Abstract
Background
Contrast-induced nephropathy (CIN) is a common cause of acute kidney injury. Several preventive therapies for this injury have been tested; however, there is still no consensus on the optimal protocol.
Methods
We performed a systematic search of the National Library of Medicine and the Cochrane Library databases from January 1985 to November 2008 to identify randomized controlled studies examining sodium bicarbonate as a preventive measure for CIN in humans. We also reviewed conference abstracts from cardiology nephrology and radiology meetings from 2004 to 2008. A change in serum creatinine levels defined by an absolute (≥0.5 mg/dl) or percentage (≥25%) increase in the serum creatinine level is defined as CIN. The primary outcome measure was the incidence of CIN, and the secondary outcome measures were: change in serum creatinine from baseline, requirement for renal replacement therapy and death.
Results
Seventeen randomized controlled trials have investigated the role of sodium bicarbonate for prophylaxis of CIN. The overall incidence of CIN was 11.3%. Using the results from all 17 studies that compared bicarbonate versus saline, the pooled relative risk of developing CIN was 0.54 (95% CI, 0.36–0.83) in the intervention arm, indicating a significant benefit from sodium bicarbonate. The pooled relative risk of CIN was 0.57 (95% CI, 0.35–0.95) when we analyzed for the studies that compared the effects sodium bicarbonate to NAC on development of CIN. There was no difference in the rates of requirement for renal replacement therapy and death.
Conclusions
The use of sodium bicarbonate appears to reduce the incidence of CIN when compared to other preventive strategies for CIN without a significant difference in the requirement of renal replacement therapy and mortality. There are study heterogeneity and publication biases. Further adequately powered randomized controlled studies are needed to determine whether sodium bicarbonate will reduce the clinically meaningful outcomes (e.g., need for dialysis or death) and optimal hydration strategy in high-risk patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute kidney injury (AKI) has life-threatening consequences, and iodine contrast media is one of the most important factors that precipitates acquired AKI in hospitalized patients [1–3]. The rising incidence of contrast-induced nephropathy (CIN) over the last decades is related to an increasing number of invasive diagnostic procedures requiring radiographic contrast, which are frequently performed in an ever more susceptible, high-risk population. Primarily, several different risk factors for CIN have been documented, including impaired kidney function [4], diabetes [5], age and conditions that impair renal blood flow, such as hypotension or nonsteroidal anti-inflammatory drugs [6]. It has been well established that patients who develop CIN have an increased risk of morbidity, prolonged hospitalization and mortality [7–11]. Due to these increased risks, efforts to prevent or ameliorate CIN are warranted, but the best available strategy to minimize these important risks still needs to be exactly defined [2, 3].
Although the pathophysiological processes of CIN are not completely understood, many potential mechanisms for renal injury have been proposed, including contrast-media-induced vasoconstriction resulting in reduction in renal blood flow, direct tubular toxicity, and free radical and oxidative injury to tubular cells [12, 13]. Based on these mechanisms, several preventive therapies for CIN have been tested in patients receiving iodinated contrast media. There are encouraging results in the prevention of CIN with isotonic saline, theophylline, N-acetylcysteine, low and iso-osmolar contrast [14–17]. A very recent meta-analysis including 41 studies by Kelly et al. [18] about the effectiveness of drugs (including dopamine, fenoldopam, furosemide, N-acetylcysteine and theophylline) for prevention of CIN showed that (1) N-acetylcysteine is more protective than hydration alone, (2) theophylline may also reduce the risk for development of CIN, but its association with better outcomes did not reach significance, (3) furosemide increases the risk for development of CIN and (4) dopamine and fenoldopam did not affect the risk of CIN.
However, all of these previous strategies to prevent CIN are often insufficient, and there is still no certainty about the optimal protocol. Sodium bicarbonate has recently been the focus of various reports, both prospective and retrospective analyses with large databases [19–36]. Results from two retrospective studies, the Mayo clinic cohort study [37] and the study by Schmidt et al. [38], suggest that sodium bicarbonate is associated with increased incidence of CIN, in contrast to several prospective randomized but smaller size studies. Moreover, two recent meta-analyses found that sodium bicarbonate hydration significantly decreases the incidence of CIN compared to normal saline [39, 40]. However, two recently published randomized controlled trials (RCT) and abstracts do not suggest that hydration with sodium bicarbonate is superior to hydration with normal saline for prevention of the development of CIN [33, 34]. Therefore, it is time to systematically review the available evidence and investigate the results from pooling RCTs. In this report, we performed a meta-analysis to assess the overall effect of sodium bicarbonate in preventing CIN using all available data.
Methods
Literature review
A systematic computer-aided search of the National Library of Medicine, EMBASE, and the Cochrane Library was performed for all pertinent studies examining sodium bicarbonate as a preventive measure for CIN in humans published between 1985 and November 2008 without language restriction. Key words used included ‘contrast media or contrast or radiocontrast,’ ‘nephropathy or contrast nephropathy,’ ‘kidney failure or acute renal failure or acute kidney injury’ and ‘sodium bicarbonate.’ In addition, we identified other potentially relevant studies using a manual search of references from all eligible studies, review articles and Science Citation Index Expanded on the Web of Science, and searched the top 50 citations for each paper through the “related articles” feature of PubMed. Furthermore, we also reviewed conference proceedings of the American Society of Nephrology, International Society of Nephrology, American College of Cardiology, American Heart Association, American Society of Anesthesiologists and American College of Clinical Pharmacists. The two reviewers worked independently (M.K., F.T.), and disagreements were resolved by consensus.
Data extraction
We independently extracted data from all primary studies fulfilling eligibility criteria. Inclusion criteria were as follows: (1) study design (randomized controlled trials), (2) target population (patients receiving contrast media for angiography or computed tomography), (3) intervention (trials of sodium bicarbonate versus control) and (4) outcome (trials with explicit definition of CIN). Data extracted included identifying information, focus of the study, details of the study protocol and demographic data. The primary outcome measure was the incidence of CIN. The secondary outcome measures were: change in serum creatinine from baseline, requirement for renal replacement therapy and mortality.
Statistical methods
We assessed the risk of CIN observed with the administration of sodium bicarbonate versus control therapies in 2 × 2 contingency tables. Initially, the results were pooled using fixed effects (Mantel–Haenzel) methods. Between study heterogeneity was determined by the Q statistic, with a P value < 0.1 considered statistically significant. The I 2 statistic was used to quantify the magnitude of heterogeneity, with values of 0 to 30%, 31 to 50% and greater than 50% representing mild, moderate and notable heterogeneity, respectively. Because statistical heterogeneity was present, the overall results were mathematically pooled using techniques that accounted for within and between study heterogeneity (random effects method of DerSimonian and Laird). All statistical analyses were performed with the software program Comprehensive Meta Analysis 1.0.25 (Englewood, NJ).
Results
Identification of studies
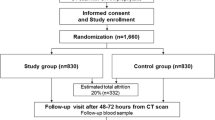
A total of 2,173 unique citations were identified by our search strategy (Fig. 1). After the initial screen, 332 citations were selected for further review. All of these citations were identified by the electronic search strategy and were published in peer-reviewed journals. Only 17 studies (all published between 2004 and 2008; 9 available only in abstract format; presented at international meetings) that investigated the role of sodium bicarbonate for prophylaxis for CIN [19–36] were randomized controlled trials.
Flow diagram of study selection process. Abbreviations: RCTs randomized controlled trials, ASN American Society of Nephrology, ISN International Society of Nephrology, AHA American Heart Asscociation, ACC American College of Cardiology, ASA American Society of Anesthesiologists, ACCP American College of Clinical Pharmacists
Patient characteristics
A total of 2,448 patients were examined in these trials, among whom 1,225 received sodium bicarbonate and 1,223 were in control groups. Key elements of study methods and reporting varied among studies [41]. Overall, the quality of the included studies was low to moderate.
Table 1 describes baseline characteristics of the study patients. The mean age ranged from 61 to 76 years, and men constituted 68–88% of participants. Nine studies included diabetic patients, with the prevalence ranging between 27 and 55% in these studies [19, 23, 24, 26, 29, 33–36]. Ten studies were performed exclusively in patients with stable chronic kidney disease [19, 23, 25, 26, 29–33, 36]. In one study, there were only nine patients (8%) with chronic kidney disease, of whom four were in the sodium bicarbonate group and five in the control group [20].
Intervention
The dosing and schedule of administration of sodium bicarbonate were similar in all studies. Of note, sodium bicarbonate was used alone in 12 studies [19, 20, 22, 25–27, 29–31, 33, 35, 36] and together with NAC in 5 studies [21, 23, 24, 32, 34]. Four studies compared sodium bicarbonate and NAC [20, 22, 26, 29]. All patients received a hydration protocol with their angiographic procedure, and the most common dose was 0.9% isotonic saline at 1 ml kg−1 h−1. The most common schedule of hydration was for 12 h before the procedure. Patients received non-ionic, iso-osmolar or low-osmolar or high-osmolar contrast media, and the mean dose of contrast media ranged from 130 to 290 ml. In four studies, diuretics were withheld on the day of contrast injection [19, 24, 35, 36].
The definitions of CIN varied across studies. Two studies defined CIN as a >0.5 mg/dl increase in serum creatinine from baseline [23, 34], 13 studies used a >25% increase in serum creatinine from baseline [19, 21, 22, 24–35], and one study used a >25% decrease in the glomerular filtration rate [36]. Except for one study [34], the time for ascertaining CIN for all studies was 48–72 h after exposure to contrast media. Protocols for administration and total cumulative dosages of sodium bicarbonate varied across the studies. The most common protocol was sodium bicarbonate 3 ml kg−1 h−1 1 h before and 1 ml kg−1 h−1 for 6 h during and after the procedure for the bicarbonate group and isotonic saline 3 ml kg−1 h−1 1 h before and 1 ml kg−1 h−1 for 6 h during and after the procedure for the control group.
Outcomes
Contrast-induced nephropathy
All studies reported the main outcome measure, incidence of CIN, the secondary outcome measure and mean change in creatinine at 48–72 h. All studies reported on the need for RRT. The overall incidence of CIN was 11.3%. Using the results from all 17 studies that compared bicarbonate versus saline, the pooled relative risk of developing CIN was 0.54 (95% CI, 0.36–0.83) in the intervention arm, indicating a statistically significant trend towards a benefit from sodium bicarbonate (Fig. 2). Regarding the secondary outcomes, CIN requiring dialysis only occurred in 17 patients: 6 received sodium bicarbonate, and 11 were in the control group (P = NS).
Sensitivity analysis
In an effort to explore the potential causes of heterogeneity, we performed sensitivity analyses by separating the studies into two subgroups. We grouped the studies based on whether NAC was administered together with sodium bicarbonate or not. There were 11 randomized controlled studies not using NAC and 5 studies using a combination of NAC and sodium bicarbonate. The pooled relative risk from the studies analyzing only sodium bicarbonate was similar to the overall effect size (pooled RR 0.38, 95% CI, 0.18–0.79). Furthermore, we analyzed four randomized controlled studies that compared the effects of sodium bicarbonate and NAC on development of CIN. The pooled relative risk was 0.57 (95% CI, 0.35–0.95), (Fig. 3).
Need for renal replacement therapy
There was no difference in the need for renal replacement therapy between the sodium bicarbonate and control group in 11 trials, 6 of 935 (0.6%) versus 11 of 927 (1.2%); the pooled relative risk was 0.64 (95% CI, 0.27–1.53) (Fig. 4).
Mortality
There was no difference in mortality between the sodium bicarbonate and control group in 4 trials, 8 of 513 (1.6%) versus 12 of 512 (2.3%); the pooled relative risk was 0.74 (95% CI, 0.29–1.87) (Fig. 5).
Discussion
The salient findings of this meta-analysis indicate that (1) the administration of sodium-bicarbonate-based fluids significantly reduces the risk of CIN compared to other standard prophylactic hydration regimens, (2) administration of sodium-bicarbonate-based fluids significantly reduces the risk of CIN compared to NAC and (3) administration of sodium-bicarbonate-based fluids has no superiority in preventing the need for renal replacement therapy and decreasing the rate of mortality due to CIN compared to other standard prophylactic hydration regimens. We demonstrate that the use of sodium bicarbonate reduces the risk of CIN by 54–83% to an overall incidence of CIN 8%. However, we found a publication bias that may influence the results in favor of sodium-bicarbonate-based fluids for prevention of the development of CIN.
CIN is the third most common cause of hospital-acquired renal failure [42–45]. Moreover, the use of elective and particularly emergency coronary angiography continues to increase, and patients are opting for medical treatment more frequently than for surgical solutions. In the highest risk patients, i.e., those with a total risk score ≥16 (according to the score described by Mehran et al. [6]), the risk of a 25% increase in serum creatinine is 57.3%, and the risk of dialysis is 12.6% after percutaneous coronary intervention [6]. Most importantly, CIN is associated with markedly increased short-term and long-term mortality. Therefore, determining the best strategies to minimize CIN is an important objective. Volume supplementation and the use of the smallest amount of low/iso-osmolar contrast agents are currently recommended strategies for CIN prevention [46]. However, in patients at high risk—as defined by available and validated risk stratification algorithms [11]—additional measures might be required. Reactive oxygen species (ROS) generated by contrast media may enhance the effects of vasoconstrictors; subsequently, medullary hypoxia further promotes mithocondrial generation of ROS. Thus, it seems reasonable to combine agents targeting the various pathogenic mechanisms of CIN, particularly antioxidative-oriented treatments, such as NAC, bicarbonate and ascorbic acid—the most investigated compounds. However, two large retrospective studies suggested that sodium bicarbonate was not beneficial for prevention of CIN [37, 38]. In our analyses, data from the 17 RCTs in our systematic review demonstrated a protective effect of sodium bicarbonate [19–36] when compared to saline alone or saline plus NAC.
While NAC prevents direct oxidative stress in a dose-dependent manner, working through pathways similar to ascorbic acid, bicarbonate may also intervene in a different, additive manner. Most importantly, it is an efficient and rapid method to alkalinize the renal tubular fluid. At the kidney (tubular) level, free radical generation is promoted and enhanced by the typical acidic milieu and is inhibited by the higher pH of normal extracellular fluid. This is clinically relevant, as supported by the increased risk of CIN observed in patients with enhanced urinary acid excretion from high aldosterone (dehydration, congestive heart failure, hypoproteinemia). The beneficial effect of sodium bicarbonate is not related to a better (compared to sodium chloride) direct volume expansion [47]. Indeed, in animal models, pretreatment with sodium bicarbonate is more protective than sodium chloride for prevention of acute kidney injury promoted by ischemia [48] or doxorubicin [49].
The achievement of sodium bicarbonate in reducing the development of CIN does not seem to be only due to the result of volume expansion but is consistent with the hypothesis that contrast injury is from the increased production of free radicals, which may play a role in the effects of various vasoconstrictors, generated within the acid environment of the renal medulla [50]. Furthermore, medullary hypoxia also contributes to mitochondrial generation of reactive oxygen species, which have a major role in the development of CIN [51]. In the previous studies, it was shown that free-radical formation is promoted by an acidic environment typical of tubular urine, but it is inhibited by the higher pH of normal extracellular fluid [52]. At physiological concentrations, bicarbonate also scavenges peroxynitrite and other reactive species generated from nitric oxide [53]. Thus, alkalinizing renal tubular fluid with bicarbonate may prevent the development of CIN by reducing renal injury by slowing the free radical production in the renal medulla.
There are several methodological limitations that were relevant when the impact of sodium bicarbonate was assessed from the studies included in this review. In 9 of the 17 studies cited, sodium bicarbonate was compared to saline alone—in each of these 9 trials, the saline regimens differed in the amounts administered, timing of administration and duration of therapy. In one study, the dose and manner of administration of NAC differed between the control and intervention [23]. Furthermore, there was considerable variation in the degree of renal dysfunction in the cohorts studied, ranging from a mean serum creatinine of 0.8 mg/dl (Lin et al. [27]) to 1.95 mg/dl (Recio-Mayoral et al. [23]). There was also considerable variation in the definitions of CIN among the studies. Despite the reported association of CIN with impaired outcomes, no trial examined clinical hard outcomes, such as long-term dialysis dependency and mortality, length of hospital stay, hospital mortality and morbidity. Another limitation of the studies examined are that all studies included fewer than 110 patients per intervention arm and could have represented false-positive results. In the landmark trial by Merten et al. [19], 13% of the initially randomized subjects were lost from analysis, and the trial was terminated early. The timing of the interim analysis and the stopping rules were not prespecified, and the P value for the difference in event rates (P = 0.02) was higher than the standard for stopping a trial early. In addition, the statistical power of the trial reported by Ozcan et al. [26] may also be insufficient due to the small size of the study population, while the study reported by Lin et al. [27] offered preliminary data also derived from a small population. A second relevant methodological issue is related to the type of population included. The results from the trial reported by Briguori et al. [24] cannot be extended to high-risk patients (with a risk score ≥16, see above). Similarly, the study reported by Mora et al. [25] did not include patients with acute renal failure, diabetes mellitus, overt hypervolemia or those on non-steroid antiinflammatory drugs. However, most of the patients requiring contrast have such risk factors. Finally, Brar et al. [36] included patients with a GFR ≤60 ml min−1 1.73 m−2 (stage 3 chronic kidney disease). Therefore, the results of these studies cannot be extended to all patients (with GFR >60 ml min−1 1.73 m−2 and/or high risk). Additional relevant issues should also be underlined. In the RENO study [23], the definition of the primary endpoint was different from the other seven RCTs, and the prevalence of CIN in the control and intervention arms was significantly high (22 and 15%, respectively), although the proportion of very high risk patients is not reported. Although the study of Recio-Mayoral has several differences from other studies because of the different hydration protocols used in the treatment arms, we performed an analysis with and without that study, and we obtained similar results [20]. Most of the studies were performed in single centers and were not blinded. Taking into account the discrepancy between the results provided by retrospective analyses [37, 38], the largest RCT study [34, 36] and the current meta-analysis, we suggest that additional larger and better designed RCTs are warranted. Despite any inherent limitations of pooling and meta-analyzing the above-mentioned data, increasing the effective sample size will bring further support and greater precision to the point estimate of the protective effect of sodium bicarbonate. Finally, studies included in the present meta-analysis measured a surrogate outcome as their primary endpoint (CIN based on change in serum creatinine) and not hard outcomes, such as dialysis-requiring CIN or death; we were also not able to assess the protective effect of sodium bicarbonate for dialysis-requiring CIN because the incidence of this endpoint was too low in these studies. These limitations may be the reason we observed a high amount of statistical heterogeneity when we pooled the results.
In conclusion, despite the limitations noted above, the use of sodium bicarbonate appears to be an effective strategy for the prevention of CIN. Further studies are needed to determine whether sodium bicarbonate will reduce clinically meaningful patient-centered outcomes (e.g., need for dialysis or death) in high-risk patients. However, until these studies are performed and the definitive data emerge, it appears that sodium bicarbonate can be safely applied to patients at risk for CIN without much risk for adverse events or significant cost.
References
Murphy SW, Barrett BJ, Parfrey PS (2000) Contrast nephropathy. J Am Soc Nephrol 11:177–182
Weisbord SD, Chen H, Stone RA, Kip KE, Fine MJ, Saul MI, Palevsky PM (2006) Associations of increases in serum creatinine with mortality and length of hospital stay after coronary angiography. Am Soc Nephrol 17(10):2871–2877. doi:10.1681/ASN.2006030301
Rudnick M, Feldman H (2008) Contrast-induced nephropathy: what are the true clinical consequences? Clin J Am Soc Nephrol 3(1):263–272. doi:10.2215/CJN.03690907
Dangas G, Iakovou I, Nikolsky E, Aymong ED, Mintz GS, Kipshidze NN, Lansky AJ, Moussa I, Stone GW, Moses JW, Leon MB, Mehran R (2005) Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol 95:13–19. doi:10.1016/j.amjcard.2004.08.056
Toprak O, Cirit M, Yesil M, Bayata S, Tanrisev M, Varol U, Ersoy R, Esi E (2007) Impact of diabetic and pre-diabetic state on development of contrast-induced nephropathy in patients with chronic kidney disease. Nephrol Dial Transplant 22:819–826. doi:10.1093/ndt/gfl636
Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, Mintz GS, Lansky AJ, Moses JW, Stone GW, Leon MB, Dangas G (2004) A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol 44:1393–1399
Levy EM, Viscoli CM, Horwitz RI (1996) The effect of acute renal failure on mortality. A cohort analysis. JAMA 275:1489–1494. doi:10.1001/jama.275.19.1489
Gruberg L, Mehran R, Dangas G, Mintz GS, Waksman R, Kent KM, Pichard AD, Satler LF, Wu H, Leon MB (2001) Acute renal failure requiring dialysis after percutaneous coronary interventions. Catheter Cardiovasc Interv 52:409–416. doi:10.1002/ccd.1093
Rihal CS, Textor SC, Grill DE, Berger PB, Ting HH, Best PJ, Singh M, Bell MR, Barsness GW, Mathew V, Garratt KN, Holmes DR Jr (2002) Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation 105:2259–2264. doi:10.1161/01.CIR.0000016043.87291.33
Fishbane S, Durham JH, Marzo K, Rudnick M (2004) N-acetylcysteine in the prevention of radiocontrast-induced nephropathy. J Am Soc Nephrol 15:251–260. doi:10.1097/01.ASN.0000107562.68920.92
Gruberg L, Mintz GS, Mehran R, Gangas G, Lansky AJ, Kent KM, Pichard AD, Satler LF, Leon MB (2000) The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Coll Cardiol 36:1542–1548. doi:10.1016/S0735-1097(00)00917-7
Bakris GL, Lass N, Gaber AO, Jones JD, Burnett JC (1990) Radiocontrast medium-induced declines in renal function: a role for oxygen free radicals. Am J Physiol 258:115–120
Persson PB, Hansell P, Liss P (2005) Pathophysiology of contrast-medium induced nephropathy. Kidney Int 68:14–22. doi:10.1111/j.1523-1755.2005.00377.x
Solomon R, Werner C, Mann D, D’Alia J, Silva P (1994) Effects of saline, mannitol, and furosemide on acute decreases in renal function induced by radiocontrast agents. N Engl J Med 331:1416–1420. doi:10.1056/NEJM199411243312104
Huber W, Ilgmann K, Page M, Hennig M, Schweigart U, Jeschke B, Lutilsky L, Weiss W, Salmhofer H, Classen M (2002) Effect of theophylline on contrast material-nephropathy in patients with chronic renal insufficiency: controlled, randomized, double-blinded study. Radiology 223:772–779. doi:10.1148/radiol.2233010609
Kay J, Chow WH, Chan TM, Lo SK, Kwok OH, Yip A, Fan K, Lee CH, Lam WF (2003) Acetylcysteine for prevention of acute deterioration of renal function following elective coronary angiography and intervention: a randomized controlled trial. JAMA 289:553–558. doi:10.1001/jama.289.5.553
Aspelin P, Aubry P, Fransson SG, Strasser R, Willenbrock R, Berg KJ, Nephrotoxicity in High-Risk Patients Study of Iso-Osmolar and Low-Osmolar Non-Ionic Contrast Media Study Investigators (2003) Nephrotoxic effects in high-risk patients undergoing angiography. N Engl J Med 348:491–499. doi:10.1056/NEJMoa021833
Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC (2008) Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med 148(4):284–294
Merten GJ, Burgess WP, Gray LV, Holleman JH, Roush RS, Kowalchuk GJ, Bersin RM, Van Moore A, Simonton CA, Rittase RA, Norton HJ, Kennedy TP (2004) Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. JAMA 291:2328–2334. doi:10.1001/jama.291.19.2328
Hill S, Fowler S, Sikand H, Phillips P (2005) Comparison of oral N-actylcysteine versus intravenous sodium bicarbonate in contrast-induced nephropathy treatment (CONVICT Trial). Pharmacotherapy 25(10):1433
Saidin R, Zainudin S, Kong NCT et al (2006) Intravenous sodium bicarbonate versus normal saline infusion as prophylaxis against contrast nephropathy in patients with chronic kidney disease undergoing coronary angiography or angioplasty. J Am Soc Nephrol 17:766A
Addad F, Gamra H, Jemmali M, Dridi Z, Ben Hamda K, Bethout F, Maatoug F, Ben Farhat M (2006) Acetylcysteine versus bicarbonate or combination to prevent contrast-induced nephropathy in patients with diabetes and chronic renal insufficiency: ABC contrast study. Eur Heart J 27(Suppl 1):246–247
Recio-Mayoral A, Chaparro M, Prado B, Cózar R, Méndez I, Banerjee D, Kaski JC, Cubero J, Cruz JM (2007) The reno-protective effect of hydration with sodium bicarbonate plus N-acetylcysteine in patients undergoing emergency percutaneous coronary intervention: the RENO Study. J Am Coll Cardiol 49:1283–1288. doi:10.1016/j.jacc.2006.11.034
Briguori C, Airoldi F, D’Andrea D, Bonizzoni E, Morici N, Focaccio A, Michev I, Montorfano M, Carlino M, Cosgrave J, Ricciardelli B, Colombo A (2007) Renal insufficiency following contrast media administration trial (REMEDIAL): a randomized comparison of 3 preventive strategies. Circulation 115:1211–1217
Mora JA, Macaraeg CR, Mora RC (2007) Urinary alkalinization and contrast nephropathy. World Congress of Nephrology, T-PO-1650, p 513
Ozcan EE, Guneri S, Akdeniz B, Akyildiz IZ, Senaslan O, Baris N, Aslan O, Badak O (2007) Sodium bicarbonate, N-acetylcysteine, and saline for prevention of radiocontrast-induced nephropathy. A comparison of 3 regimens for protecting contrast-induced nephropathy in patients undergoing coronary procedures. A single-center prospective controlled trial. Am Heart J 154(3):539–544. doi:10.1016/j.ahj.2007.05.012
Lin M, Sabeti M, Iskander E, Malhotra N, Pham PTT, Pham PCT (2007) Prevention of contrast nephropathy with sodium bicarbonate. American Sciety of Nephrology Renal Week, PUB591
Masuda M, Yamada T, Mine T, Morita T, Tamaki S, Tsukamoto Y, Okuda K, Iwasaki Y, Hori M, Fukunami M (2007) Comparison of usefulness of sodium bicarbonate versus sodium chloride to prevent contrast-induced nephropathy in patients undergoing an emergent coronary procedure. Am J Cardiol 100(5):781–786. doi:10.1016/j.amjcard.2007.03.098
Shaikh F, Maddikunta R, Museitif R, Haddadian B, Dochee J, Qureshi J, Wallach JD, Solis J, Tumuluri R, Bajwa T, Allaqaband S (2007) A prospective randomzed trial comparing normal saline and sodium bicarbonate with or without N-acetylcysteine for prevention of contrast-induced nephropathy. Am J Cardiol 100(8A):122L–123L (Suppl S)
Kim H, Kim KS, Shin JH, Lee CH, Kang CM (2007) Hydration with sodium bicarbonate for the preventon of radio contrast-induced nephropathy. Nephrol Dial Transplant 22(Suppl 6):49
Chen H, Wu H, He Q, Chen H (2007) Comparison of sodium bicarbonate and sodium chloride as strateges for preventing contrast nephropathy. J Am Soc Nephrol 18:817A. doi:10.1681/ASN.2006091021
Heguilen R, Liste A, Rosende G et al (2007) Prevention of contrast-induced nephropathy: volume expansion, N-actylcysteine or both? Results from a pilot study. Nephrol Dial Transplant 22(Suppl 6):54
Adolph E, Holdt-Lehmann B, Chatterjee T, Paschka S, Prott A, Schneider H, Koerber T, Ince H, Steiner M, Schuff-Werner P, Nienaber CA (2008) Renal insufficiency following radio contrast exposure trial (REINFORCE): a randomized comparison of sodium bicarbonate versus sodium chloride hydration for the prevention of contrast-induced nephropathy. Coron Artery Dis 19(6):413–419
Maioli M, Toso A, Leoncini M, Gallopin M, Tedeschi D, Micheletti C, Bellandi F (2008) Sodium bicarbonate versus saline for the prevention of contrast-induced nephropathy in patients with renal dysfunction undergoing coronary angiography or intervention. J Am Coll Cardiol 52(8):599–604. doi:10.1016/j.jacc.2008.05.026
Masuda M, Yamada T, Okuyama Y, Morita T, Sanada S, Furukawa Y, Tsukamoto Y, Okuda K, Iwasaki Y, Yasui T, Fukunami M (2008) Sodium bicarbonate improves long-term clinical outcomes compared with sodium chloride in patients with chronic kidney disease undergoing an emergent coronary procedure. Circ J 72(10):1610–1614. doi:10.1253/circj.CJ-08-0368
Brar SS, Shen AY, Jorgensen MB, Kotlewski A, Aharonian VJ, Desai N, Ree M, Shah AI, Burchette RJ (2008) Sodium bicarbonate vs sodium chloride for the prevention of contrast medium-induced nephropathy in patients undergoing coronary angiography: a randomized trial. JAMA 300(9):1038–1046. doi:10.1001/jama.300.9.1038
From AM, Bartholmai BJ, Williams AW, Cha SS, Pflueger A, McDonald FS (2008) Sodium bicarbonate is associated with an increased incidence of contrast nephropathy: a retrospective cohort study of 7977 patients at mayo clinic. Clin J Am Soc Nephrol 3(1):10–18. doi:10.2215/CJN.03100707
Schmidt P, Pang D, Nykamp D, Knowlton G, Jia H (2007) N-acetylcysteine and sodium bicarbonate versus N-acetylcysteine and standard hydration for the prevention of radiocontrast-induced nephropathy following coronary angiography. Ann Pharmacother 41(1):46–50. doi:10.1345/aph.1H354
Hogan SE, L’Allier P, Chetcuti S, Grossman PM, Nallamothu BK, Duvernoy C, Bates E, Moscucci M, Gurm HS (2008) Current role of sodium bicarbonate-based preprocedural hydration for the prevention of contrast-induced acute kidney injury: a meta-analysis. Am Heart J 156(3):414–421. doi:10.1016/j.ahj.2008.05.014
Navaneethan SD, Singh S, Appasamy S, Wing RE, Sehgal AR (2009) Sodium bicarbonate therapy for prevention of contrast-induced nephropathy: A systematic review and meta-analysis. Am J Kidney Dis 53(4):617–627
Jadad A, Moore R, Carrol D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–12. doi:10.1016/0197-2456(95)00134-4
Tepel M, Aspelin P, Lameire N (2006) Contrast-induced nephropathy: a clinical and evidence-based approach. Circulation 113(14):1799–1806. doi:10.1161/CIRCULATIONAHA.105.595090
Nash K, Hafeez A, Hou S (2002) Hospital-acquired renal insufficiency. Am J Kidney Dis 39(5):930–936. doi:10.1053/ajkd.2002.32766
Rosenstock JL, Bruno R, Kim JK, Lubarsky L, Schaller R, Panagopoulos G, DeVita MV, Michelis MF (2008) The effect of withdrawal of ACE inhibitors or angiotensin receptor blockers prior to coronary angiography on the incidence of contrast-induced nephropathy. Int Urol Nephrol 40(3):749–755. doi:10.1007/s11255-008-9368-1
Lima RS, Marques CN, Silva Júnior GB, Barbosa AS, Barbosa ES, Mota RM, Araújo SM, Gutiérrez-Adrianzén OA, Libório AB, Daher EF (2008) Comparison between early and delayed acute kidney injury secondary to infectious disease in the intensive care unit. Int Urol Nephrol 40(3):731–739. doi:10.1007/s11255-008-9352-9
Barrett BJ, Carlisle EJ (1993) Metaanalysis of the relative nephrotoxicity of high- and low-osmolality iodinated contrast media. Radiology 188(1):171–178
Julian BA, Galla JH, Guthrie GP Jr, Kotchen TA (1982) Renin and aldosterone responses to short-term NaCl or NaHCO3 loading in man. J Lab Clin Med 100(2):261–268
Halliwell B, Gutteridge JM (1990) Role of free radicals and catalytic metal ions in human disease: an overview. Methods Enzymol 186:1–85. doi:10.1016/0076-6879(90)86093-B
Baroni EA, Costa RS, Volpini R, Coimbra TM (1999) Sodium bicarbonate treatment reduces renal injury, renal production of transforming growth factor-beta, and urinary transforming growth factor-beta excretion in rats with doxorubicin-induced nephropathy. Am J Kidney Dis 34(2):328–337. doi:10.1016/S0272-6386(99)70363-X
Persson PB, Hansell P, Liss P (2005) Pathophysiology of contrast medium-induced nephropathy. Kidney Int 68(1):14–22. doi:10.1111/j.1523-1755.2005.00377.x
Chandel NS, McClintock DS, Feliciano CE, Wood TM, Melendez JA, Rodriguez AM, Schumacker PT (2000) Reactive oxygen species generated at mitochondrial complex III stabilize hypoxia-inducible factor-1alpha during hypoxia: a mechanism of O2 sensing. J Biol Chem 275(33):25130–25138. doi:10.1074/jbc.M001914200
Sporer H, Lang F, Oberleithner H, Greger R, Deetjen P (1981) Inefficacy of bicarbonate infusions on the course of postischaemic acute renal failure in the rat. Eur J Clin Invest 11(4):311–315. doi:10.1111/j.1365-2362.1981.tb02122.x
Cohen G (1985) The fenton reaction. In: Greenwald RA (ed) CRC handbook of methods for oxygen radical research. CRC Press, Boca Raton, pp 55–64
Disclosures
No financial support was obtained from any institution or company except for logistic support from the authors’ affiliation departments.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript has been seen by all authors. It has not been submitted in similar form for publication elsewhere.
Rights and permissions
About this article
Cite this article
Kanbay, M., Covic, A., Coca, S.G. et al. Sodium bicarbonate for the prevention of contrast-induced nephropathy: a meta-analysis of 17 randomized trials. Int Urol Nephrol 41, 617–627 (2009). https://doi.org/10.1007/s11255-009-9569-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-009-9569-2