Abstract
Objective
Aortic stiffness measured by pulse wave velocity (PWV) predicts all-cause and cardiovascular mortality in hemodialysis (HD) patients. However, there is a lack of information on stiffness parameter β, another index of arterial stiffness, in HD patients. The aim of the present study was to investigate the clinical usefulness of stiffness parameter β in HD patients.
Materials and methods
We compared the relation of stiffness parameter β to carotid intima-media thickness (IMT) and plaque score estimated by carotid ultrasound and investigated the relationship between stiffness parameter β and silent cerebral infarction (SCI) in 64 HD patients.
Results
Stiffness parameter β was positively correlated with mean IMT (r = 0.318, P = 0.0113) and plaque score (r = 0.672, P < 0.0001). Stepwise regression analysis revealed that pulse pressure and age were found to be independent determinants of stiffness parameter β (partial correlation coefficients: β = 0.501 and P < 0.0001 for pulse pressure, β = 0.488 and P < 0.0001 for age). In addition, stiffness parameter β in patients with SCI (12.2 ± 3.9) was significantly higher than those (8.0 ± 2.4) in patients without SCI. However, there was no significant difference in mean IMT and plaque score in both groups.
Conclusion
These results suggest that arteriosclerosis assessed by stiffness parameter β is associated with atherosclerotic changes of carotid arteries and with the presence of SCI in HD patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Arterial stiffness is an independent predictor of all-cause and cardiovascular mortality in patients on chronic hemodialysis (HD) [1, 2]. Arterial stiffness can be evaluated by measuring pulse wave velocity (PWV) between two sites in the arterial tree [3]. However, aortic PWV measurement is technically difficult and has low reproducibility [4]. Brachial-ankle PWV (baPWV), which provides a more convenient assessment of arterial stiffness, has been developed in Japan [5–7]. However, the problem with the clinical use of baPWV is that the index is significantly dependent on blood pressure levels [8]. On the other hand, stiffness parameter β was reported to be independent of blood pressure [9]. The stiffness parameter β has been used to evaluate arterial stiffness in patients with type 2 diabetes [10] and patients with chronic renal failure [11]. However, its clinical usefulness has not yet been fully clarified in HD patients.
An alternative method for evaluating arterial stiffness is the relative change in lumen diameter during the cardiac cycle adjusted for driving pulse pressure, expressed as arterial distensibility. Carotid distensibility is measured by ultrasound imaging. An ultrasound imaging of the common carotid artery (CCA) has been developed for the evaluation of early atherosclerotic lesions [12–14]. HD patients exhibit markedly increased intima-media thickness (IMT), a higher prevalence of plaques in the CCA compared to control subjects [15–17].
The aim of the present study was to measure stiffness parameter β and examine the relation of stiffness parameter β to IMT, plaque score or biochemical parameters in patients on chronic HD. In addition, we assessed the correlation between stiffness parameter β and silent cerebral infarction (SCI) estimated by magnetic resonance imaging (MRI).
Methods
Study subjects
The study subjects were 64 maintenance HD patients (31 men and 33 women) treated at the Dialysis Unit of Hidaka Hospital. HD was performed three times weekly (4 h/day). The dialysis potassium concentration was 2.0 mEq/l, and the calcium concentration was 3.0 mEq/l. Blood pressure was recorded three times with a brachial sphygmomanometer, after the subject had rested in the supine position for at least 10 min and the average value of the three measurements was adopted. Hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg, or use of antihypertensive medication. Pulse pressure was calculated by the formula PP = SBP − DBP. Diabetes mellitus (DM) was defined by World Health Organization (WHO) criteria [18]. Patients with congestive heart failure, atrial fibrillation, malignant tumor or autoimmune diseases were excluded. All measurements as listed below were performed after dialysis session except blood sampling. Information about antihypertensive medications was obtained from medical charts and analyzed. This study was in compliance with the Declaration of Helsinki and was in agreement with the guidelines approved by the ethics committee of our institution; informed consent was obtained from each patient.
Ultrasound evaluation
Ultrasound evaluation of the CCA was performed with an Aplio (Toshiba Co., Tokyo, Japan) using a 7.5-MHz probe equipped with a Doppler system. After the subjects had rested in the supine position for at least 10 min, their neck was placed in a slightly hyperextended position, and then optimal bilateral visualization of the CCA was performed. Based on multiple visualizations, plaque formation was identified as the presence of wall thickening at least 50% greater than the thickness of the surrounding wall. To evaluate the distribution of atherosclerosis in the CCA, we used a plaque scoring method as previously described [13]. The plaque score was computed by summing the maximum thickness of the intima-media complex, measured in millimeters, on the near and far walls of each of four divisions on both sides of the carotid arteries. The length of the individual plaques was not considered in determining the plaque score. The IMT of the far wall was measured in the CCA as sites 1 and 2 cm proximal to the bulb from the anterior, lateral, and posterior approaches, and the results were averaged in order to obtain the mean IMT values. No measurements were carried out at the level of discrete plaques.
Two-dimensional guide M-mode tracing of the right CCA 2 cm proximal to the bulb was recorded with simultaneous electrocardiogram and phonocardiogram. M-mode images were obtained in real time using a frame grabber. The axial resolution of the M-mode system was 0.1 mm. The internal diameters of the CCA at end diastole (Dd) and peak systole (Ds) were determined by continuous tracing of the intimal-luminal interface of the near and far wall of the CCA during three cycles, and the results were then averaged. The stiffness parameter β was calculated by the following formulae:
Intraobserver intrasession variability was evaluated from three repeated measurements in one session. The coefficient of variation of the three measurements was calculated in each subject. Intraobserver intersession variability was studied by one observer by performing two sessions on different days. The intraobserver intrasession variability was less than 10%, and the intraobserver intersession variability was less than 15%. SBP and DBP were measured at the brachial artery in the arm without blood access by an automated sphygmomanometer (Omlon-Colin Co., Tokyo, Japan) immediately after the evaluation of carotid ultrasound.
Magnetic resonance imaging (MRI)
All participating patients had a brain MRI (EXCELART, Toshiba Co., Tokyo, Japan) and used a superconducting magnet at a field strength of 1.5 T on proton density, T1-, and T2-weighted images in axial planes at 10-min-thick slices. Infarction was defined as a focal area larger than 3 mm in diameter in both T1- and T2-weighted images that was visible as low-signal intensity areas on T1-weighted image and as high-signal intensity areas on T2-weighted image. The MR images were assessed independently by two neuroradiologists who had not been notified of any clinical information.
Laboratory data
Blood samples were drawn after an overnight fast of at least 12 h before dialysis session, and serum creatinine (automated enzymatic method), urea, glucose, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), triglyceride (TG), albumin, calcium (Ca), phosphate (P), and C-reactive protein (CRP) levels were determined by using routine biochemical methods. With regard to the urea kinetics, we measured a blood-based dialysis parameter, Kt/V [19]. Serum intact parathyroid hormone (iPTH) was measured by commercially available radioimmunoassay.
Statistical analysis
Data are expressed as mean ± standard deviation. Pearson’s correlation coefficient was used to assess the association between continuous variables. Student's unpaired t-test was used to analyze the comparisons between means. We used stepwise multiple regression analysis to evaluate the independent determinants of stiffness β. Differences with P less than 0.05 are considered statistically significant. Statistical analyses were performed using SPSS software, version 11.0 (SPSS Inc., Chicago, IL).
Results
Characteristics of the study participants
The mean age of the participants was 64.9 ± 16.5 years, and the mean duration of dialysis was 8.7 ± 5.8 years. Underlying diseases of end-stage renal disease were 32 with chronic glomerulonephritis, 22 with DM, 5 with polycystic kidney disease, 3 with nephrosclerosis and 2 with unknown origin. All HD patients were treated with antihypertensive drugs, including calcium channel blockers (62 patients), angiotensin II receptor blockers/angiotensin-converting enzymes (51 patients), α-blockers (17 patient) and β-blockers (10 patients). Three (4.7%) patients were treated with statins, and 45 (70.3%) were treated with anti-platelet drugs. The clinical characteristics and data of stiffness β and carotid parameters of the study subjects are summarized in Table 1. Twenty-eight (45.2%) had SCI as a lacunar infarction.
Correlation between stiffness parameter β and clinical variables
We examined the relationships between stiffness parameter β and pro-atherosclerotic factors, such as age, SBP and DBP, pulse pressure, Kt/V, TC, TG, HDL-C, Ca, P, iPTH, albumin, and CRP.
As shown in Table 2, the univariate linear regression analysis showed that the stiffness parameter β was strongly correlated with age and pulse pressure, weakly correlated with DBP and CRP, and not correlated at all with duration of dialysis, SBP, Kt/V, TC, TG, HDL-C, Ca, P, iPTH, or albumin. No significant difference in stiffness parameter β was noted in diabetic patients (10.4 ± 3.7) or non-diabetic patients (9.6 ± 3.8) (P = 0.1876). Because these factors may be associated with each other, stepwise multiple regression analyses were performed to evaluate the independent determinants of stiffness parameter β using age, DBP, pulse pressure, and CRP as covariates. Pulse pressure and age were found to be independent determinants of stiffness parameter β (partial correlation coefficients: β = 0.501 and P < 0.0001 for pulse pressure, β = 0.488 and P < 0.0001 for age). In general, increased arterial stiffness is the cause of greater pulse pressure. However, it is likely that this statistical model included pulse pressure as a possible determinant of stiffness parameter β.
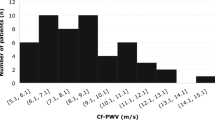
Correlation between stiffness parameter β and carotid ultrasound parameters or SCI
In an attempt to investigate the relation of stiffness β to carotid atherosclerosis, univariate analysis was performed. There was a significant positive correlation between stiffness parameter β and mean IMT (r = 0.318, P = 0.0113) (Fig. 1) and plaque score (r = 0.672, P < 0.0001) (Fig. 2). The independent determinant factors of stiffness parameter β were mean IMT (β = 0.471, P = 0.0116) and plaque score (β = 0.672, P < 0.0001) estimated by a stepwise regression analysis using mean IMT and plaque score as covariates. Accordingly, we compared carotid atherosclerotic or arteriosclerotic parameters in HD patients with or without SCI. As shown in Table 3, stiffness β in patients with SCI (12.2 ± 3.9) was significantly higher than those (8.0 ± 2.4) in patients without SCI. However, there was no significant difference in mean IMT and plaque score in both groups. These findings suggest that stiffness parameter β is affected by mean IMT independent of plaque score, and stiffness parameter β is affected by plaque score independent of mean IMT.
Discussion
Although the usefulness of measuring stiffness parameter β has been shown in type 2 diabetes mellitus and other populations, no previous paper is available for HD patients. In the present study, we found a strong correlation between stiffness parameter β and IMT or plaque score. Thus, this study provides novel information on stiffness parameter β in HD patients.
Atherosclerosis involves a combination of fatty degeneration (atherosis) and vessel stiffening (sclerosis) of the arterial wall [20]. Arterial stiffness is usually assessed in the aorta by measuring carotid-femoral PWV, but it can also be assessed in the CCA by measuring the distensibility coefficient. Atherosclerosis is commonly assessed by IMT and the presence of plaques in the carotid artery [21]. A significant relationship between PWV and IMT has been demonstrated, especially in the general population [21, 22]. Kawada et al. [23] reported that stiffness parameter β was higher in hypertensive HD patients than in non-hypertensive HD patients and was independently associated with age and hypertension. In the present study, stiffness parameter β was related to both IMT and plaque score in all HD patients treated with antihypertensive agents.
Makita et al. [24] reported that plaque score was reported to be more closely related to serum CRP level than to IMT in the general population. In the present study, stiffness parameter β was positively associated with CRP level (r = 0.320, P = 0.0108) in HD patients. It has been shown that baseline PWV as well as the changes of PWV during follow-up was independently associated with serum CRP level [25] in HD patients. They indicated that low-grade inflammation decreases the efficiency of cardiovascular therapeutic interventions and participates in the persistence of cardiovascular hemodynamic overload. These reports and our results suggest that the correlation between stiffness parameter β and plaque score may be stronger in HD patients with chronic inflammation in HD patients. Moreover, Tseke et al. [26] reported that stiffening and atherosclerosis are associated with chronic inflammation as well as DBP in HD patients.
SCI is thought to be an underlying or concomitant condition of clinical subcortical brain infarction or brain hemorrhage in the general population [27]. In most cases, SCI is found as a lacunar infarction, the most common form of subcortical infarction, defined by Fisher as a small, deep cerebral infarction caused by occlusion of small penetrating cerebral arteries [28]. Nakatani et al. [29] reported a higher incidence of SCI in HD patients compared with the control group using MRI studies (48.8% vs. 9.6%, respectively). They also showed that HD patients with SCI had a significantly higher cerebral and vascular morbidity than the group without SCI [30]. In the present study, stiffness parameter β in patients with SCI was significantly higher than those in patients without SCI, suggesting that carotid arteriosclerosis is associated with the presence of SCI in HD patients.
In order to overcome the problem that baPWV is significantly dependent on blood pressure levels, we used stiffness parameter β to evaluate the atherosclerotic burden in HD patients. Kanters et al. [31] reported the reproducibility of measurement of distensibility in the CCA, and showed that the intraobserver intrasession variability and the intraobserver intersession variability of stiffness parameter β were 19.1% and 25.4%, respectively. In the present study, the intraobserver intrasession variability was less than 10%, and the intraobserver intersession variability was less than 15%, showing that our reproducibility of measurement of stiffness parameter β was higher than those in the previous study. The stiffness parameter β should give the better estimate without pressure dependence of the real deformation behavior of the vascular wall within the physiological pressure range. Further prospective studies are required to evaluate if stiffness parameter β is a useful tool for predicting atherosclerotic burden and SCI in HD patients.
There were several limitations in our study, namely that the study population was relatively small and that we could not eliminate the effect of medications on stiffness parameter β level. Another limitation of this study is that brachial SBP and DBP were used to calculate the carotid stiffness parameter β instead of carotid SBP and DBP. Physiologically, mean blood pressure and DBP are nearly identical in the carotid and brachial arteries, whereas SBP and pulse pressure are significantly higher in the brachial arteries than the carotid arteries, although the differences are minimized with aging [32]. This may be a reason that stiffness parameter β was associated with mean IMT, although this association was relatively weak. The pulsatility index and/or resistive index might be an additional indicator for carotid arteriosclerosis in HD patients [33].
In conclusion, we demonstrated that stiffness parameter β was associated with carotid IMT and plaque score in HD patients. Stiffness parameter β may serve as a useful clinical marker for arteriosclerosis in HD patients with SCI.
References
Shoji T, Emoto M, Shinohara K et al (2001) Diabetes mellitus, aortic stiffness, and cardiovascular mortality in end-stage renal disease. J Am Soc Nephrol 12:2117–2124
Blacher J, Safar ME, Guerin AP, Pannier B, Marchais SJ, London GM (2003) Aortic pulse wave velocity index and mortality in end-stage renal disease. Kidney Int 63:1852–1860. doi:10.1046/j.1523-1755.2003.00932.x
Mattace-Raso FU, van der Cammen TJ, Hofman A et al (2006) Arterial stiffness and risk of coronary heart disease and stroke. Circulation 113:657–663. doi:10.1161/CIRCULATIONAHA.105.555235
Asmar R, Topouchian J, Pannier B, Benetos A, Safar M (2001) Pulse wave velocity as endpoint in large-scale intervention trial: the Complior study. Scientific quality control, coordination and investigation committees of the complior study. J Hypertens 19:813–818. doi:10.1097/00004872-200104000-00019
Kubo T, Miyata M, Minagoe S, Setoyama S, Maruyama I, Tei C (2002) A simple oscillometric technique for determining new indices of arterial distensibility. Hypertens Res 25:351–358. doi:10.1291/hypres.25.351
Yamashina A, Tomiyama H, Takeda K et al (2002) Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 25:359–364. doi:10.1291/hypres.25.359
Munakata M, Sakuraba J, Tayama J et al (2005) Higher brachial-ankle pulse wave velocity is associated with more advanced carotid atherosclerosis in end-stage renal disease. Hypertens Res 28:9–14. doi:10.1291/hypres.28.9
Matsui Y, Kario K, Ishikawa J, Eguchi K, Hoshide S, Shimada K (2004) Reproducibility of arterial stiffness indices (pulse wave velocity and augmentation index) simultaneously assessed by automated pulse wave analysis and their associated risk factors in essential hypertensive patients. Hypertens Res 27:851–857. doi:10.1291/hypres.27.851
Niki K, Sugawara M, Chang D et al (2002) A new noninvasive measurement system for wave intensity: evaluation of carotid arterial intensity and reproducibility. Heart Vessels 17:12–21. doi:10.1007/s003800200037
Kizu A, Koyama H, Tanaka S et al (2003) Arterial wall stiffness is associated with peripheral circulation in patients with type 2 diabetes. Atherosclerosis 170:87–91. doi:10.1016/S0021-9150(03)00237-5
Leskinen Y, Lehtimaki T, Loimaala A et al (2003) Carotid atherosclerosis in chronic renal failure-the central role of increased plaque burden. Atherosclerosis 171:295–302. doi:10.1016/j.atherosclerosis.2003.08.010
Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R (1986) Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation 74:1399–1406
Handa N, Matsumoto M, Maeda H et al (1990) Ultrasonic evaluation of early carotid atherosclerosis. Stroke 21:1567–1572
Yambe M, Tomiyama H, Hirayama Y et al (2004) Arterial stiffening as a possible risk factor for both atherosclerosis and diastolic heart failure. Hypertens Res 27:625–631. doi:10.1291/hypres.27.625
London GM, Guerin AP, Marchais SJ et al (1996) Cardiac and arterial interactions in end-stage renal disease. Kidney Int 50:600–608. doi:10.1038/ki.1996.355
Hojs R (2000) Carotid intima-media thickness and plaques in hemodialysis patients. Artif Organs 24:691–695. doi:10.1046/j.1525-1594.2000.06466.x
Kato A, Takita T, Maruyama Y, Hishida A (2004) Chlamydial infection and progression of carotid atherosclerosis in patients on regular hemodialysis. Nephrol Dial Transplant 19:2539–2546. doi:10.1093/ndt/gfh416
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553. doi:10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S
Daugirdas JT (1993) Second generation logarithmic estimates of single-pool variable volume Kt/V: an analysis of error. J Am Soc Nephrol 4:1205–1213
Taniwaki H, Kawagishi T, Emoto M et al (1999) Correlation between the intima-media thickness of the carotid artery and aortic pulse-wave velocity in patients with type 2 diabetes. Vessel wall properties in type 2 diabetes. Diabetes Care 22:1851–1857. doi:10.2337/diacare.22.11.1851
van Popele NM, Grobbee DE, Bots ML et al (2001) Association between arterial stiffness and atherosclerosis. The Rotterdam study. Stroke 32:454–460
Paini A, Boutouyrie P, Calvet D, Tropeano A-I, Laloux B, Laurent S (2006) Carotid and aortic stiffness: determinants of discrepancies. Hypertension 47:371–376. doi:10.1161/01.HYP.0000202052.25238.68
Kawada H, Sumimoto T, Okayama H, Hiwada K (2001) Structure and function of the ventricle and carotid artery in hemodialysis patients. Hypertens Res 24:221–227. doi:10.1291/hypres.24.221
Makita S, Nakamura M, Hiramori K (2005) The association of C-reactive protein levels with carotid intima-media complex thickness and plaque formation in the general population. Stroke 36:2138–2142. doi:10.1161/01.STR.0000181740.74005.ee
London GM, Marchais SJ, Guerin AP, Metivier F, Adda H, Pannier B (2003) Inflammation, arteriosclerosis, and cardiovascular therapy in hemodialysis patients. Kidney Int Suppl 84:S88–S93. doi:10.1046/j.1523-1755.63.s84.25.x
Tseke P, Grapsa E, Stamatelopoulos K et al (2006) Atherosclerotic risk factors and carotid stiffness in elderly asymptomatic HD patients. Int Urol Nephrol 38:801–809. doi:10.1007/s11255-006-9000-1
Kobayashi S, Okada K, Koide H et al (1997) Subcortical silent brain infarction as a risk for clinical stroke. Stroke 28:1932–1939
Fisher CM (1982) Lacunar strokes and infarcts. Rev Neurol 32:871–976
Nakatani T, Naganuma T, Uchida J et al (2003) Silent cerebral infarction in hemodialysis patients. Am J Nephrol 23:86–90. doi:10.1159/000068034
Naganuma T, Uchida J, Tsuchida K et al (2005) Silent cerebral infarction predicts vascular events in hemodialysis patients. Kidney Int 67:2434–2439. doi:10.1111/j.1523-1755.2005.00351.x
Kanters SD, Elgersma OE, Banga JD, van Leeuwen MS, Algra A (1998) Reproducibility of measurements of intima-media thickness and distensibility in the common carotid artery. Eur J Vasc Endovasc Surg 16:28–35. doi:10.1016/S1078-5884(98)80088-9
Dart AM, Gatzka CD, Kingwell BA et al (2006) Brachial blood pressure but not carotid arterial waveforms predict cardiovascular events in elderly female hypertensives. Hypertension 47:785–790. doi:10.1161/01.HYP.0000209340.33592.50
Karaman O, Albayrak R, Colbay M et al (2008) Carotid hemodynamic parameters in hemodialysis patients. Int Urol Nephrol 40:779–784. doi:10.1007/s11255-007-9314-7
Acknowledgements
The study was supported by grants from the Japan Research Promotion Society for Cardiovascular Diseases and Educational Institute for Integrated Medical Sciences (IREIIMS).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ogawa, T., Shimada, M., Ishida, H. et al. Relation of stiffness parameter β to carotid arteriosclerosis and silent cerebral infarction in patients on chronic hemodialysis. Int Urol Nephrol 41, 739–745 (2009). https://doi.org/10.1007/s11255-009-9526-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-009-9526-0