Abstract
In this case report, the procedure of penis replanting and its complications after genital self-mutilation in a male adult are explained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic amputation of the penis is an infrequent injury. The most common cause of injury is genital self-mutilation in men with psychiatric disorders [1]. The current standard of treatment for this infrequent injury is replantation with approximation of the urethra, corporal bodies, and microsurgical dorsal vein, artery and nerve anastomosis [2]. In this case, replantation of a self-amputated penis is reported.
Material method
A 32-year-old man with a history of schizoaffective personality disorder was admitted because of a self-inflicted traumatic amputation of his penis. The penis was amputated using a bread knife. After the patient had cut off his penis and informed his family about it, his father wrapped it immediately with snow (1230) and delivered him urgently to Aksaray State Hospital. Aksaray State Hospital made the first intervention (1330) and got the bleeding under control. A complete amputation of penis at the proximal one third with bleeding vessels was found. The amputated penis was placed, wrapped with a surgical gauze immersed with serum physiologic, between two ice packs after the family’s referral to emergency at the Aksaray State Hospital and preserved 5 h in the ice bag.
The patient was brought to the emergency department of University Hospital and the operation started about 6 h after the trauma (Fig. 1). Before replantation, a suprapubic cystostomy was performed. The urethra was reapproximated with a two-layer closure over a 16-Fr Foley catheter using 5–0 polyglycolic acid, followed by anastomosis of the corporeal bodies with 3–0 polyglycolic acid. The dorsal vein, artery, and nerve were anastomosed with a microsurgical technique (×5 magnification) using 8–0 Prolene suture. Foley catheter was removed during the operation. Buck’s and dartos fascia were reapproximated, and the skin was closed (Fig. 2).
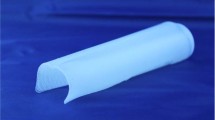
Normal micturition was acquired on the fifth day, and the cystostomy tube was removed on the seventh day after the operation. The amputated penis healed almost completely, except for skin necrosis, 3 weeks after the operation. A skin graft was used to cover the penile shaft 8 weeks postoperatively (Figs. 3, 4). A split-thickness skin graft was harvested by pneumatic dermatome from the left posterolateral thigh. The posterolateral thigh was the preferred donor site because the skin is thicker than that of the medial thigh and allows better reepithelialization [3]. Graft length was determined by measuring shaft circumference penile surface and adding an additional 3-cm overlap. Graft thickness was 0.012–0.016 in. Meshing was performed in a 1:1 ratio, and grafts were applied without stretching apart the meshed slits. Neither urethral stricture nor fistula development occurred. However, erection was not acquired by the patient again.
Discussion
Penile amputation injuries were categorized into three groups by Jezior et al. [4] as: self-inflicted injuries, amputations from felonious assault, and injuries due to accidental trauma. The most common cause of injury is the underlying diagnosis of schizophrenia and the act of self-mutilation under the influence of hallucinations and delusions [5]. Similarly, our patient suffered from schizoaffective personality disorder.
Treatment of penile amputation takes three basic forms: surgical replantation of the amputated penis, tailoring of the remaining penile stump, or total phallic replacement. Replanting the amputated segment is recommended in all cases, as it is the only method likely to yield the most physiologically appropriate result. It depends, however, on the viability of the penis and the condition of the graft bed or penile stump at the time of the injury [4]. We preferred a multidisciplinary approach, as in penile replantation, the anastomosis of vascular neurological cavernosal tissue has to be conducted by experienced surgeons from different disciplines at each level using a microscope. In our case, the penis was prepared correctly, and it took only 6 h until the operation. In such cases, the amputated parts are to be wrapped in saline-soaked gauze and placed in a sterile bag, ensuring that the ice is not in direct contact with the penile skin. The bag and the protected penis are to be placed in a second ice-slush bag to maintain hypothermic conditions until completion of the replantation process [6].
Replanting the penis using microsurgery techniques for the connection of the vessels and nerves enables preservation of sensation in the organ, physiologic miction, and sexual function [2]. In such cases, excessive skin loss is among the common complications. In the case reported here, skin loss in the genital area was corrected through wrapping up the penile shaft with the skin graft. Another common complication in replanting a penis is the development of urethral stricture or fistula. In this case, the urethral catheter was removed after the replanting process was performed. There were no urethral stricture indications after a 9-month follow-up. Within these 9 months the patient suffered from erectile dysfunction, but in line with the relevant literature, there was recovery in the patient after 12 months [7]. Although erectile function and the ability for intromission remained intact in most cases reported so far, in our case, despite the use of microsurgery, it could not be reestablished. The underlying reason for this might be the antipsychopathic drugs that the patient has been using, the erection quality of the patient before the injury, and our operation technique.
Conclusion
Male genital self-mutilation is among the traumas rarely encountered. In cases of penile amputations, the amputated part should be preserved as recommended and the replantation process performed as soon as possible. A multidisciplinary approach with microsurgical replantation is the treatment of choice for the management of penile amputation.
Reference
Greilsheimer H, Groves JE (1979) Male genital self-mutilation. Arch Gen Psychiatry 36:441
Darewicz B, Galek L, Darewicz J, Kudelski J, Malczyk E (2001) Successful microsurgical replantation of an amputated penis. Int Urol Nephrol 33:385–386
Black PC, Friedrich JB, Engrav LH, Wessells H (2004) Meshed unexpanded split-thickness skin grafting for reconstruction of penile skin loss. J Urol 172(3):976–979
Jezior JR, Brady JD, Schlossberg SM (2001) Management of penile amputation injuries world. J Surg 25:1602–1609
Stunell H, Power RE, Floyd M, Quınlan DM (2006) Genital self-mutilation. Int J Urol 13: 1358–1360
Hayhurst SW, O’Brien BM, Ishida H (1974) Experimental digital replantation after prolonged cooling. Hand 6:134–141
Szasz G, McLoughlin MG, Warren RJ (1990) Return of sexual functioning following penile replant surgery. Arch Sex Behav 19:343–348
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ozturk, A., Kilinc, M., Guven, S. et al. Penis replantation after self-mutilation. Int Urol Nephrol 41, 109–111 (2009). https://doi.org/10.1007/s11255-008-9374-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-008-9374-3