Abstract
Given the paucity of comparative efficacy data and the difference in cost between andexanet-alfa and prothrombin complex concentrates (PCC), debates continue regarding optimal cost-effective therapy for patients who present with major bleeding associated with oral factor Xa inhibitors. Available literature comparing the cost-effectiveness of the reversal agents is limited, and the large difference in price between therapy options has led many health systems to exclude andexanet-alfa from their formularies. To evaluate the clinical outcomes and cost of PCC compared to andexanet-alfa for patients with factor Xa inhibitor associated bleeds. We performed a quasi-experimental, single health system study of patients treated with PCC or andexanet-alfa from March 2014 to April 2021. Deterioration-free discharge, thrombotic events, length of stay, discharge disposition, and cost were reported. 170 patients were included in the PCC group and 170 patients were included in the andexanet-alfa group. Deterioration-free discharge was achieved in 66.5% of PCC-treated patients compared to 69.4% in the andexanet alfa-treated patients. 31.8% of PCC-treated patients were discharged home compared to 30.6% in the andexanet alfa-treated patients. The cost per deterioration-free discharge was $20,773.62 versus $5230.32 in the andexanet alfa and 4 F-PCC group, respectively. Among patients that experienced a bleed while taking a factor Xa inhibitor, there was no difference in clinical outcomes for patients treated with andexanet-alfa compared to PCC. Although there was no difference in the clinical outcomes, there was a significant difference in cost with andexanet-alfa costing approximately four times as much as PCC per deterioration-free discharge.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Highlights
-
The available literature comparing the cost-effectiveness of andexanet-alfa and PCC is limited.
-
This study took place at a single health system in southeast Michigan comprised of 5 hospitals.
-
Cost per deterioration-free discharge was $20,773.62 for andexanet-alfa and $5230.32 for PCC.
-
There were no significant differences in the clinical outcomes that were assessed.
Introduction
The use of oral factor Xa inhibitors has continued to increase for the prevention of stroke in patients with atrial fibrillation (AF) and treatment of venous thromboembolism (VTE). Due to the inhibition of clotting factor Xa, patients taking these medications are at an increased risk of bleeding. However, there is still debate about optimal cost-effective management of bleeding events associated with factor Xa inhibitors.
In May 2018, andexanet-alfa (Andexxa®) was approved by the U.S Food and Drug Administration (FDA) for the reversal of life-threatening or uncontrolled bleeding for patients treated with rivaroxaban (Xarelto®) or apixaban (Eliquis®), becoming the first agent with specific reversal activity related to factor Xa [1]. The Annexa-4 study demonstrated that andexanet-alfa was efficacious for achieving “good or excellent” hemostasis in 82% of patients at 12 h. Thrombotic events occurred in 10% of patients, and death occurred within 30 days for 14% of patients [2].
Prior to the approval of andexanet-alfa, major bleeding events associated with rivaroxaban or apixaban were commonly treated with prothrombin complex concentrates (PCC), including activated prothrombin complex concentrate (aPCC) and four factor prothrombin complex concentrate, as recommended by guidelines [3, 4].
Current national guidelines from the American College of Cardiology (ACC) recommend using andexanet-alfa as the first line agent if it is available and using PCC as an alternative if andexanet-alfa is unavailable [5]. The American College of Gastroenterology (ACG) and Canadian Association of Gastroenterology (CAG) also have a collaborative guideline specific to gastrointestinal bleeding. The guideline recommends against andexanet-alfa and PCC for gastrointestinal bleeding with the exception of selective clinical scenarios such as a life-threatening bleed. In the situation of a life-threatening bleed the ACG-CAG does not provide a recommendation for a preferred agent between andexanet-alfa and PCC [6]. Data published to date from the FIX-ICH trial supports the guideline recommendations that PCC are viable treatment options for patients with a factor Xa inhibitor associated bleeds. The results demonstrated similar safety and efficacy to patients treated with andexanet-alfa in the Anexxa-4 study. Good or excellent hemostasis was achieved in 81.8% of patients, thrombotic events occurred in 3.8%, and 19% of patients had in-hospital mortality [7].
Andexanet alfa is an expensive agent (estimated to range from $12,375–$49,500/patient based on the dose and New Technology Add-on Payment (NTAP) reimbursement), and debate continues about the cost-effectiveness of therapy compared to PCC (actual cost ranging from $2430–$8100 depending on the amount of units used) [8].
There is limited available literature comparing the cost-effectiveness of reversal agents used for bleeds associated with factor Xa inhibitors. The large difference in price between the therapy options has led to some health systems excluding andexanet-alfa from their formularies [9].
Most available literature following the Anexxa-4 study assesses hemostasis alone as the primary outcome and includes patients with intracranial hemorrhage [10,11,12]. There are many other outcomes meaningful to patients, providers, and health-systems worthy of consideration when determining whether one reversal agent would be preferred over another.
For the purposes of this study, a novel clinical endpoint, deterioration-free discharge, was developed as a composite outcome to further evaluate clinical outcomes beyond hemostasis alone. The clinical endpoints included administration of additional packed red blood cells, hemoglobin drop after initial achievement of hemostasis, need for additional bleeding-related intervention, requiring escalation of care (i.e. transfer from general practice unit to intensive care unit), or in-hospital mortality that are assessed with this composite endpoint.
This study aimed to fill the gap in literature by including patients that were treated with andexanet-alfa or PCC regardless of the source of bleeding and using real world acquisition costs of reversal agents. In addition to evaluating cost and reimbursement data, clinical outcomes were characterized between the different types of DOAC induced bleeding. We hypothesized that andexanet-alfa would not lead to an increase in the number of positive outcomes that would offset the cost difference between the reversal agents thus, cost per deterioration free discharge would be lower in the PCC group.
Methods
Data collection
This is a single health system, retrospective cohort study based on chart review from March 2014 to April 2021. Andexanet-alfa was added to the health-system formulary in September 2018, leading to an update in system-wide anticoagulation reversal guidelines. Prior to the adoption of andexanet-alfa, the institutional antithrombotic reversal guideline recommended one dose of aPCC 25 units/kg with one additional dose of aPCC 25 units/kg if necessary, for ongoing bleeding, based on provider discretion.
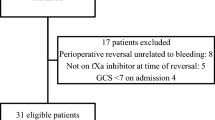
Patients were identified using an electronic health record medication administration history of PCC from March 2014–September 2018 and andexanet-alfa from October 2018–April 2021. Patients were screened in reverse chronological order for the PCC group and chronological order for the andexanet-alfa group to help limit any potential maturation bias. Patients were included if they were 18 years of age or older, taking rivaroxaban, apixaban, betrixaban, or edoxaban, and had a bleeding event that required reversal using PCC prior to September 2018 or andexanet-alfa post September 2018. Patients were excluded if they were pregnant, incarcerated, or if they received PCC prior to andexanet-alfa after September 2018.
Data was collected via retrospective chart review and included patient demographics, the agent and dose of the reversal agent administered, the factor Xa inhibitor the patient was taking prior to the bleeding event including dose, indication, time since last dose, if known, and source of the bleeding. The severity of the bleeding event was assessed using Glasgow Blatchford score for gastrointestinal bleeds and ICH score for patients with intracerebral hemorrhage [13, 14]. SOFA score for patients admitted to an intensive care unit was calculated as an overall predictor of clinical outcomes [15].
Hemostatic efficacy was assessed based on Anexxa-4 rating system for effective hemostasis by analyzing hemoglobin and hematocrit trends for gastrointestinal, genitourinary, and non-visible bleeds, reviewing radiologist reports of head CT impressions for intracranial hemorrhages, and reviewing notes to assess time to cessation of bleeding for visible bleeds [2].
Other data collected to assess clinical outcomes associated with bleeding reversal included the patient care unit the patient was admitted to, the amount of blood products that were administered, documentation of unplanned interventions, and in-hospital mortality.
Additional data that was collected included the NTAP reimbursement that was received for a patient’s admission, the patient’s disposition documented in the discharge note, the time therapeutic anticoagulation was restarted, and the admission and discharge time to and from the hospital, as well as the ICU.
Outcomes
The primary composite outcome was deterioration free discharge which was defined as a hospital course following anticoagulation reversal that achieved hemostasis based on criteria similar to those used in Annexa-4 and did not include any of the following administration of additional packed red blood cells, hemoglobin drop after initial achievement of hemostasis, need for additional bleeding-related intervention, requiring escalation of care, or in-hospital mortality.
Deterioration-free discharge was created as the primary outcome to assess various factors that could correlate with patients having positive outcomes beyond achieving hemostasis, including achieving a stable hemoglobin and not requiring additional transfusion or intervention, not requiring transfer to a unit that provides higher level of care, and survival at hospital discharge. Secondary outcomes included cost per deterioration-free discharge, discharge disposition, hospital and ICU length of stay, and in-hospital thrombotic events.
Cost was assessed using acquisition costs of the reversal agents as of February 2022. NTAP reimbursements that were received by the health system were also included in assessing cost. NTAP is a payment made by Centers of Medicare & Medicaid Services (CMS) to promote patient access for the most up to date treatment options [16]. Cost per deterioration-free discharge was calculated using the total acquisition cost of the reversal agents (with NTAP reimbursement subtracted, if applicable, in the andexanet-alfa group) divided by the number of patients with a deterioration free discharge.
Statistical analysis
Based on hemostasis and mortality results of published literature it was estimated that a 15% difference in the primary outcome would occur between the andexanet alfa and PCC groups [2, 10]. From this assumption, it was estimated that 340 patients would be needed to provide an alpha of 0.05 and power of 0.8.
Descriptive statistics, including numbers of patients, proportions, and measures of central tendency and variability were used to describe the patient population. Categorical variables were compared using Chi-square, and continuous variables were compared using Mann Whitney U as appropriate for the data distribution. Odds ratios and 95% confidence intervals were calculated for subgroups of baseline characteristics. For all analyses, P values < 0.05 were considered statistically significant. All calculations were performed using IBM-SPSS Statistics (Armonk, NY).
Two subgroup analyses were planned a priori; one comparing the two reversal agents in patients with gastrointestinal bleeds and another comparing the reversal agents in patients that experienced an intracranial hemorrhage.
Results
Baseline characteristics
Baseline characteristics were similar between the two study groups with the exception of BMI and race (Table 1). The mean age of participants was 75 years, sex was similarly distributed, and most participants were white (78%). The mean BMI was slightly higher in the PCC group compared to the andexanet-alfa group, 29.6 and 27.8 respectively (p = 0.048).
The characteristics of the factor Xa inhibitor the patient was taking prior to bleeding was also similar between the two groups. More patients were taking apixaban prior to the bleed (66%) and the most common indication was AF (72%). More patients in the PCC group were taking a factor Xa inhibitor for AF (p < 0.001), and there were more patients with an indication for acute VTE in the andexanet-alfa group (p = 0.013).
The source of bleeding was similar between the two groups with 47% presenting with intracranial bleeds, 37% presenting with gastrointestinal bleeds, and 16% presenting with another type of bleeding event (i.e. musculoskeletal, genitourinary, renal, splenic, abdominal, and peritoneal). The severity of the bleeding event using the Glasgow Blatchford score for patients with a gastrointestinal bleed, and ICH score for patients with intracerebral hemorrhage, was also similar between the groups.
There was not a significant difference in concurrent use of antiplatelets, including aspirin, clopidogrel, ticagrelor, and prasugrel, between the two groups. The groups had a similar rate of patients that had previous diagnosis of liver failure, hypertension, alcohol use disorder, and peptic ulcer disease; however more patients in the PCC group had a diagnosis for renal failure, cancer, or anemia.
Patients in the PCC group were mostly treated with aPCC 25 units/kg (n = 149, 87.6%), one patient (0.6%) received aPCC 50 units/kg, eight patients (4.7%) were treated with 4-factor PCC 25 units/kg, and twelve (7.1%) received 4-factor PCC 50 units/kg. In the andexanet-alfa group 28 (16%) patients were treated with high dose (800 mg bolus followed by 8 mg/min infusion up to 120 min) and 142 (84%) received low dose (400 mg bolus followed by 4 mg/min infusion up to 120 min). Based on the factor Xa inhibitor dose and time since last administration it was determined that 18/28 (64%) high dose administrations were appropriate and 127/142 (89%) low dose administrations were appropriate based on manufacturer dosing recommendations.
Deterioration-free discharge
Deterioration-free discharge was achieved in 66.5% of patients who received PCC compared to 69.4% who received andexanet-alfa (p = 0.646) (Table 2.). When comparing PCC and andexanet-alfa there was no significant difference in hemostasis (p = 0.640), administration of additional packed red blood cells (p = 0.146), hemoglobin drop following stabilization (p = 0.176), unplanned bleeding related interventions (p = 0.156), level of care escalation (p = 0.314), or in-hospital mortality (p = 0.448). The odds ratios (95% CI) calculated for baseline characteristic subgroups all included 1, suggesting weak association between these characteristics and deterioration free discharge (Table 3).
Secondary clinical outcomes
In-hospital thrombotic events, hospital length of stay, ICU length of stay, and time to resumption of therapeutic anticoagulation were similar between the two reversal agent groups (Table 3). Therapeutic anticoagulation was restarted during the admission for 64/340 (19%) of patients, 29 treated with PCC and 35 treated with andexanet-alfa. The discharge dispositions were also similar between reversal agent groups, with the most common discharge dispositions being home (31%), skilled nursing facility (18%), and in-hospital mortality (15%) (Figure 1). The average cost per deterioration-free discharge for PCC was $5230.32 compared to $20,773.62 for andexanet-alfa (p < 0 0.001).
ICH subgroup
In this study, 159 patients presented with an intracranial hemorrhage. Eighty (50.3%) were treated with PCC and 79 (49.7%) were treated with andexanet-alfa. Deterioration-free discharge was achieved in 67.5% of patients that received PCC compared to 77% in the andexanet-alfa group (p = 0.399). When comparing PCC and andexanet-alfa there was no significant difference in hemostasis (p = 0.246), in-hospital mortality (p = 0.805), or level of care escalation (p = 0.319). Patients in the ICH subgroup did not have a drop in hemoglobin following the stabilization, require additional administration of blood products, or have any unplanned bleeding-related interventions. The discharge disposition was similar between the groups with 18.8% of patients in the PCC group and 13.9% of patients in the andexanet-alfa group being discharged home (p = 0.411).
The cost per deterioration-free discharge for PCC was $4979.15 compared to $17,925.36 for andexanet-alfa (p < 0 0.001).
GI subgroup
There were 126 patients who presented with a gastrointestinal bleed; 67 (53.2%) were treated with PCC and 59 (46.8%) were treated with andexanet-alfa. Deterioration-free discharge was achieved in 70.1% of patients that received PCC compared to 71.2% in the andexanet-alfa group (p = 0.898). When comparing PCC and andexanet-alfa, there was no significant difference in hemostasis (p = 0.722), in-hospital mortality (p = 0.590), level of care escalation (p = 0.928), administration of additional blood products (p = 0.146), or hemoglobin drop following stabilization (p = 0.251), There were no unplanned bleeding-related interventions performed in the GI subgroup. The discharge disposition was similar between the groups with 46.3% of patients in the PCC group and 49.2% of patients in the andexanet-alfa group being discharged home (p = 0.746).
The cost per deterioration-free discharge for PCC was $5307.65 compared to $18,421.27 for andexanet-alfa (p < 0 0.001).
Discussion
Among patients who experienced a bleeding event while taking a factor Xa inhibitor, there was no difference in deterioration-free discharge in patients treated with andexanet-alfa compared to PCC. Although there was no difference in the clinical outcomes, there was an approximate four-fold higher cost per deterioration-free discharge for andexanet alfa compared to PCC.
Deterioration-free discharge has not been used previously to assess outcomes of factor Xa inhibitor associated bleeding reversal. The outcome was created as a composite primary outcome of variables that have been used in previous studies to assess multiple factors, meaningful to patients and providers, that could be characteristic of positive outcomes, including achieving a stable hemoglobin and not requiring additional transfusion or intervention, not requiring transfer to a unit that provides higher level of care, and survival at hospital discharge. It is important to note that there were no differences in any of the specific outcomes that made up the composite. We also assessed discharge disposition to compare potential quality of life following the hospital course. Assessing hemostasis alone would fail to capture many factors that impact the quality of life of a patient following administration of andexanet-alfa or PCC.
In the andexanet-alfa group of our study, clinical outcomes including hemostasis and death occurred at a similar rate to those seen from the Anexxa-4 study [2]. The PCC arm of the ICH subgroup in our study also had similar hemostasis and in-hospital mortality outcomes to patients in the PCC arm of the FIX-ICH trial [6]. The similar outcomes of our study with these two larger studies adds to the validity that there may not be a difference in clinical outcomes of patients treated with andexanet-alfa or PCC.
Other literature published following the Anexxa-4 study often includes limited sample sizes with patients that have intracranial hemorrhage, evaluating endpoints looking at either clinical outcomes or cost [8, 10,11,12]. This study adds value to the available literature by including patients with a variety of bleeding sites and assessing both clinical outcomes and cost in the same population. The composite endpoint that was used also assesses additional clinical endpoints, beyond achievement of hemostasis, that are meaningful to both health-systems and patients. The results also add further support to the conclusion from a systematic review and meta-analysis performed by Nederpelt and colleagues, that neither reversal agent was significantly associated with increased effectiveness [17].
PCC may be an acceptable alternative to andexanet-alfa for the reversal of DOAC associated gastrointestinal bleeds based on the similar rate of deterioration-free discharge between andexanet-alfa and PCC in the GI subgroup, the lack of a recommendation for a specific agent from the ACG-CAG guidelines, and the significant cost difference between the agents.
The high dose andexanet-alfa was used inappropriately, according to the manufacturer dosing guideline, in 10/28 (36%) patients in our study. Ensuring the appropriate dose of andexanet-alfa would be another way to optimize healthcare spending. High dose was used when the manufacturer dosing guideline would have recommended low dose in a variety of situations. The most common occurrence was when patients were using apixaban 5 mg or less and the last dose was within 8 h or the time since last administration was unknown. The use of low dose instead of high dose andexanet-alfa for these 10 patients would have reduced total acquisition cost of andexanet-alfa by approximately $200,000.
There are limitations to this study. Since patients were included over a period of eight years there is the potential for maturation bias. The clinical advancements in treating DOAC associated bleeds over time could potentially cause more favorable outcomes in the andexanet-alfa group. Another limitation is that this was a retrospective single-system study, so there is a possibility for selection bias from treating providers that would not be easily identifiable on chart review. Selection bias could lead to differences in baseline characteristics between the groups; however, there were no patients included in the PCC group of the study after andexanet-alfa was approved. There was also no difference in SOFA score, ICH score, or Glasgow Blatchford score between the groups. There were differences in other baseline characteristics between the two groups. A majority of the patients in the study were white which is consistent with the prevalence of clinically diagnosed atrial fibrillation reported by the American Heart Association [18]. DOACs were initially FDA approved for A.fib and then later approved for treatment of VTE which could have contributed to more patients with an indication of VTE treatment in the andexanet-alfa group. The patients with an indication of VTE treatment may have been at a higher risk of thrombosis than patients taking a DOAC for atrial fibrillation. The PCC group had more patients with a previous diagnosis for renal failure, cancer, or anemia which could put them at a higher risk for bleed than the patients in the andexanet-alfa group. It should also be noted that the rate of Medicare patients presenting to an institution with an anticoagulant related bleeding event will differ between institutions. Therefore, the influence of NTAP reimbursement on cost in this study may not be fully generalizable to all institutions.
The proportion of patients who received doses of andexanet alfa that did not align with manufacturer dosing recommendations could have also influenced the results of this study. It should also be noted that the analysis of the cost data in this study occurred before an announcement that a significant decrease in the price of andexanet-alfa and changes to the NTAP reimbursements are anticipated. These changes could impact the financial analysis presented within this study, however the cost reduction combined with changes in NTAP reimbursement would need to be reduced nearly 400% to have equivalent cost per deterioration free discharge between the groups, based on our results.
The cost per deterioration free discharge was re-calculated using pricing of the reversal agents as of April 2023, but it is also important to note the NTAP reimbursements received by the institution are expected to be reduced due to the reduced cost of andexanet-alfa. The cost per deterioration free discharge for andexanet-alfa would be $13,786.79 using new pricing and 45% of the NTAP reimbursements received during the study period, assuming the decrease in NTAP reimbursement will be directly proportional to the decrease in andexanet-alfa wholesale acquisition cost [16].
Conclusion
Among patients that experienced a bleeding event while taking a factor Xa inhibitor, there was no difference in deterioration free discharge for patients treated with andexanet-alfa compared to PCC. Although there was no difference in the clinical outcomes, there was a significant difference in cost with andexanet-alfa costing approximately four times as much as PCC per deterioration-free discharge.
References
Andexxa (coagulation factor Xa (recombinant), inactivated-zhzo) (2018) [Highlights of Prescribing Information]. Portola Pharmaceuticals, Inc
Connolly SJ, Crowther M, Eikelboom JW et al (2019) Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med 380:1326–1335
Frontera JA, Lewin JJ, Rabinstein AA, Zerfoss CL et al (2016) Guideline for reversal of antithrombotics in intracranial hemorrahge. Neurocrit Care 24:6–46
Hoffman M, Goldstein JN, Levy JH (2018) The impact of prothrombin complex concentrates when treating DOAC-associated bleeding: a review. Int J Emerg Med 11:1–18
Tomaselli G et al (2020) 2020 ACC expert consensus decision pathway on management of bleeding in patients on oral anticoagulants: a report of the American college of cardiology solution set oversight committee. J Am Coll Cardiol 76(5):594–622
Abraham NS, Barkun AN, Sauer BG et al (2022) American college of gastroenterology-canadian association of gastroenterology clinical practice guideline: management of anticoagulants and antiplatelets during acute gastrointestinal bleeding and the periendoscopic period. Am J Gastroenterol 117(4):542–558
Panos NG, Cook AM, John S et al (2020) Factor Xa inhibitor-related intracranial hemorrhage (FiX-ICH): results from a multicenter, observational cohort receiving prothrombin complex concentrates. Circulation 26(21):1681–1689
Frontera JA, Bhatt P, Lalchan R et al (2020) Cost comparison of andexanet versus prothrombin complex concentrates for direct factor Xa inhibitor reversal after hemorrahge. J Throm Thrombolys 49:121–131
Rowe AS, Dietrich S, Hamilton LA (1995) Analysis of anticoagulation reversal survey (ARES). Hosp Pract 48(3):123–127
Barra ME, Das AS, Hayes BD et al (2020) Evaluation of andexanet alfa and four-factor prothrombin complex concentrate (4F-PCC) for reversal of rivaroxaban- and apixaban-associated intracranial hemorrhages. J Thromb Haemost 18:1637–1647
Ammar AA, Ammar MA, Owusu KA et al (2021) Andexanet alfa versus 4-factor prothrombin complex concentrate for reversal of factor Xa inhibitors in intracranial hemorrhage. Neurocrit Care 35(1):255–261
Vestal ML, Hodulik K, Mando-Vandrick J et al (2022) Andexanet alfa and four-factor prothrombin complex concentrate for reversal of apixaban and rivaroxaban in patients diagnosed with intracranial hemorrhage. J Thromb Thrombolysis 53(1):167–175
Blatchford O, Murray WR, Blatchford M (2000) A risk score to predict need for treatment for upper-gastrointestinal haemorrhage. Lancet 356(9238):1318–1321
Hemphill JC 3rd, Bonovich DC, Besmertis L, Manley GT, Johnston SC (2001) The ICH score: a simple, reliable grading scale for intracerebral hemorrhage. Stroke 32(4):891–897
Lambden S, Laterre PF, Levy MM et al (2019) The SOFA score—development, utility and challenges of accurate assessment in clinical trials. Crit Care 23:374
AstraZeneca. (n.d.) Access & Reimbursement. Andexxa. https://www.andexxa.com/access-reimbursement.html Accessed 3 May 2023
Nederpelt CJ, Naar L, Krijnen P et al (2021) Andexanet alfa or prothrombin complex concentrate for factor Xa inhibitor reversal in acute major bleeding: a systematic review and meta-analysis. Crit Care Med 49(10):e1025–e1036. https://doi.org/10.1097/CCM.0000000000005059
Heckbert SR, Austin TR, Jensen PN et al (2020) Differences by race/ethnicity in the prevalence of clinically detected and monitor-detected atrial fibrillation: MESA. Circ Arrhythm Electrophysiol 13(1):e007698. https://doi.org/10.1161/CIRCEP.119.007698
Author information
Authors and Affiliations
Contributions
JK, MJ, JL, CH, MB, MB, JK were all involved with designing the methods and revision of the manuscript. JK performed data collection and analyzed the data.
Corresponding author
Ethics declarations
Conflicts of interest
JJK, MCJ, JL, CDH, MKB, MEB, JSK declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Keinath, J.J., Lekura, J., Hauser, C.D. et al. Deterioration free discharge comparison of andexanet-alfa and prothrombin complex concentrates (PCC) for reversal of factor Xa inhibitor associated bleeds. J Thromb Thrombolysis 56, 315–322 (2023). https://doi.org/10.1007/s11239-023-02840-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-023-02840-8