Abstract
Food-borne bacterial infections have worldwide importance, and a great variety of antibiotic resistance mechanisms, mainly of the chromosome type, have rapidly developed. Antimicrobial resistance was determined in this study in terms of the presence of extended-spectrum β-lactamases (ESBLs), plasmid AmpC β-lactamases (pAmpC), and plasmid-mediated quinolone resistance (PMQR) from 155 Escherichia coli isolates obtained from bovine carcasses from two states in Mexico (states of Mexico and Jalisco). Isolates were challenged with β-lactam antimicrobials (ampicillin, ceftazidime, and cefotaxime) and quinolones (nalidixic acid and ciprofloxacin). The presence of the bla TEM, bla SHV, bla CTX-M, bla OXA , bla CMY, bla MOX, bla LAT, bla BIL, qnrA, qnrB, qnrS, aac(6′)-Ib-cr, and qepA genes was examined by PCR. Clonal relationship was determined using pulsed-field gel electrophoresis (PFGE). The highest resistance was found to be to nalidixic acid (64 %), followed by ampicillin (32 %), ciprofloxacin (10 %), and ceftazidime and cefotaxime (both 1.3 %). bla CMY (n = 1), bla TEM (n = 24), qnrB (n = 9), and qnrS (n = 7) genes were detected. PFGE analysis showed that the majority of isolates had a different genotypic profile. To our knowledge, this is the first report of the presence of the qnrB, qnrS, and bla CMY genes in E. coli isolated from bovine meat in Mexico.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Escherichia coli causes intestinal and extraintestinal infections due to harboring of various adherence and virulence factors (Bok et al. 2015). A large part of these infections is treated with β-lactam and quinolone antimicrobials, which are considered critical in human medicine by the World Health Organization. Nevertheless, their widespread use in the health sector, as well as their inadequate use in veterinary medicine, has put their usefulness at risk due to the spread of microorganisms that are resistant to these antibiotics (Collignon et al. 2009; Acar and Moulin 2013).
The presence of infections caused by E. coli resistant to β-lactam antimicrobials such as extended-spectrum cephalosporins and quinolones has reached very high levels (Poirel et al. 2012; Seiffert et al. 2013). The main resistance mechanism to these antimicrobials is generated through β-lactamase enzymes of which the extended-spectrum β-lactamases (ESBLs) of the TEM, SHV, and CTX-M families, as well as plasmid AmpC β-lactamases, are noteworthy. Both types of β-lactamases provide resistance to cephalosporins such as ceftazidime and cefotaxime, albeit they are different in that ESBLs are inactivated by β-lactamase inhibitors such as clavulanate, sulbactam, or tazobactam while plasmid AmpC β-lactamases (pAmpC) are resistant to these inhibitors (Seiffert et al. 2013).
Furthermore, resistance to quinolones has increased during the last two decades in E. coli isolates obtained from human patients and hospital facilities, as well as from animal-origin isolates. Although the main mechanisms of resistance to quinolones are coded in the chromosome, plasmid-mediated quinolone resistance (PMQR) has been reported since 1998. These include the Qnr proteins, acetyltransferase aminoglycoside enzyme (AAC(6′)-Ib-cr), or the QepA efflux pump, which, although they provide low-level resistance to quinolones, they are a favorable start for the selection of additional resistance mechanisms. The increase in resistance to β-lactam and quinolone antimicrobials is possibly due to their widespread use in human and veterinary medicine (Poirel et al. 2012).
Apart from the acquisition of resistance genes, the interchange of E. coli isolates between humans and animals destined for human consumption is very important because the latter can act as reservoirs of isolates resistant to antimicrobials and cause disease in humans (Egervärn et al. 2014; Fortini et al. 2011).
In Mexico, the presence of the bla SHV and bla CTX-M ESBL coding genes has been reported from hospital infections. Furthermore, the qnr A, B, and S; aac(6′)-Ib-cr; and qepA genes have also been reported. All these genes for antimicrobial resistance have been identified in various genera of the Enterobacteriaceae family isolated mainly in hospitals for humans throughout the country (Garza-González et al. 2011; Silva-Sánchez et al. 2013).
In contrast, little is known in Mexico on the presence of these resistance genes in animal-origin or meat product isolates. Only a single study has demonstrated the presence of pAmpC bla CMY-2 in animal-origin Salmonella enterica serovar Typhimurium isolates (Zaidi et al. 2007). The objective of this study was to examine the presence of ESBL/pAmpC and PMQR determinants in E. coli isolates from bovine meat of two states in Mexico.
Materials and methods
Bacterial isolates
A total of 155 E. coli isolates were collected from two Republic Mexican states, 75 isolates originated from the State of Mexico: 56 were from bovine carcasses in municipal slaughterhouses, 12 from food processing plants, and 7 from minced meat in butcher’s shops (3-month sampling duration, once each month). Eighty bovine carcass isolates in municipal slaughterhouses in Jalisco (10-month duration) were collected. All samples collected from 2009 to 2012 came from fattened beef calves reared in each state. Carcass and colon samples were taken; approximately 1 g of feces was taken directly from the colon and was placed in an assay tube with 9 ml of 1 % peptonate water. Carcass samples were taken after carcass washing and before refrigeration using a sterile cotton swab moistened with 0.1 % NaCl at 0.85 %; afterwards, each swab was placed in a Falcon-type tube with 25 ml of 1 % peptonate water (European Commission 2001). Samples were transported under refrigeration until their arrival to the laboratory. All samples were incubated for 24 h at 37 °C.
Isolates were inoculated into MacConkey agar plates; a single colony from each plate was selected, subjected to conventional biochemical tests, and confirmed by PCR using primers UAL1939b 5′-ATGGAATTTCGCCGATTTTGC-3′ and UAL2105b 5′-ATTGTTTGCCTCCCTGCTGC-3′ to identify the uidA gene that codes for the β-glucuronidase enzyme (Heijnen and Medema 2006).
Antimicrobial susceptibility testing
The test was carried out using the disk diffusion method on Mueller-Hinton agar, according to the guidelines of the Clinical and Laboratory Standards Institute (CLSI 2012a). The following antimicrobials were used: ampicillin 10 μg (AMP), ceftazidime 30 μg (CAZ), cefotaxime 30 μg (CTX), nalidixic acid 30 μg (NAL), and ciprofloxacin 5 μg (CIP). Isolates resistant to β-lactam antimicrobials were subjected to a ESBL confirmatory test using cefotaxime and ceftazidime on their own and in association with 10 μg clavulanic acid (CLA), as described by CLSI (2012b). The ATCC 25922 E. coli strain was used as control.
Detection of antimicrobial resistance genes
All isolates were tested using PCR in order to detect the bla TEM, bla SHV, bla CTX-M, bla OXA , bla CMY, bla MOX, bla LAT, and bla BIL genes using the previously mentioned primers (Table 1) (Dallenne et al. 2010). In order to determine the presence of the qnrA, qnrB, and qnrS genes, a multiplex PCR was used followed by an end-point PCR. The aac(6′)-Ib-cr and qepA genes were analyzed using primers specific to each gene (Table 1) (Cattoir et al. 2007; Park et al. 2006; Yamane et al. 2007).
Pulsed-field gel electrophoresis
The clonal relationship of the strains which were resistant to CAZ, CTX, and CIP was carried out using pulsed-field gel electrophoresis (PFGE) of samples digested with the XbaI restriction enzyme in agarose following the standardized protocol of the Centers for Disease Control and Prevention, Atlanta, GA (Hunter et al. 2005). Electrophoresis was carried out using a CHEF-DRII chamber. Band patterns were analyzed using the NTSYSpc version 2.2 software while the relationships among genotypes were determined using the unweighted pair group method with arithmetic mean (UPGMA) and band similitude was calculated using Dice’s coefficient.
Statistical analysis
The significant differences (P < 0.05) in the gene presence and the sample origin were assessed by the chi-square test and Yates’s correction using SPSS for Windows ver. 20.0 (SPSS, Chicago, IL).
Results
Of the 155 E. coli isolates confirmed by biochemical tests and the presence of the uidA gene, 64 % (99/155) were resistant, 6 % (9/155) were intermediately resistant, and 30 % (47/155) were susceptible to NAL. Nevertheless, in the case of CIP, 88 % (135/155) of isolates were susceptible, 2 % (3/155) were intermediately resistant, and 10 % (16/155) were resistant. In terms of AMP, 65 % (100/155) were susceptible, 3 % (5/155) were intermediately resistant, and 32 % (50/155) were resistant. Only two isolates (1.3 %) showed resistance to CAZ and CTX, while the rest (98.7 %, 153) were susceptible. The confirmatory test for determining ESBLs in these two isolates showed a different pattern to that established by CLSI since they were resistant to CAZ, CTX, and their combination with CLA.
The bla TEM gene was present in 48 % (24/50) of the isolates resistant to AMP. Of the two isolates suspected of producing the AmpC β-lactamase, only one had the bla CMY gene while for the other, the gene that provided β-lactam antibiotic resistance, could not be determined (Table 2). Up to 5 % (5/100) of the isolates phenotypically susceptible to AMP had the bla TEM gene, while none of the intermediately resistant isolates had this gene. All isolates that had the bla TEM gene were phenotypically susceptible to CAZ and CTX.
In terms of resistance to quinolones, we found that 10 % (16/155) of the isolates had some of the qnr genes, 9 isolates had the qnrB gene, and 7 had the qnrS gene, while no isolate had the qnrA gene. Up to 87.5 % (14/16) of the isolates that had a qnr gene were phenotypically susceptible to CIP, and only 12.5 % (2/16) of the isolates that also had the qnrS gene were resistant to this antimicrobial. Furthermore, only 31 % (5/16) of the isolates had both the qnr and the bla TEM gene. The aac(6′)-Ib-cr and qepA genes were not detected (Table 2).
Isolates showed an almost equal distribution of the bla TEM gene among both states, 52 % (15/29) of the isolates that carried the gene came from the State of Mexico, while the remaining 48 % (14/29) came from Jalisco. Also, 55 % (5/9) of isolates carrying the qnrB gene were from the State of Mexico, while 44 % (4/9) came from Jalisco. In contrast, 86 % of the isolates positive to the qnrS gene came from the State of Mexico and only 14 % (1/7) from Jalisco. The single isolate with the bla CMY gene came from the State of Jalisco (Table 3).
PFGE
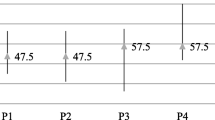
A total of 18 isolates with intermediate sensitivity and resistant to CIP, CAZ, and CTX were selected from the 155 isolates in order to obtain their genetic profiles using the PFGE technique from which a dendrogram was constructed (Fig. 1) that shows the phylogenetic relationship among isolates. The presence of two distinct clades with a <70 % similitude between them can be observed in Fig. 1, one composed of a single isolate (isolate 147) from Jalisco and the other encompassing the remaining isolates (17) from the states of Mexico and Jalisco. Within the largest clade, two isolates were found to be closely related between them (isolates 4 and 15 from municipal slaughterhouses in the State of Mexico) that were resistant to CIP and had a 100 % similitude coefficient, which suggests that they had clonal relationship.
Discussion
In this study, resistance of up to 64 % to NAL and 10 % to CIP was found, which contrasts with the results obtained in a Polish study in which they found resistance of up to 1.3 for norfloxacin in E. coli isolates from cattle. This study also found resistance to AMP of up to 32 %, while for CAZ and CTX, it reached 1.3 %. The aforementioned authors reported resistance of 3.9 % for AMP and 3.4 % for CAZ (Mazurek et al. 2013). Another study in the USA, which included E. coli isolates obtained from beef, reported resistance levels to AMP of 6.0 %, CIP of 0 %, and NAL of 0.8 % (Zhao et al. 2012). A German study found that isolates obtained from bull calves showed up to 59 % resistance to AMP, 3 % to CAZ, 1.4 % to CTX, 10.5 % to NAL, and 13.3 % to CIP (Kaesbohrer et al. 2012). Lastly, a study carried out in France found resistance levels of up to 61 % to amoxicillin, 1.0 % to CTX, 0 % to CAZ, 14.7 % to NAL, and 5.4 % to enrofloxacin (Haenni et al. 2014). In general, the results in this study showed resistance levels to antimicrobials that were similar, and sometimes higher for some of them, when compared to those found in the aforementioned countries. Such increase in resistance has also been observed in studies carried out with human-origin E. coli isolates in Mexico. Amábile-Cuevas (2010) reported resistance levels of up to 74 % for AMP, 33 % for CIP, and 8 % for CAZ, which could suggest the spread of clones or antimicrobial resistance mechanisms between the human and animal populations in our country.
To our knowledge, this is the first report of E. coli isolates collected from bovine meat samples that have the bla CMY gene, as well as the first report of the presence of the qnrB and qnrS genes in animal-origin isolates in Mexico. This finding highlights the possibility that isolates that are carriers of these resistance mechanisms decrease the efficacy of antimicrobials used in humans as they become less effective for fighting infections placing public health at risk.
The presence of the bla CMY gene agrees with a study carried out in Mexico with Salmonella Typhimurium that found that it was the only gene present that provided resistance to cephalosporins, which in turn suggests the wide distribution of the gene within isolates of different origins in our country (Zaidi et al. 2007). In North America, the presence of the bla CMY gene, specifically the bla CMY-2 variant, is relatively common, although the plasmid AmpC β-lactamase is more widespread as it is found in isolates from samples of poultry, pig, and cattle (Doi et al. 2010; Glenn et al. 2012; Mollenkopf et al. 2011).
The bla TEM gene was present in almost half of the isolates resistant to AMP. Nevertheless, 52 % (26/50) of the isolates resistant to AMP did not have this gene. This suggests that there is another gene that is responsible for phenotypic resistance, such as the bla PSE-1 gene, whose presence has been reported in Salmonella spp. isolates in Mexico (Varela-Guerrero et al. 2013).
This study showed a relatively low frequency of bovine-origin isolates that contained the bla CMY gene when compared to other animal species (Zaidi et al. 2007). This could be related to animal production practices, as well as to the quantity and class of antimicrobials used in comparison to swine and poultry farms (EMA 2012). Nevertheless, the fact that an E. coli isolate that had the bla CMY gene was found suggests that such gene could spread in the following years within animal populations and meat products in a similar fashion as what is observed in isolates from Salmonella spp. in Mexico (Zaidi et al. 2007).
In regard to the resistance to quinolones, 16 isolates were found that had qnr genes. Studies carried out in other countries also using E. coli which were obtained from cattle show a lower number of positive isolates. This could reflect that in Mexico, there is a wider spread of this gene in bovine-origin isolates. For example, two studies carried out in Europe with E. coli isolates from cattle just found one positive qnrS gene in each, respectively (Kirchner et al. 2011; Veldman et al. 2011). Notwithstanding, 87.5 % (14/16) of the isolate carriers of a qnr gene were susceptible to ciprofloxacin, confirming that these genes only slightly increase their resistance to such antibiotics, and they are classified as susceptible under the CLSI criteria making them pass unnoticed. Nevertheless, it has been reported that the presence of qnr genes favors the acquisition of other mechanisms of resistance to quinolones (Poirel et al. 2012).
The PFGE analysis showed that the majority of the isolates had differing genotypic profiles. Both clades formed did not show particular similitudes which would group isolates by state of origin, with the exception of the two isolates that had similar banding patterns suggesting the same clonal origin at the local level. Nevertheless, cross-contamination during processing in an abattoir cannot be ruled out.
This study evidences the fact that the detection of these antimicrobial resistance genes in animal-origin isolates constitutes a warning of the risk and the lack of limiting and control of antimicrobial treatments used in veterinary medicine represents, as well as their possible transmission through the food chain, especially in meat products. In Mexico, restrictions have been placed upon the sale of antimicrobials. Nevertheless, such measures only apply to pharmaceuticals for human use excluding those used in veterinary medicine. As such, their prophylactic application or as growth promoters could contribute to an increase in antimicrobial resistance levels as years go by. Furthermore, it is evident that further epidemiological studies are needed on the presence of β-lactamase and PMQR determinants in animal-origin isolates in order to determine if these resistance mechanisms are spreading, as well as allow the establishment of mechanisms that counter antimicrobial resistance.
References
Acar JF. and Moulin G. 2013. Integrating animal health surveillance and food safety: the issue of antimicrobial resistance. Revue scientifique et technique (International Office of Epizootics), 32(2):383–92.
Amábile-Cuevas C. 2010. Antibiotic resistance in Mexico: a brief overview of the current status and its causes. The Journal of Infection in Developing Countries, 4(3):126–131.
Bok E., Mazurek J., Stosik M., Wojciech M., Baldy-Chudzik K. 2015. Prevalence of virulence determinants and antimicrobial resistance among commensal Escherichia coli derived from dairy and beef cattle. International Journal of Environmental Research and Public Health, 12(1):970–85.
Cattoir V., Poirel L., Rotimi V., Soussy CJ., Nordmann P. 2007. Multiplex PCR for detection of plasmid-mediated quinolone resistance qnr genes in ESBL-producing enterobacterial isolates. Journal of Antimicrobial Chemotherapy, 60(2):394–397.
CLSI. Clinical and Laboratory Standard Institute. 2012a. Performance Standards for Antimicrobial Disk Susceptibility Tests, 19th edition, Approved Standard M02-A11. Wayne, PA.
CLSI. Clinical and Laboratory Standard Institute. 2012b. Performance Standards for Antimicrobial Susceptibility Testing, 22nd informational supplement. M100-S22. Wayne, PA.
Collignon P., Powers JH., Chiller TM., Aidara-Kane A., Aarestrup FM. 2009. World Health Organization ranking of antimicrobials according to their importance in human medicine: A critical step for developing risk management strategies for the use of antimicrobials in food production animals. Clinical Infectious Diseases, 49(1):132–141.
Dallenne C., Da Costa A., Decré D., Favier C., Arlet G. 2010. Development of a set of multiplex PCR assays for the detection of genes encoding important β-lactamases in Enterobacteriaceae. Journal of Antimicrobial Chemotherapy, 65(3):490–495.
Doi Y., Paterson DL., Egea P., Pascual A., López-Cerero L., Navarro MD., Adams-Haduch JM., Qureshi ZA., Sidjabat HE., Rodríguez-Baño J. 2010. Extended-spectrum and CMY-type β-lactamase-producing Escherichia coli in clinical samples and retail meat from Pittsburgh, USA and Seville, Spain. Clinical Microbiology and Infection, 16(1):33–38.
Egervärn M., Börjesson S., Byfors S., Finn M., Kaipe C., Englund S., Lindblad M. 2014. Escherichia coli with extended-spectrum beta-lactamases or transferable AmpC beta-lactamases and Salmonella on meat imported into Sweden. International Journal of Food Microbiology, 171:8–14.
EMA. European Medicines Agency. Second ESVAC Report 2012. European Surveillance of Veterinary Antimicrobial Consumption Report (ESVAC). Sales of Veterinary Antimicrobial Agents in 19 EU/EEA Countries in 2010. http://www.ema.europa.eu/docs/ en_GB/document_library/Report/2012/10/WC500133532.pdf
European Commission. 2001. European Directive 2001/471/EC, Official Journal of the European Communities, L165, 48–53.
Fortini D., Fashae K., García-Fernández A., Villa L., Carattoli A. 2011. Plasmid-mediated quinolone resistance and β-lactamases in Escherichia coli from healthy animals from Nigeria. Journal of Antimicrobial Chemotherapy, 66(6):1269–72.
Garza-González E., Mendoza-Ibarra SI., Llaca-Díaz JM., González GM. 2011. Molecular characterization and antimicrobial susceptibility of extended-spectrum β-lactamase producing Enterobacteriaceae isolates at a tertiary-care center in Monterrey, Mexico. Journal of Medical Microbiology, 60(Pt 1):84–90.
Glenn LM., Englen MD., Lindsey RL., Frank JF., Turpin JE., Berrang ME., Meinersmann RJ., Fedorka-Cray PJ., Frye JG. 2012. Analysis of antimicrobial resistance genes detected in multiple-drug-resistant Escherichia coli isolates from broiler chicken carcasses. Microbial Drug Resistance, 18(4):453–463.
Haenni M., Châtre P., Métayer V., Bour M., Signol E., Madec JY., Gay E. (2014): Comparative prevalence and characterization of ESBL-producing Enterobacteriaceae in dominant versus subdominant enteric flora in veal calves at slaughterhouse, France. Veterinary Microbiology. pii: S0378-1135(14)00113-8. doi: 10.1016/j.vetmic.2014.02.023.
Heijnen L. and Medema G. 2006. Quantitative detection of E. coli, E. coli O157 and other Shiga toxin producing E. coli in water samples using a culture method combined with real-time PCR. Journal of Water and Health, 4: 487–498.
Hunter SB., Vauterin P., Lambert-Fair MA., Van Duyne MS., Kubota K., Graves L., Wrigley D., Barrett T., Ribot E. 2005. Establishment of a universal size standard strain for use with the PulseNet standardized pulsed-field gel electrophoresis protocols: converting the national databases to the new size standard. Journal of Clinical Microbiology, 43:1045–1050.
Kaesbohrer A., Schroeter A., Tenhagen BA., Alt K., Guerra B., Appel B. 2012. Emerging antimicrobial resistance in commensal Escherichia coli with public health relevance. Zoonoses and Public Health, 59 Suppl 2:158–165.
Kirchner M., Wearing H., Teale C. 2011. Plasmid-mediated quinolone resistance gene detected in Escherichia coli from cattle. Veterinary Microbiology, 148(2–4):434–435.
Mazurek J., Pusz P., Bok E., Stosik M., Baldy-Chudzik K. 2013. The phenotypic and genotypic characteristics of antibiotic resistance in Escherichia coli populations isolated from farm animals with different exposure to antimicrobial agents. Polish Journal of Microbiology, 62(2):173–9.
Mollenkopf DF., Kleinhenz KE., Funk JA., Gebreyes WA., Wittum TE. 2011. Salmonella enterica and Escherichia coli harboring bla CMY in retail beef and pork products. Foodborne Pathogens and Disease, 8(2):333–336.
Park CH., Robicsek A., Jacoby GA., Sahm D., Hooper DC 2006. Prevalence in the United States of aac(6′)-Ib-cr encoding a ciprofloxacin-modifying enzyme. Antimicrobial Agents and Chemotherapy, 50(11):3953–3955.
Poirel L., Cattoir V., Nordmann P. 2012. Plasmid Mediated Quinolone Resistance; Interactions between Human, Animal, and Environmental Ecologies. Frontiers in Microbiology, 3:24. doi: 10.3389/fmicb.2012.00024.
Seiffert SN., Hilty M., Perreten V., Endimiani A. 2013. Extended-spectrum cephalosporin-resistant Gram-negative organisms in livestock: an emerging problem for human health?. Drug Resistance Updates, 16(1–2):22–45.
Silva-Sánchez J., Cruz-Trujillo E., Barrios H., Reyna-Flores F., Sánchez-Pérez A; Bacterial Resistance Consortium, Garza-Ramos U. 2013. Characterization of plasmid-mediated quinolone resistance (PMQR) genes in extended-spectrum β-lactamase-producing Enterobacteriaceae pediatric clinical isolates in Mexico. PLoS One, 8(10):e77968. doi: 10.1371/journal.pone.0077968.
Varela-Guerrero JA., Talavera-Rojas M., Gutiérrez-Castillo A del C., Reyes-Rodríguez NE., Vázquez-Guadarrama J. 2013. Phenotypic-genotypic resistance in Salmonella spp. isolated from cattle carcasses from the north central zone of the State of Mexico. Tropical Animal Health and Production, 45(4):995–1000.
Veldman K., Cavaco LM., Mevius D., Battisti A., Franco A., Botteldoorn N., Bruneau M., Perrin-Guyomard A., Cerny T., De Frutos Escobar C., Guerra B., Schroeter A., Gutierrez M., Hopkins K., Myllyniemi AL., Sunde M., Wasyl D., Aarestrup FM. 2011. International collaborative study on the occurrence of plasmid-mediated quinolone resistance in Salmonella enterica and Escherichia coli isolated from animals, humans, food and the environment in 13 European countries. Journal of Antimicrobial Chemotherapy, 66(6):1278–1286.
Yamane K., Wachino J., Suzuki S., Kimura K., Shibata N., Kato H., Shibayama K., Konda T., Arakawa Y. 2007. New plasmid-mediated fluoroquinolone efflux pump, QepA, found in an Escherichia coli clinical isolate. Antimicrobial Agents and Chemotherapy, 51(9):3354–3360.
Zaidi MB., Leon V., Canche C., Perez C., Zhao S., Hubert SK., Abbott J., Blickenstaff K., McDermott PF. 2007. Rapid and widespread dissemination of multidrug-resistant bla CMY-2 Salmonella Typhimurium in Mexico. Journal of Antimicrobial Chemotherapy, 60(2):398–401.
Zhao S., Blickenstaff K., Bodeis-Jones S., Gaines SA., Tong E., McDermott PF. 2012. Comparison of the prevalences and antimicrobial resistances of Escherichia coli isolates from different retail meats in the United States, 2002 to 2008. Applied and Environmental Microbiology, 78(6):1701–1707.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aguilar-Montes de Oca, S., Talavera-Rojas, M., Soriano-Vargas, E. et al. Determination of extended spectrum β-lactamases/AmpC β-lactamases and plasmid-mediated quinolone resistance in Escherichia coli isolates obtained from bovine carcasses in Mexico. Trop Anim Health Prod 47, 975–981 (2015). https://doi.org/10.1007/s11250-015-0818-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11250-015-0818-3