Abstract
Background
Recently, there have been a few reports on the decrease in the incidence of severe Henoch-Schönlein purpura nephritis (HSPN) in Japan. To evaluate the incidence and the severity of HSPN, we examined the epidemiology and clinical manifestations of HSPN in Fukushima Prefecture over a 22-year period.
Methods
We enrolled 61 patients (Group 1) diagnosed with HSPN between 1987 and 1997 and a further 59 patients (Group 2) diagnosed with HSPN between 1998 and 2008. Epidemiology, clinical features, laboratory data, pathological findings, treatment and outcome were retrospectively compared between the two groups.
Results
The mean number of patients per 100,000 children per year was 3.5 ± 1.2 in Group 1 and 3.6 ± 0.8 in Group 2. The clinical manifestations and laboratory findings at onset were comparable between Groups 1 and 2. Pathological findings in Group 1 and Group 2 were classified as ISKDC grade IIIa in 16 (26%) and 14 cases (24%), grade IIIb in 26 (43%) and 27 cases (46%), grade IV in 5 (8%) and 6 cases (10%)), grade V in 1 (2%) and 5 cases (8%), and grade VI in 2 (3%) and 2 cases (3%), respectively. There were no inter-group differences in ISKDC classification or rate of crescentic formation.
Conclusions
Our findings suggest that the incidence of HSPN and the severity of HSPN in patients between 1987 and 1997 were similar to those in patients between 1998 and 2008 and that the number of patients with severe HSPN has not decreased.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Henoch-Schönlein purpura (HSP) is an immunoglobulin A (IgA)-mediated immune-complex vasculitis affecting predominantly the skin, joints, gastrointestinal tract, and kidneys. It occurs most frequently in childhood, and the prognosis for HSP patients is largely predicted by the severity of renal involvement [1].
The epidemiology of HSP is obscure, and the proportion of patients reported to have renal involvement varies between 30 and 80% [1–4].
Recently, Trapani et al. [2] reported that 77 (54%) of 150 patients with HSP had renal involvement, 11 (7%) had severe nephropathy, and 3 (2%) had acute renal insufficiency. The majority of children with Henoch-Schönlein nephritis (HSPN) presenting with only hematuria and/or low-grade proteinuria have a good chance of recovery. However, patients with massive proteinuria at onset frequently show a progressive course [4–8].
As to the changes in the onset rate of HSPN in Japan, Moriya et al. [9] investigated 30 patients diagnosed with HSPN between 1971 and 1982 and 11 patients diagnosed with HSPN between 1985 and 1996 and found that the severity of the renal histopathologic findings was lower in the 11 patients with HSPN diagnosed between 1985 and 1996. However, apart from the above report, there have been no reports on the changes in the incidence of HSPN. Thus, we investigated the epidemiology and clinical manifestations of HSPN over a 22-year period in Fukushima Prefecture, Japan, to evaluate changes in the rate of onset and severity of HSPN.
Patients and methods
This study was carried out at Fukushima Medical University Hospital, Fukushima Red Cross Hospital, Soma General Hospital, Ohara General Hospital, Hoshi General Hospital, Shirakawa General Hospital, Iwase General Hospital and Takeda General Hospital. Informed consent was obtained from all patients or their parents.
Patients
Between January 1987 and December 2008, 120 children were newly diagnosed with HSPN at the Department of Pediatrics, Fukushima Medical University School of Medicine, Fukushima Red Cross Hospital, Soma General Hospital, Ohara General Hospital, Hoshi General Hospital, Shirakawa General Hospital, Iwase General Hospital and Takeda General Hospital. These children were divided into two groups according to the time of onset of HSPN. Group 1 consisted of 61 patients who had been diagnosed with HSPN between 1987 and 1997, and Group 2 consisted of 59 patients who had been diagnosed with HSPN between 1998 and 2008.
Epidemiology, clinical features, laboratory data, pathological findings, treatment and prognosis were retrospectively investigated for both groups.
Definitions
Hematuria was defined as microscopic urine examination showing five or more red blood cells per high-power field, and macrohematuria was diagnosed if the same number of red blood cells were visible with the naked eye [10]. Proteinuria was evaluated by 24-h quantitative measurement. Nephrotic syndrome was defined as the presence of proteinuria (≥40 mg/m2/h) and a serum albumin level of less than 2.5 g/dl, with or without edema [10, 11]. A diagnosis of HSP was made if the major manifestations of the illness consisted of a purpuric rash and abdominal pain without thrombocytopenia. Additional features including arthritis and nephritis were accepted as being consistent with the diagnosis. The criteria for renal biopsy were defined as follows: (1) the patients had proteinuria of 20 mg/m2/h or greater and hematuria or (2) the patients had proteinuria of less than 20 mg/m2/h and recurrent macrohematuria.
The clinical status of each patient at the latest observation was classified as follows.
Stage (A)-normal: the patient was normal on physical examination, with normal urine and renal function.
Stage (B)-minor urinary abnormalities: the patient was normal on physical examination, with microscopic hematuria or proteinuria of less than 20 mg/m2/h.
Stage (C)-persistent nephropathy: the patient had proteinuria of 20 mg/m2/h or greater or hypertension and a 24-h creatinine clearance (24hCcr) of 60 ml/min/1.73 m2 or greater.
Stage (D)-renal insufficiency: the patient had a 24hCcr of less than 60 ml/min/1.73 m2 (including dialysis/transplant or death).
Pathology
First, renal biopsies were performed in all patients. The mean numbers of glomeruli found in the biopsy specimens were 23.8 ± 10.3 (range 11–36). The specimens were assessed by light microscopy (LM) and immunofluorescence (IF). Material for histological study was fixed in 12% neutral formalin, embedded in paraffin, sectioned at a thickness of 2–3 μm and stained with hematoxylin and eosin or periodic acid-Schiff reagent.
The glomerular changes were graded according to the classification devised by the pathologists of the International Study of Kidney Disease in Children [12].
Treatment
Following diagnostic renal biopsy, the patients with grade 1 or 2 findings were treated with anti-platelet agents (dipyridamole 5 mg/kg/day), whereas patients with grade IIIb findings were treated with daily oral prednisolone (1 mg/kg/day) for a period of more than 6 months, along with anti-platelet agents and warfarin. Warfarin was given orally in a single morning dose of 1 mg (for patients aged less 7 years) or 2 mg (for those aged over more than 7 years or over) to maintain the thrombo-test level at 30–50%. Patients with grade IIIb findings were treated with MUP therapy. MUP therapy consisted of a combination of pulse methylprednisolone at 30 mg/kg/day i.v. bolus (maximum 1 g) for three consecutive days and pulse urokinase at 5,000 u/kg/day i.v. bolus (maximum 180,000 u) for seven consecutive days, followed by daily oral prednisolone (1 mg/kg/day) for a period of more than 6 months, along with anti-platelet agents and anti-coagulant [13]. The patients with grade VI or higher findings were treated with MUP therapy plus cyclophosphamide. Cyclophosphamide was given orally at 2.5 mg/kg/day for 12 weeks [14]. Patients with greater than ISKDC grade V were treated with plasmapheresis (PP) [15].
Statistics
Data are expressed as mean values ± SEM. Statistical analysis was performed on a Macintosh computer using a Stat View software package (Abacus Concepts, Berkeley, Calif., USA). Several variables, which were clearly not in a normal distribution, were compared using non-parametric statistics such as Mann–Whitney test or Wilcoxon test. A P value <0.05 was considered significant.
Results
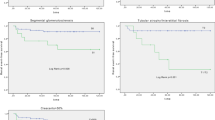
Inter-group comparison of patient characteristics at the onset of symptoms (Table 1; Figs. 1, 2, 3)
Age at onset (years) and male-to-female ratio were 8.8 ± 3.1 and 1.03, respectively, in Group 1 and 8.5 ± 3.2 and 0.76 in Group 2 (Fig. 1). The duration from onset of symptoms to biopsy (months) and the time from initial therapy (years) were longer in Group 1 than in Group 2 (6.3 ± 9.7 vs. 2.3 ± 3.2; P < 0.01, 4.8 ± 2.6 vs. 3.1 ± 1.8; P < 0.01, respectively). There was no difference between groups in the number of HSPN patients by age at the onset and the number of HSPN patients newly diagnosed each month (Figs. 1, 2). The number of patients diagnosed with HSPN per 100,000 children (<15 years old) each year from 1987 to 2008 years is shown in Fig. 3. The mean number of patients per 100,000 children per year was 3.5 ± 1.2 in Group 1 and 3.6 ± 0.8 in Group 2, with no significant difference between groups.
Among the clinical manifestations at onset in all HSPN patients, the most common clinical symptoms were purpura (100%), abdominal pain (73%), arthralgia (34%), nephrotic syndrome (18%) and Quincke’s edema (9%), and again there were no significant differences in the clinical manifestations at onset between the two groups (Table 1).
On the basis of laboratory data at the onset, all patients had proteinuria and hematuria, and there were no differences in urinary protein excretion (g/day) or frequency of macrohematuria between the two groups (protein excretion: 1.81 ± 1.84 vs. 2.14 ± 2.10, frequency of macrohematuria: 17 vs. 32%,). Further, there were no differences in serum albumin levels or serum creatinine levels between the two groups (serum albumin levels: 3.7 ± 0.7 vs. 3.6 ± 0.7, serum creatinine levels: 0.44 ± 0.18 vs. 0.46 ± 0.16,).
Inter-group comparison of pathological findings at the time of the first renal biopsy
LM findings at the first renal biopsy in all HSPN patients: On the basis of LM findings, the most common ISKDC classification was IIIb (44%), grade III (25%), grade II (13%), grade IV (9%), grade V (5%) and grade VI (3%), and there were no differences in ISKDC classification or the rate of crescent formation between the two groups (Table 2).
Inter-group comparison of treatment and clinical stage at 2 years after treatment between groups
Eleven patients (18%) in Group 1 and 5 (9%) in Group 2 were treated with anti-platelet agents, 12 patients (20%) in Group 1 and 7 (12%) in Group 2 were treated with prednisolone, 31 patients (51%) in Group 1 and 20 (34%) in Group 2 were treated with MUP therapy, 7 patients (12%) in Group 1 and 27 (46%) in Group 2 were treated with MUP plus cyclophosphamide, and 3 patients (5%) in Group 1 and 8 (14%) in Group 2 were treated with MUP plus cyclophosphamide and PP. A greater proportion of patients from Group 2 than from Group 1 were treated with MUP plus cyclophosphamide therapy (46 vs. 12%, P < 0.05,).
As to the clinical outcome at 2 years after treatment, 44 (72%) patients in Group 1 and 47 (80%) patients in Group 2 had clinically recovered, 8 (13%) in Group 1 and 10 (17%) in Group 2 patients had minimal urinary abnormalities, 8 (13%) in Group 1 and 2 (3%) in Group 2 had active renal disease, and 1 (2%) in Group 1 and none in Group 2 had renal insufficiency.
Discussion
With regard to the incidence of HSP, Gardner-Medwin et al. [16] examined the frequency of and ethnic variation in childhood vasculitis in the West Midlands region of the United Kingdom. Their survey was completed using monthly questionnaires sent to consultants and a single questionnaire sent to family doctors along with a review of case notes with diagnostic codes for vasculitis. The annual incidence of HSP reported in the study was 22.1 per 100,000, which was higher than the previous estimates of 13.5–18.0 per 100,000 [16–18]. Gardner-Medwin et al. [16] postulated that a higher incidence of HSP may lead to increases in the incidence of renal disease and need for renal medical treatment.
On the other hand, in Japan, Moriya et al. [9] investigated 30 patients diagnosed with HSPN between 1971 and 1982 and 11 patients diagnosed with HSPN between 1985 and 1996 and found that the severity of the renal histopathological findings was lower in the 11 patients diagnosed with HSPN between 1985 and 1996. In our study, the mean number of HSPN patients per 100,000 children per year was 3.6 ± 1.0 and no differences in the mean number of HSPN patients per 100,000 children per year, clinical manifestations or laboratory findings at onset were observed between the two groups. In Asian children, it was reported that the mean number of HSPN patients per 100,000 children per year was 4.9 [16]. In Fukushima Prefecture, the figure was 3.6, which we think was low due to the criteria we employed to select HSPN patients for enrollment in our study. As to the pathological findings, there were no differences in ISKDC classification or the rate of crescentic formation between the two groups. Thus, the incidence of HSPN and the severity of HSPN were similar in patients treated between 1987 and 1997 and those treated between 1998 and 2008, with no observed decrease in the severity of HSPN in the Group 2 patients.
In view of the severity of HSPN, Soylemezoglu et al. evaluated 179 children with HSPN and found that 47.6% of all children had HSPN of higher than ISKDC grade III. In our results, 104 of the 120 patients (87%) had HSPN of higher than ISKDC grade IIIb [21].
As to the treatment for HSPN, in 1988, Niaudet et al. [5] reported that methylprednisolone pulse therapy was effective in patients at risk of progression of nephropathy, particularly if it was started early during the course of the disease before the crescents become fibrosed. We have used methylprednisolone and urokinase pulse therapy for patients with HSPN of higher than ISKDC grade IIIb from 1980 and previously reported the efficacy of the treatment on the basis of a controlled study to investigate the efficacy of that therapy combined with cyclophosphamide in patients with severe HSPN [13, 14]. In addition, Iijima et al. [19] also reported that a multiple combination therapy with prednisolone, cyclophosphamide, heparin or warfarin and dipyridamole could be effective in histologically severe cases of HSPN. In view of the treatment of rapidly progressive HSPN, Gianviti [20] showed that plasmapheresis associated with immunosuppressive treatment could be of benefit in cases of idiopathic RPGN or vasculitis. Hattori [15] reported that plasmapheresis as the sole therapy effective in improving the prognosis of patients with rapidly progressive HSPN. Thus, there have been many reports on the efficacy of treatments for HSPN. However, all of the reports were retrospective studies. In a review of these reports, Zaffanello et al. stated that the treatment of HSPN has not been adequately guided by evidence obtained in properly designed, randomized, placebo-controlled trials with outcome markers related to the progression to end stage renal disease and suggested that multicenter and randomized control studies should be undertaken in order to obtain results with good statistical power [22].
As to the clinical stage at 2 years after treatment, 13% of patients in Group 1 and 3% in Group 2 had active renal disease, and 2% in Group 1 and none patients in Group 2 had renal insufficiency. The outcome at 2 years after treatment was good in both groups, and no significant inter-group differences were observed.
In conclusion, our findings suggest that the incidence of HSPN and the severity of HSPN were similar in patients diagnosed between 1987 and 1997 and those diagnosed between 1998 and 2008, with no observable decrease in the severity of HSPN. However, it is difficult at this time to emphatically state that the incidence of patients with severe HSPN has not decreased on the basis of a retrospective study conducted at just one institution. It will, of course, be necessary to further evaluate the changes in the incidence of HSPN and severity of HSPN through prospective studies at a larger number of institutions.
References
Habib R, Niaudet R, Levy M (1994) Schönlein-Henoch purpura nephritis and IgA nephropathy. Renal pathology with clinical and functional correlations, 2nd edn. Lippincott, Philadelphia, Tisher CC, Brenner BM; pp 427–523
Trapani S, Micheli A, Grisolia F et al (2005) Henoch-Schönlein purpura in childhood: epidemiological and clinical analysis of 150 cases over a 5-year period and review of literature. Semin Arthritis Rheum 35:143–153
Fretzayas A, Sionti I, Moustaki M et al (2008) Henoch-Schönlein purpura: a long-term prospective study in Greek children. J Clin Rheumatol 14:324–331
Haycock GB (1998) The nephritis of Henoch-Schönlein purpura. Oxford Textbook of Nephrology, 2nd edn. Oxford University Press, Oxford, Cameron JS pp 585–612
Niaudet P, Habib R (1998) Methylprednisolone pulse therapy in the treatment of severe forms of Schönlein-Henoch purpura nephritis. Pediatr Nephrol 12:238–243
Watanabe T, Takahashi S, Nakajo S et al (1996) Pathological improvement of IgA nephropathy and Henoch-Schönlein purpura nephritis with urokinase therapy. Acta Paediatr Jpn 38:622–628
Coppo R, Mazzucco G, Cagnoli L et al (1997) Henoch-Schönlein purpura Long-term prognosis of Henoch-Schönlein nephritis in adults and children. Nephrol Dial Transplant 12:2277–2283
Counahan R, Winterborn MH, White RHR et al (1977) Prognosis of Henoch-Schönlein nephritis in children. Br Med J 2:11–14
Moriya S, Iitaka K, Koshino H et al (2000) Henoch-Schönlein purpura nephritis (HSPN) in children: comparison of the incidence and severity between two 12-year groups. Nippon Jinzo Gakkai Shi 42:36–40
Southwest Pediatric Nephrology Study Group (1985) A clinico-pathologic study of crescentic glomerulonephritis in 50 children: a report of the Southwest Pediatric Nephrology Study Group. Kidney Int 27:450–458
National Heart, Lung and Blood Institute, Bethesda, Maryland (1987) Report of the second task force on blood pressure control in children. Pediatrics 79:1–25
White RHR (1994) Henoch-Schönlein nephritis. A disease with significant late sequelae. Nephron 68:1–9
Kawasaki Y, Suzuki J, Nozawa R et al (2003) Efficacy of methylprednisolone and urokinase pulse therapy for severe Henoch-Schönlein nephritis. Pediatrics 111:785–789
Kawasaki Y, Suzuki J, Suzuki H (2004) Efficacy of methylprednisolone and urokinase pulse therapy combined with or without cyclophosphamide in severe Henoch-Schönlein: a clinical and histopathological study. Nephrol Dial Transplant 19:858–864
Hattori M, Ito K, Konomoto T et al (1999) Plasmapheresis as the sole therapy for rapidly progressive Henoch-Schönlein Purpura nephritis in children. Am J Kidney Dis 33:427–433
Gardner-Medwin JMM, Dolezalova P, Cummins C et al (2002) Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet 360:1197–1202
Stewan M, Savage JM, Bell B et al (1988) Long term renal prognosis of Henoch-Schönlein purpura in unselected childhood population. Eur J Pediatr 147:113–115
Nielsen HE (1988) Epidemiology of Schönlein-Henoch Purpura. Acu Pathol Scand 77:125–131
Iijima K, Ito-Kariya S, Nakamura H et al (1988) Multiple combined therapy for severe Henoch-Schönlein nephritis in children. Pediatr Nephrol 12:244–248
Gianviti A, Trompeter RS, Barratt TM et al (1996) Retrospective study of plasma exchange in patients with idiopathic rapidly progressive glomerulonephritis and vasculitis. Arch Dis Child 75:186–190
Zaffanello M, Fanos V (2009) Treatment-based literature of Henoch-Schönlein purpura nephritis in childhood. Pediatr Nephrol 24:1901–1911
Soylemezoglu O, Ozkaya O, Ozen S, Bakkaloglu A, Dusunsel R, Peru H, Cetinyurek A, Yidiz N, Donmez O, Buyan N, Mir S, Arisoy N, Gur-Guven A, Alpay H, Ekim M, Aksu N, Soylu A, Gok F, Poyrazoglu H, Sonmez F, Turkish Pediatric Vasculitis Study Group (2009) Henoch- Schönlein nephritis: a nationwide study. Nephron Clin Pract 112:c199–c204
Acknowledgments
The authors thank the members of the Department of Pediatrics for their valuable advice and comments in relation to this study. None of the authors have financial relationships with any companies with an interest in the subject matter of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawasaki, Y., Suyama, K., Yugeta, E. et al. The incidence and severity of Henoch-Schönlein purpura nephritis over a 22-year period in Fukushima Prefecture, Japan. Int Urol Nephrol 42, 1023–1029 (2010). https://doi.org/10.1007/s11255-009-9701-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-009-9701-3