 75(1):145–150
Monge M et al (2006) Reappraisal of 2003 NKF-K/DOQI guidelines for management of hyperparathyroidism in chronic kidney disease patients. Nat Clin Pract Nephrol 2(6):326–336
Shahapuni I et al (2005) How do calcimimetics fit into the management of parathyroid hormone, calcium, and phosphate disturbances in dialysis patients? Semin Dial 18(3):226–238
Fournier A et al (1997) The clinical significance of adynamic bone disease in uremia. Adv Nephrol Necker Hosp 27:131–166
Ghazali A et al (1999) Is low plasma 25-(OH)vitamin D a major risk factor for hyperparathyroidism and Looser’s zones independent of calcitriol? Kidney Int 55(6):2169–2177
Jean G et al (2008) Daily oral 25-hydroxycholecalciferol supplementation for vitamin D deficiency in haemodialysis patients: effects on mineral metabolism and bone markers. Nephrol Dial Transpl 23(11):3670–3676
Ueda M et al (2005) Serum BAP as the clinically useful marker for predicting BMD reduction in diabetic hemodialysis patients with low PTH. Life Sci 77(10):1130–1139
Drueke TB (1996) Abnormal skeletal response to parathyroid hormone and the expression of its receptor in chronic uremia. Pediatr Nephrol 10(3):348–350
Urena P et al (1996) PTH/PTHrP receptor mRNA is down-regulated in epiphyseal cartilage growth plate of uraemic rats. Nephrol Dial Transpl 11(10):2008–2016
Slatopolsky E et al (2000) A novel mechanism for skeletal resistance in uremia. Kidney Int 58(2):753–761
Lehmann G et al (2005) Specific measurement of PTH (1–84) in various forms of renal osteodystrophy (ROD) as assessed by bone histomorphometry. Kidney Int 68(3):1206–1214
Sneve M et al (2008) The association between serum parathyroid hormone and bone mineral density, and the impact of smoking: the Tromso study. Eur J Endocrinol 158(3):401–409
Pei Y et al (1993) Renal osteodystrophy in diabetic patients. Kidney Int 44(1):159–164
van Daele PL et al (1995) Bone density in non-insulin-dependent diabetes mellitus. The Rotterdam study. Ann Intern Med 122(6):409–414
Acknowledgments
This study was supported by grant from the ETT of the Ministry of Health (172/2006), the Hungarian Kidney Foundation and the Foundation for Prevention in Medicine. This paper was supported by the János Bolyai Research Scholarship of the Hungarian Academy of Sciences (Miklos Zsolt Molnar).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ambrus, C., Almasi, C., Berta, K. et al. Bone mineral density and parathyroid function in patients on maintenance hemodialysis. Int Urol Nephrol 43, 191–201 (2011). https://doi.org/10.1007/s11255-009-9702-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-009-9702-2