Abstract
Purpose
Hepatitis C virus (HCV) infection impairs quality of life (QOL) in patients who are not on dialysis therapy. In dialysis patients, how HCV infection affects QOL is unknown. In our study, we investigated the independent relationship between HCV infection and QOL.
Methods
Sociodemographic and laboratory variables were recorded. Severity of depressive symptoms and QOL were assessed by Beck Depression Inventory (BDI) and Short Form-36 (SF-36), respectively.
Results
Among 165 patients, 83 were anti-HCV antibody positive and 82 were anti-HCV antibody negative. Anti-HCV antibody positive patients had higher BDI scores than anti-HCV antibody negative patients (P = 0.011). Other than the social functioning subscale, all SF-36 subscales were lower in anti-HCV antibody positive patients when compared with anti-HCV negative patients. Anti-HCV antibody positive patients had lower physical (P = 0.003) and mental component summary scores (P = 0.018) than negative patients. Physical component summary score was independently associated with hemodialysis duration (P = 0.003), sleep disturbance (P = 0.046), BDI score (P = 0.027), albumin (P = 0.002), and serum hemoglobin (P < 0.0001). Physical component summary score was not associated with anti-HCV antibody positivity. Mental component summary score was independently associated with BDI score (P = 0.001), anti-HCV antibody positivity (P = 0.016), and serum hemoglobin (P < 0.0001).
Conclusion
HCV infection impairs QOL, especially in mental aspects, in hemodialysis patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although there have been many advances in the treatment of end-stage renal disease (ESRD), mortality rates for ESRD patients remain several times higher than those of age-matched controls, and patients with ESRD continue to have significant impairments in quality of life (QOL) [1]. Quality of life is related with morbidity and mortality in hemodialysis (HD) patients [2], and it is suggested that QOL should be considered in the regular monitoring of dialysis patients [3].
Chronic hepatitis C virus (HCV) infection is another serious health problem which affects QOL. Studies conducted in patients, without paying attention to renal function, demonstrated that patients with chronic HCV infection score worse than matched controls on various QOL indices [4]. Given the disconnection between the growing importance of measuring QOL in HCV-infected patients and the inability of many clinicians to readily interpret QOL differences, it is imperative to establish the clinical significance of QOL score differences by anchoring them to changes in clinically familiar outcomes [5]. As previously demonstrated, HCV infection and comorbid psychiatric illnesses have relative impacts on QOL. However, much less is known about the effect of comorbid medical illness on QOL in patients with chronic HCV infection. Co-occurring conditions adversely affect QOL and mortality, the degree of impairment of QOL being associated with the number of medical comorbid illnesses [6]. By knowing the clinically important differences in QOL, researchers, physicians, and patients can better understand not only the overall health burden of HCV infection, but also the optimal approach [5]. There is an increasing need to study the interaction of multiple diseases with QOL, and in this regard HCV-infected hemodialysis patients constitute a very specific subset of patients with decreased QOL and increased prevalence of comorbidities, morbidity, and mortality. The factors that influence QOL in patients with ESRD are not fully known. Previous researches have focused on the effects of erythropoietin and exercise, and on the impact of the various modalities of renal replacement therapy on QOL [1]. However, the effect of chronic HCV infection, which is common in HD patients, on QOL is not specifically studied. Here in this study, we aimed to analyze the impact of chronic HCV infection on QOL and to compare the QOL of HCV-infected and noninfected HD patients via Short Form (SF)-36.
Methods
The subjects for our cross-sectional investigation were HD patients attending the HD unit in Baskent University Hospital in Ankara. The study received local ethical approval and was in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients before enrolment.
The dialysis prescription in our study included 4–5 h of HD, thrice weekly for all patients with flow rates of 300–400 ml/min, using standard bicarbonate dialysis solution (sodium 138 mmol/l, bicarbonate 35 mmol/l, potassium 1.5 mmol/l, calcium 1.25 mmol/l, and magnesium 1.8 mmol/l) by 1.1–1.7 m2 hollow-fiber dialyzer. All patients were virtually anuric and clinically euvolemic. Patients were divided into two groups according to status of anti-HCV antibody (anti-HCV antibody positive patients versus anti-HCV antibody negative patients). Urea kinetic modeling was performed in order to assess the delivered equilibrated dose of dialysis. Hemodialysis dose was evaluated using the following formula:
where spKt/V is a single-pool Kt/V, R is the ratio of post dialysis to predialysis serum urea nitrogen, t is time on dialysis in hours, UF is the amount of ultrafiltration in liters, and W is postdialysis body weight in kilograms.
Patients with an ischemic leg ulcer, or who had peripheral revascularization procedures within last 6 months or amputation for critical limb ischemia were excluded. Patients who had received interferon treatment in last 3 months were also excluded. Patients who had suffered from acute coronary syndrome, myocardial infarction, angina pectoris or coronary revascularization procedure (coronary stent replacement and coronary artery bypass graft surgery) within last 6 months were not included. Coronary artery disease was defined as presence of previous myocardial infarction, angina pectoris or coronary revascularization procedure.
We recorded the sociodemographic and clinical characteristics of the patients including age, gender, life status (living alone or with partner), education status (illiterate, elementary school, secondary school, high school, university graduate), marital status (married, not married, divorced), economical status (monthly money income satisfactory or unsatisfactory), sleep disturbance (present or absent), previous renal transplantation (present or absent), history of interferon treatment (present or absent), presence of coronary artery disease (yes or no), vascular access type (fistula, graft or catheter), alcohol abuse (present or absent). None of the patients was taking antidepressants and none of them had alcohol abuse. None of the patients were coinfected with hepatitis B virus. Body mass index (BMI) was calculated as the ratio of dry weight in kilograms (end-dialysis weight) to height squared (in square meters).
The laboratory parameters including serum hemoglobin, albumin, C-reactive protein (CRP), predialysis blood urea nitrogen and creatinine, predialysis calcium and phosphorus, alkaline phosphatase (ALP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), serum iron, total iron binding capacity (TIBC), ferritin, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, triglyceride, and intact parathyroid hormone (iPTH) were measured before the beginning of HD session. Postdialysis serum urea nitrogen levels, used to calculate urea reduction ratio, were also measured.
Serum anti-HCV antibody was measured by the peptide synthesized microparticle enzyme immunoassay (MEIA-III, AxSYM HCV version 3.0, Abbott Laboratories, Paul-Ehrlich-Institut, Langen, Germany). Serum HCV-RNA level was determined by quantitative assay (AcuGen RT-Amplisensor, Biotronics Tech Corp, Lowell, MA, USA), using a standardized technique based on reverse-transcriptase polymerase chain reaction.
After being given a brief explanation, Beck Depression Inventory (BDI) and QOL assessment using SF-36 were performed for each patient during regularly scheduled dialysis treatments. Assistance was available for patients who were illiterate.
Beck Depression Inventory
The BDI, which was originally introduced by Beck et al., is a 21-item self-reported inventory that measures characteristic attitudes and symptoms of depression [7]. The 21 items are answered on a four-point Likert scale, on which 0 represents absence of a problem and 3 represents extreme severity of a problem. The total score ranges from 0 to 63. For example, the score for feeling sad ranges from zero (“I don’t feel sad.”) to 3 (“I am so unhappy that I cannot stand it.”). Examples of other cognitive feelings surveyed are guilt, disappointment, failure, and decision making. The somatic items of the BDI are used to assess issues such as fatigue and sleep function. For example, the score for fatigue ranges from zero (“I do not get more tired than usual.”) to 3 (“I am too tired to do anything.”). The BDI is documented as a valid index of depression and BDI scores correlate well with the diagnostic criteria for depression. The advantage of the BDI is that it places the subject within a range of depression severity, rather than merely identifying whether the person meets certain diagnostic criteria [8]. It has been used frequently to measure severity of depressive symptoms in HD patients and is a useful screen for managing clinical depression in this patient group [9]. Savasir and Sahin demonstrated the validity of the BDI in the Turkish population [10].
Quality-of-life assessment
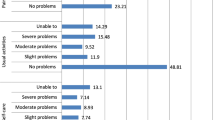
In order to evaluate the QOL of the patients, a short form of medical outcomes study (SF-36) was used [11], which was adapted to Turkish population [12]. The test consists of 36 items, which are assigned to eight subscales, namely physical functioning, role-physical limitation (i.e., role limitations caused by physical problems), bodily pain, general health perception, vitality, social functioning, role emotional (i.e., role limitations caused by emotional problems), and mental health. Each subscale is scored with a range from 0 to 100. The higher the score, the better the QOL. Pain subscale is scored so that a high score indicates freedom from pain. These eight subscales can be summarized by a physical component summary score (PCS) and mental component summary score (MCS). SF-36 has been commonly used and validated in patients with ESRD [13]. SF-36 was also used widely in HCV-infected patients and impact of HCV infection on QOL measured by SF-36 was recently systematically reviewed [14].
Statistical analysis
All values are expressed as mean ± standard deviation, median, and as a percentage (%). Nonnormally distributed variables are reported as medians with 25th and 75th percentiles in parentheses. Data were analyzed using the SPSS 11.0 program (SPSS Inc., Chicago, IL, USA) for Windows. Normality of the data was evaluated by Kolmogorov-Smirnov test with Shapiro-Wilk correction. Parameter differences between two groups were evaluated using the Mann-Whitney U-test for nonnormally distributed variables and Student t-test for normally distributed variables. P value <0.05 was accepted as statistically significant. For the comparison of categorical variables, chi-square test was used. Univariate associations between PCS and MCS with clinical and demographic parameters (as independent variables) including age, gender, HD duration, anti-HCV antibody status, presence of diabetes mellitus and coronary artery disease, marital status, history of previous renal transplantation, sleep disturbance, education status, BDI score, hemoglobin, albumin, and CRP were assessed using univariate linear regression. Then, we performed multivariate linear regression analysis to determine the factors related to PCS and MCS, respectively. All variables with P value <0.05 in the univariate analysis were included in the multivariate linear regression model. Stepwise procedure was selected for multivariate analysis. Absence of collinearity among explanatory factors was checked in all models based on standard procedures.
Results
Initially, 188 patients were recruited. Nine anti-HCV antibody positive and four anti-HCV antibody negative patients refused to answer the BDI and SF-36 questionnaires. Three patients with ischemic leg ulcer and who had peripheral revascularization procedures within last 6 months or amputation for critical limb ischemia were excluded. Although patients who had previously received interferon treatment were included, two patients who received interferon treatment within last 3 months were excluded. Five patients who had suffered from acute coronary syndrome, myocardial infarction, angina pectoris or coronary revascularization procedure within last 6 months were excluded. The study was conducted on the remaining 165 HD patients.
Among these 165 patients, 83 were anti-HCV antibody positive and 82 were anti-HCV antibody negative. The comparative sociodemographic characteristics and laboratory parameters of anti-HCV antibody positive and anti-HCV antibody negative HD patients are given in Table 1 and Table 2, respectively. Vascular access for HD was an arteriovenous fistula in 137 patients, a vascular graft in 18 patients, and a permanent intravenous catheter in 10 patients. Etiologies for ESRD were as follows: glomerulonephritis in 29, diabetes mellitus in 25, hypertension in 25, vesicourethral reflux and pyelonephritis in 21, nephrolithiasis in 16, polycystic kidney disease in 10, amyloidosis in 11, contrast nephropathy in 2 patients, Alport syndrome in 1, and systemic lupus erythematosus in 1 patient, respectively. The etiology for ESRD was unknown in 24 patients. Among anti-HCV antibody positive patients, 49 (59%) had HCV-RNA positivity and 34 (40.9%) had previously received interferon treatment. Table 3 presents the comparative BDI and SF-36 scores of anti-HCV antibody positive and negative HD patients.
In multiple linear regression analysis, anti-HCV positivity was an independent predictor of the following SF-36 subscales: physical functioning (B = 9.727, beta = 0.178, 95% confidence interval = 0.625–18.830, P = 0.036), general health perception (B = 7.847, beta = 0.215, 95% confidence interval = 1.567–14.127, P = 0.015), vitality (B = 10.327, beta = 0.250, 95% confidence interval = 3.574–17.079, P = 0.003), and mental health (B = 6.910, beta = 0.195, 95% confidence interval = 1.200–12.620, P = 0.018). Other subscales were not independently associated with anti-HCV positivity.
In univariate regression analysis, PCS was independently associated with age (P = 0.011), gender (P = 0.002), HD duration (P < 0.0001), anti-HCV positivity (P = 0.003), sleep disturbance (P = 0.009), BDI score (P = 0.001), hemoglobin (P < 0.0001), albumin (P < 0.0001), and CRP (P = 0.046). To determine the independent variables which are related to PCS (as a dependent variable), these independently associated variables in univariate analysis were selected for multivariate linear stepwise analysis (Table 4).
In univariate regression analysis, MCS was associated with anti-HCV antibody positivity (P = 0.018), hemoglobin (P < 0.0001), and BDI score (P < 0.0001). To determine the independent variables which are related to MCS (as a dependent variable), these independently associated variables in univariate analysis were selected for multivariate linear stepwise analysis (Table 4). When considering only anti-HCV antibody positive patients, presence of HCV-RNA was related neither with PCS (P = 0.660) nor with MCS (P = 0.245) in regression models.
Discussion
In the current study, we demonstrated that the majority of the SF-36 subscales were lower in anti-HCV antibody positive HD patients compared with in anti-HCV antibody negative patients. To our knowledge, we are the first to find an independent association between anti-HCV antibody positivity and MCS of SF-36, but not with PCS. Hence, it is likely that patient-reported perception of mental state, no matter how subjective it sounds, is more closely related with anti-HCV antibody positivity than is their perception of physical state.
We do not know the exact mechanisms regarding the relationship between anti-HCV antibody positivity and low MCS found in our study. However, presence of depressive symptoms might be one of the explanations. The published literature and routine clinical practice inform us that depression is a common finding in HCV-infected patients. The relationship between HCV infection and depression is complex. Patients with depression may have a higher incidence of HCV infection. Conversely, depression may exist as a secondary phenomenon to HCV infection. This may take the form of a reactive depression related to the diagnosis and concerns over long-term health or may be secondary to symptoms such as fatigue and cognitive impairment [15]. Previously, it was shown that HD patients with depression scored lower on all eight of the SF-36 subscales [16] and the severity of depression correlated with QOL parameters [17]. In our study, we found that depression scores of HCV-infected HD patients were higher than HCV noninfected patients.
Another possible factor for the increased cognitive impairment in HCV-infected HD patients might be coexistent minimal encephalopathy. It is well established that cognitive impairment is frequently detectable in patients with cirrhosis, even in the absence of clinical encephalopathy, and is termed “minimal encephalopathy” [18]. The effect of HCV infection on cognitive capability may in part explain the high prevalence of depression, which in turn may result in decreased MCS in HCV-infected HD patients.
We found no relationship between liver enzymes and QOL. As an interesting finding, regarding anti-HCV antibody positive patients, HCV-RNA did not associate with either PCS or MCS. Given that presence of anti-HCV antibody is not equivalent to active hepatitis C infection, our findings need to be discussed further. Previous studies conducted in non-HD patients with chronic HCV infection have shown that there was no consistent relationship between QOL and liver disease parameters including HCV-RNA, serum ALT levels, and liver histology [19–23]. Mechanisms regarding these findings are not known. However, one postulated hypothesis was the “labeling effect.” It was previously pointed out that the reduction in QOL may not be caused by biological consequences of HCV infection. Chronic HCV infection may impair QOL simply because of the effects of labeling, which refers to the impact on QOL of the consequences of establishing the diagnosis. Thus, worse QOL in HCV-infected patients may partly be attributable to the impact of the diagnostic process per se [24, 25]. We found that PCS was positively and independently associated with hemoglobin and albumin and negatively and independently associated with HD duration, sleep disturbance, and BDI scores. Our findings were in accordance with the previous findings in the literature [26–30]. Mental component summary score was positively correlated with hemoglobin and negatively correlated with BDI scores. Kalantar-Zadeh et al. also found significant positive correlations between PCS, MCS, hemoglobin, and albumin in HD patients. However, comparative analysis of QOL regarding the status of anti-HCV antibody was lacking in their study [31]. Our results demonstrated that QOL was not related with dialysis adequacy, as measured by spKt/V. These findings are in accordance with the previous findings [27, 31–34].
Since, as far as we know, our study is the first in the literature, we cannot exactly know the clinical significance of our findings at the present time. Mapes et al. demonstrated that both PCS and MCS are independently associated with higher risk of death and hospitalization in HD patients, independent of a series of demographic and comorbid factors [35]. It is hypothesized that HCV infection is related with higher mortality in HD patients [36]. Thus, we can speculate that one of the mechanisms of increased mortality by HCV infection might be due to impaired QOL observed in these patients. This finding may be important for some reasons. First of all, treatment of HCV infection in HD patients may decrease mortality by improving QOL, independent of other factors (e.g., liver disease). Some HD patients with advanced liver disease may still benefit from therapy, especially in terms of QOL and therefore decreased mortality. Secondly, factors affecting QOL in HD patients are not exactly known and HCV infection might be accepted as a novel factor for worse QOL, especially in mental aspects. Thirdly, our findings could be accepted as an indirect clue, as other clues, that HCV infection might be responsible for the minimal encephalopathy (firstly described in patients with normal renal function) in HD patients [18, 37].
We have limitations that deserve mention. First of all, HD patients invited to this study were from a single center and may not be representative of all HD patients. Additionally, it was not possible to accurately measure all the variables that might have impact on HRQOL. Finally, since our study had a cross-sectional design, our findings do not prove a cause–effect relationship.
In conclusion, HCV infection impairs QOL, especially in mental aspects, in HD patients. Dialysis staff must bear in mind that HCV infection, by impairing QOL, may result in increased morbidity and mortality in HD patients.
References
Manns BJ, Johnson JA, Taub K et al (2002) Dialysis adequacy and health related quality of life in hemodialysis patients. ASAIO J 48:565–569. doi:10.1097/00002480-200209000-00021
DeOreo PB (1997) Hemodialysis patient-assessed functional health status predicts continued survival, hospitalization, and dialysis-attendance compliance. Am J Kidney Dis 30:204–212. doi:10.1016/S0272-6386(97)90053-6
Merkus MP, Jager KJ, Dekker FW et al (1999) Physical symptoms and quality of life in patients on chronic dialysis: results of The Netherlands cooperative study on adequacy of dialysis (NECOSAD). Nephrol Dial Transplant 14:1163–1170. doi:10.1093/ndt/14.5.1163
McHutchison JG, Ware JE Jr, Bayliss MS et al (2001) Hepatitis interventional therapy group the effects of interferon alpha-2b in combination with ribavirin on health related quality of life and work productivity. J Hepatol 34:140–147. doi:10.1016/S0168-8278(00)00026-X
Spiegel BMR, Younossi ZM, Hays RD et al (2005) Impact of hepatitis C on health related quality of life: a systematic review and quantitative assessment. Hepatology 41:790–800. doi:10.1002/hep.20659
Kwan JW, Cronkite RC, Yiu A et al (2008) The impact of chronic hepatitis C and co-morbid illnesses on health-related quality of life. Qual Life Res 17:715–724. doi:10.1007/s11136-008-9344-3
Beck AT, Ward CH, Mendelson M et al (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Micozkadioglu H, Micozkadioglu I, Zumrutdal A et al (2006) Relationship between depressive affect and malnutrition-inflammation complex syndrome in haemodialysis patients. Nephrology (Carlton) 11:502–505
Koo JR, Yoon JW, Kim SG et al (2003) Association of depression with malnutrition in chronic hemodialysis patients. Am J Kidney Dis 41:1037–1042. doi:10.1016/S0272-6386(03)00201-4
Savasir I, Sahin NH (1997) Assessment in cognitive behavioral therapy: frequently used scales. Turkish Society of Psychologists, Ankara
Ware JE Jr, Sherbourne CD (1984) Physicians’ attitudes in counseling patients about smoking. Med Care 22:360–365. doi:10.1097/00005650-198404000-00007
Koçyigit H, Aydemir Ö, Fişek G et al (1999) Kısa form 36 (kf-36)’nın Türkçe versiyonunun güvenilirliği ve geçerliligi. İlaç ve tedavi dergisi 12:102–106
Johansen KL, Painter P, Kent-Braun JA et al (2001) Validation of questionnaires to estimate physical activity and functioning in end-stage renal disease. Kidney Int 59:1121–1127. doi:10.1046/j.1523-1755.2001.0590031121.x
Spiegel BM, Younossi ZM, Hays RD et al (2005) Impact of hepatitis C on health related quality of life: a systematic review and quantitative assessment. Hepatology 41:790–800. doi:10.1002/hep.20659
Forton DM, Taylor-Robinson SD, Thomas HC (2003) Cerebral dysfunction in chronic hepatitis C infection. J Viral Hepat 10:81–86. doi:10.1046/j.1365-2893.2003.00416.x
Walters BA, Hays RD, Spritzer KL et al (2002) Health-related quality of life, depressive symptoms, anemia, and malnutrition at hemodialysis initiation. Am J Kidney Dis 40:1185–1194. doi:10.1053/ajkd.2002.36879
Turk S, Atalay H, Altintepe L et al (2006) Treatment with antidepressive drugs improved quality of life in chronic hemodialysis patients. Clin Nephrol 65:113–118
Ferenci P, Lockwood A, Mullen K et al (2002) Hepatic encephalopathy–definition, nomenclature, diagnosis, and quantification: final report of the working party at the 11th World Congresses of Gastroenterology, Vienna, 1998. Hepatology 35:716–721. doi:10.1053/jhep.2002.31250
Davis GL, Balart LA, Schiff ER et al (1994) Assessing health-related quality of life in chronic hepatitis C using the sickness impact profile. Clin Ther 16:334–343
Carithers RL Jr, Sugano D, Bayliss M (1996) Health assessment for chronic HCV infection: results of quality of life. Dig Dis Sci 41:75S–80S. doi:10.1007/BF02087879
Foster GR, Goldin RD, Thomas HC (1998) Chronic hepatitis C virus infection causes a significant reduction in quality of life in the absence of cirrhosis. Hepatology 27:209–212. doi:10.1002/hep.510270132
Bayliss MS, Gandek B, Bungay KM et al (1998) A questionnaire to assess the generic and disease-specific health outcomes of patients with chronic hepatitis C. Qual Life Res 7:39–55. doi:10.1023/A:1008884805251
Fontana RJ, Moyer CA, Sonnad S et al (2001) Comorbidities and quality of life in patients with interferon-refractory chronic hepatitis C. Am J Gastroenterol 96:170–178. doi:10.1111/j.1572-0241.2001.03473.x
Rodger AJ, Jolley D, Thompson SC et al (1999) The impact of diagnosis of hepatitis C virus on quality of life. Hepatology 30:1299–1301
Córdoba J, Reyes J, Esteban JI et al (2003) Labeling may be an important cause of reduced quality of life in chronic hepatitis C. Am J Gastroenterol 98:226–227
Kutner NG, Zhang R, Huang Y et al (2008) Patient-reported sleep difficulty and cognitive function during the first year of dialysis. Int Urol Nephrol 40:203–210. doi:10.1007/s11255-007-9188-8
Iliescu EA, Coo H, McMurray MH et al (2003) Quality of sleep and health-related quality of life in haemodialysis patients. Nephrol Dial Transplant 18:126–132. doi:10.1093/ndt/18.1.126
Elder SJ, Pisoni RL, Akizawa T et al (2008) Sleep quality predicts quality of life and mortality risk in haemodialysis patients: results from the dialysis outcomes and practice patterns study (DOPPS). Nephrol Dial Transplant 23:998–1004. doi:10.1093/ndt/gfm630
Acaray A, Pinar R (2005) Quality of life in Turkish haemodialysis patients. Int Urol Nephrol 37:595–602. doi:10.1007/s11255-005-0397-8
Vasilieva IA (2006) Quality of life in chronic hemodialysis patients in Russia. Hemodial Int 10:274–278
Kalantar-Zadeh K, Kopple JD, Block G et al (2001) Association among SF-36 quality of life measures and nutrition, hospitalization, and mortality in hemodialysis. J Am Soc Nephrol 12:2797–2806
Morton AR, Meers C, Singer MA et al (1996) Quantity of dialysis: quality of life–what is the relationship? ASAIO J 42:M713–M717
Unruh M, Benz R, Greene T et al (2004) Effects of hemodialysis dose and membrane flux on health-related quality of life in the HEMO study. Kidney Int 66:355–366. doi:10.1111/j.1523-1755.2004.00738.x
Merkus MP, Jager KJ, Dekker FW et al (1997) Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. The Necosad study group. Am J Kidney Dis 29:584–592. doi:10.1016/S0272-6386(97)90342-5
Mapes DL, Lopes AA, Satayathum S et al (2003) Health-related quality of life as a predictor of mortality and hospitalization: the dialysis outcomes and practice patterns study (DOPPS). Kidney Int 64:339–349. doi:10.1046/j.1523-1755.2003.00072.x
Fabrizi F, Martin P, Dixit V et al (2004) Meta-analysis: effect of hepatitis C virus infection on mortality in dialysis. Aliment Pharmacol Ther 20:1271–1277. doi:10.1111/j.1365-2036.2004.02290.x
Thomas HC, Török ME, Forton DM et al (1999) Possible mechanisms of action and reasons for failure of antiviral therapy in chronic hepatitis C. J Hepatol 31(Suppl 1):152–159. doi:10.1016/S0168-8278(99)80393-6
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Afsar, B., Elsurer, R., Sezer, S. et al. Quality of life in hemodialysis patients: hepatitis C virus infection makes sense. Int Urol Nephrol 41, 1011–1019 (2009). https://doi.org/10.1007/s11255-009-9576-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-009-9576-3